Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Tension Pneumothorax
Related Subjects: Asthma |Acute Severe Asthma |Exacerbation of COPD |Pulmonary Embolism |Cardiogenic Pulmonary Oedema |Pneumothorax |Tension Pneumothorax |Respiratory (Chest) infections Pneumonia |Fat embolism |Hyperventilation Syndrome |ARDS |Respiratory Failure |Diabetic Ketoacidosis
🚨 Tension Pneumothorax (TPTX) is a clinical diagnosis – do not wait for radiology. Immediate needle thoracocentesis is lifesaving. When intrapleural pressure rises like a balloon 🎈, venous return is impaired → cardiac output collapses → death if untreated. 🪡 Pop the balloon with a needle and let the air out!
🫁 About
- Needs urgent decompression with a needle → “hiss of air” confirms diagnosis.
- If no tension present, little harm done: remove needle and proceed to CXR for other causes.
⚙️ Aetiology
- Air enters pleural space but cannot escape (valve effect).
- If intrathoracic pressure > diastolic filling pressure → cardiac output falls → shock and death.
🧾 Causes
- 💥 Trauma
- Penetrating (stab wound, rib fracture)
- Blunt trauma (e.g. RTA)
- ⚕️ Iatrogenic
- Central line or pacing wire insertion
- Lung biopsy, bronchoscopy
- Percutaneous tracheostomy
- Positive pressure ventilation (barotrauma)
- CPR, intercostal nerve block, thoracentesis
- 🌊 Non-Iatrogenic
- Diving, flying, rib fractures
- 🌀 Atraumatic
- Primary (young, tall, thin, unknown cause)
- Secondary (underlying lung disease e.g. COPD, fibrosis)
👩⚕️ Clinical Features
- Seen after chest trauma, procedures (e.g. CVC insertion), or on ventilation.
- Subcutaneous emphysema possible.
- Cardinal signs: tachycardia ❤️🔥, cyanosis, anxiety, rapid deterioration.
- Raised JVP, absent breath sounds on affected side, hyper-resonant chest.
- Hypotension = late and deadly sign ☠️.
- Obvious chest wound may be present.
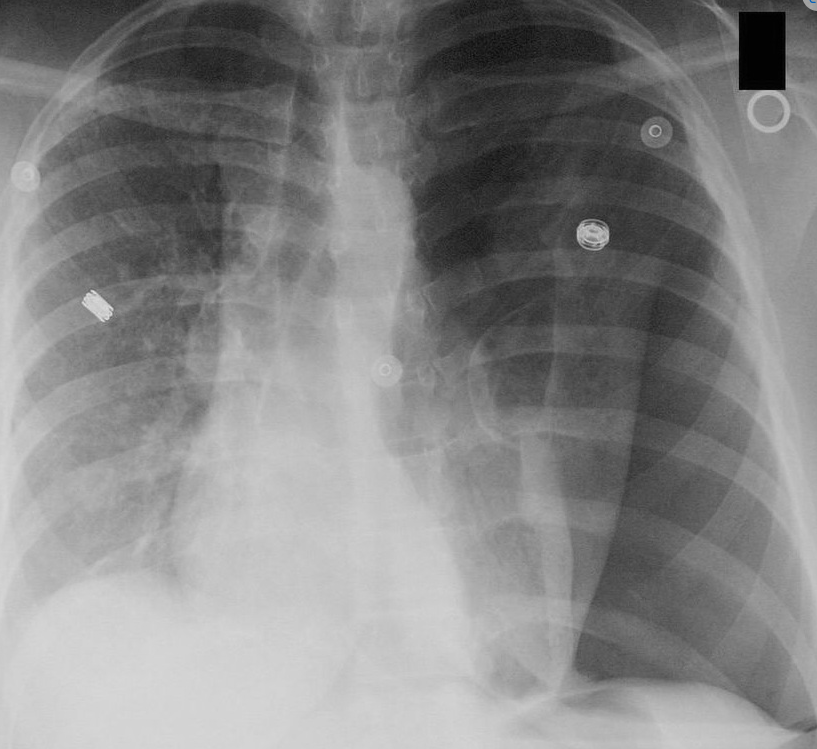
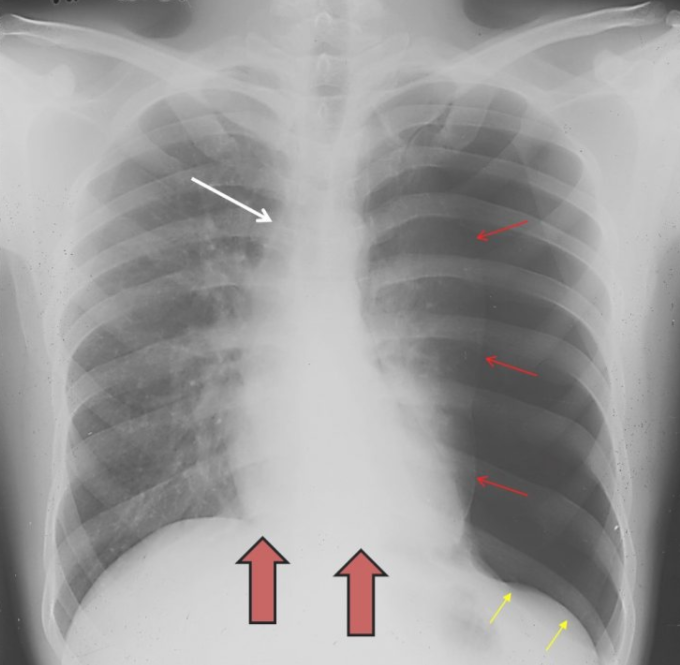
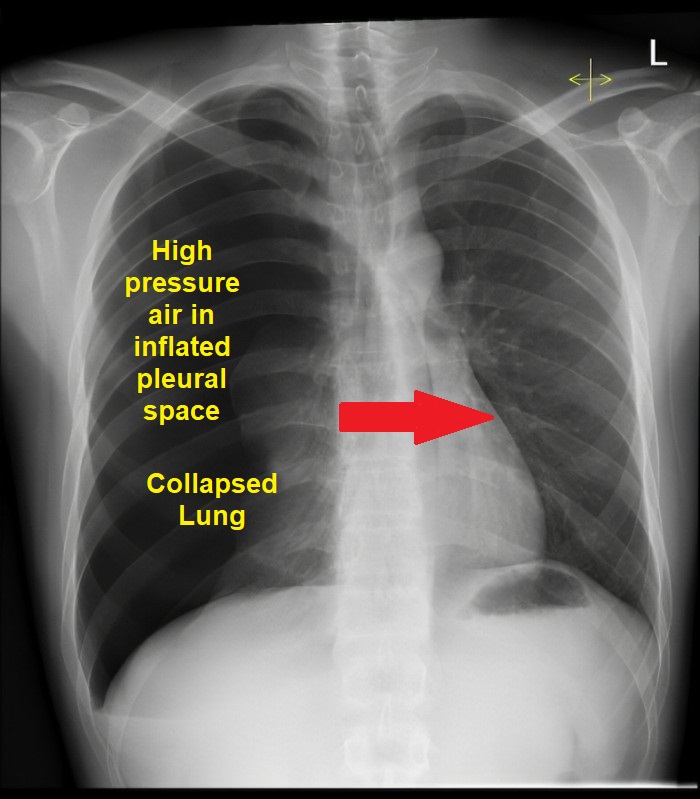
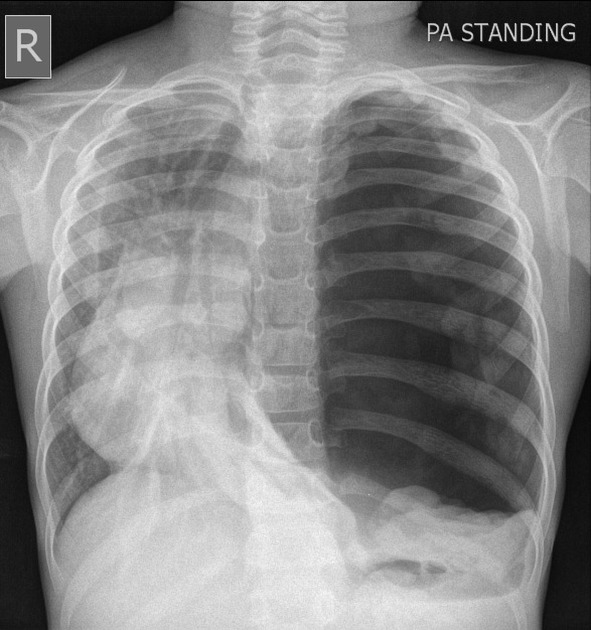
📸 Imaging
Patients often too unstable for CXR, but classic findings include:
- Thin vertical line of visceral pleura.
- Loss of lung markings distal to line.
- Complete ipsilateral lung collapse.
- Mediastinal shift away from pneumothorax.
- Tracheal deviation to contralateral side.
- Flattened hemidiaphragm.
- Subcutaneous emphysema.
🔍 Ultrasound (94% sensitive, 100% specific): absent lung sliding, “lung point” seen.
🛠️ Management
- ⚡ Immediate ABCDE approach: Sit up, 15L/min O₂ via NRB mask.
- 💉 If in extremis: Immediate needle decompression
- Classically: 2nd intercostal space, midclavicular line.
- Alternative (preferred in many UK hospitals): 4th/5th ICS anterior axillary line (safe triangle).
- Listen for hiss of escaping air, leave cannula in situ.
- 🩺 Chest drain insertion (definitive): placed in “safe triangle”. Do not wait for imaging.
- If no hiss after cannula → consider malposition or alternate diagnosis.
- Monitor for recurrence if drain blocks or dislodges.
Cases — Tension Pneumothorax
- Case 1 — Trauma setting 🚑: A 24-year-old motorcyclist arrives after a high-speed collision. He is agitated, tachypnoeic (RR 36), with absent breath sounds and hyper-resonance on the left. Trachea is deviated to the right, JVP is raised, and SpO₂ 78% on high-flow oxygen. Immediate needle decompression is performed in the 2nd intercostal space, mid-clavicular line, followed by chest drain insertion.
- Case 2 — Iatrogenic setting 💉: A 68-year-old man with COPD develops acute pleuritic chest pain and collapse during subclavian central line insertion. On exam: hypotension, distended neck veins, trachea deviated away from the affected side, and absent breath sounds. Diagnosis of iatrogenic tension pneumothorax is made; rapid decompression with a large-bore cannula is lifesaving.
- Case 3 — Cardiac Arrest 🫀: A 32-year-old ventilated patient in ITU suddenly deteriorates and becomes pulseless (PEA arrest). Bagging is increasingly difficult with high airway pressures. Examination reveals distended neck veins, absent right-sided breath sounds, and tracheal deviation. Immediate bilateral needle decompression is performed as part of ALS reversible causes ("H’s & T’s"), restoring output before chest drains are placed.
Teaching Point 🩺: Tension pneumothorax is a clinical diagnosis — do not delay for chest X-ray. Progressive intrapleural pressure causes mediastinal shift and obstructive shock. Needle decompression is life-saving, but definitive treatment is chest drain insertion.
Categories
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology