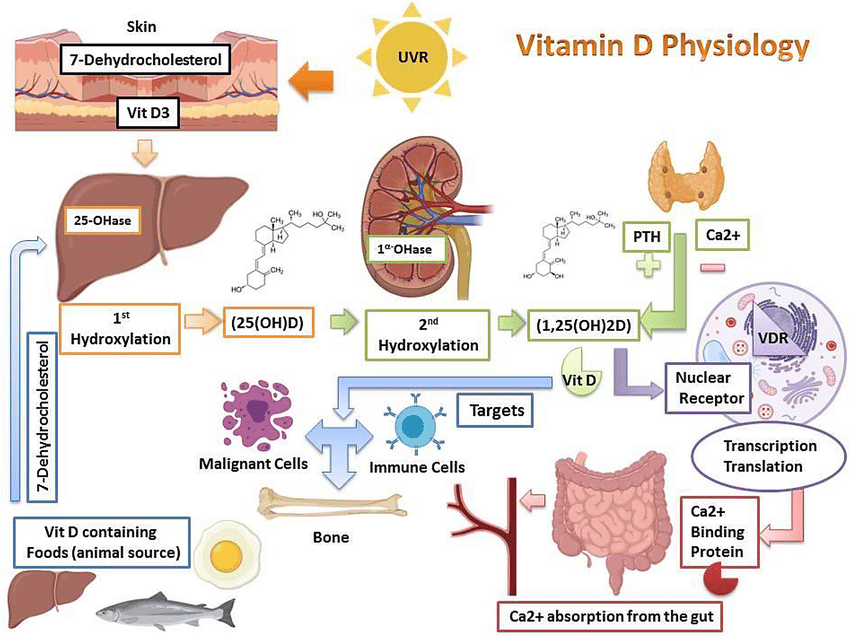
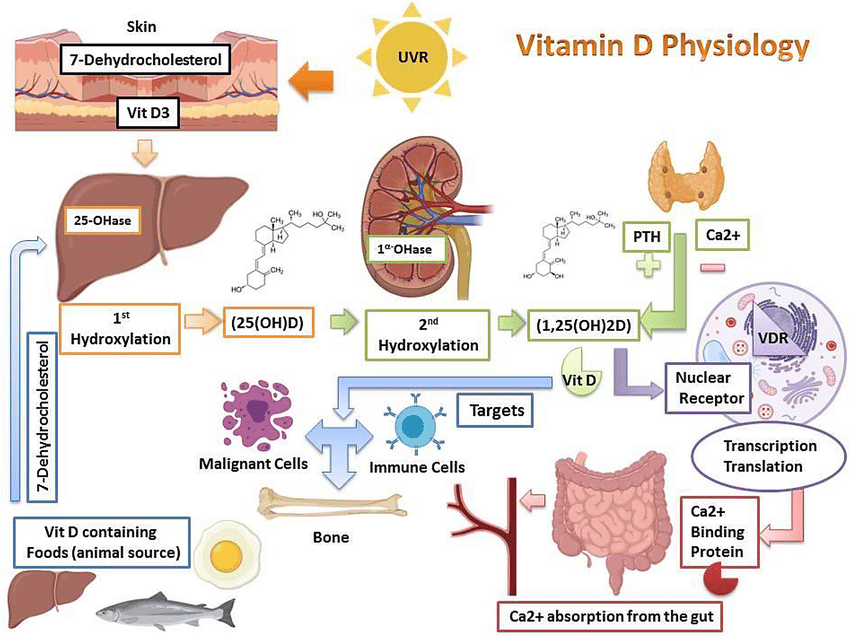
Vitamin D Physiology
Vitamin D is a fat-soluble vitamin that behaves like a steroid hormone.
It is vital for calcium and phosphate homeostasis, bone mineralisation, and muscle function.
The two main forms are cholecalciferol (D₃) from sunlight/animal sources and ergocalciferol (D₂) from plants.
☀️ Physiology & Metabolism
- UV-B light converts 7-dehydrocholesterol in skin → vitamin D₃.
- Liver: 25-hydroxylation → 25-hydroxyvitamin D (25(OH)D).
- Kidney: 1-α-hydroxylation → active 1,25-dihydroxyvitamin D (calcitriol).
- Enhances intestinal Ca²⁺ and PO₄³⁻ absorption; supports bone mineralisation.
- Downregulated by high phosphate or fibroblast growth factor-23 (FGF-23).
🇬🇧 UK Context
- Effective skin synthesis occurs only between April–September.
- From October–March, UV-B levels in the UK are too low → dietary/supplemental intake required.
- Deficiency common in elderly, dark-skinned, veiled, institutionalised, and obese individuals.
📊 Definitions (NICE / SACN)
| Status | 25(OH)D Level | Interpretation |
|---|
| Deficient | < 25 nmol/L | Associated with osteomalacia/rickets |
| Insufficient | 25–50 nmol/L | May be inadequate for some individuals |
| Sufficient | > 50 nmol/L | Adequate for bone health |
🧍♂️ Clinical Features of Deficiency
- Adults: Bone pain, proximal myopathy, fragility fractures, fatigue.
- Children: Rickets — bowing of legs, delayed milestones, craniotabes.
- Biochemical pattern: ↓ Ca²⁺, ↓ PO₄³⁻, ↑ ALP, ↑ PTH (secondary hyperparathyroidism).
🔬 Investigations
- Primary test: Serum 25(OH)D (not calcitriol).
- Also check calcium, phosphate, ALP, ± PTH and renal function.
- Testing indicated only if symptomatic or before starting potent anti-resorptive therapy.
💊 Management & Supplementation
- Prevention (Public Health England):
All adults and children > 4 yrs should take 10 µg = 400 IU daily Oct–Mar.
- Year-round supplementation: For those with dark skin, veiling, housebound, or little sun exposure.
- Treatment of deficiency:
Loading dose total ≈ 300 000 IU (e.g. 50 000 IU weekly × 6 weeks) → maintenance 800–2000 IU daily.
- Ensure sufficiency before anti-resorptive therapy (e.g., zoledronate, denosumab).
⚠️ Vitamin D Toxicity
- Excess supplementation → hypercalcaemia, nausea, renal stones, confusion.
- Monitor calcium and renal function in those on high-dose or long-term therapy.
🧠 Teaching Pearls
- Think vitamin D deficiency in older patients with falls or proximal weakness.
- Do not routinely test in healthy people — encourage prevention instead.
- Understand the physiology: Skin → Liver → Kidney → Bone — this explains why CKD, liver disease or immobility predispose to deficiency.
- Simple intervention, major benefit: low-cost, low-risk, high-impact in frailty and fracture prevention.
📋 Summary Table
| Aspect | Key Point |
|---|
| Deficiency threshold | < 25 nmol/L (UK) |
| Routine screening | No — reserve for symptomatic or high-risk |
| Standard supplement | 10 µg = 400 IU daily (Oct–Mar) |
| Treatment regimen | Loading ≈ 300 000 IU → maintenance 800–2000 IU/day |
| Key effect | ↑ Ca²⁺ and PO₄³⁻ absorption → bone mineralisation |
| Toxicity | Hypercalcaemia, nephrolithiasis, confusion |
🩺 Summary for Practice
In UK medicine, vitamin D deficiency is common yet easily corrected.
Always check in patients with bone pain, proximal weakness, fragility fractures, malabsorption, or before giving anti-resorptive therapy.
Focus on prevention, seasonal awareness, and practical dosing.