| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Anatomy and Physiology of the Lungs
Related Subjects: |Anatomy and Physiology of the Lungs |Anatomy and Physiology of the Heart |Coronary Anatomy and Physiology |Cardiac Embryology |Gastrointestinal tract Physiology |Autonomic Nervous System
🫁 Anatomy and Physiology of the Lungs — In Depth (Makindo)
The lungs are paired, elastic organs designed for gas exchange and acid–base homeostasis. They deliver oxygen to the bloodstream for cellular metabolism and remove carbon dioxide (CO2), the key volatile acid load. Efficient respiration requires the integrated performance of ventilation (airflow), perfusion (pulmonary blood flow), and diffusion (gas transfer across the alveolar–capillary membrane), all coordinated by neural and chemical control systems.
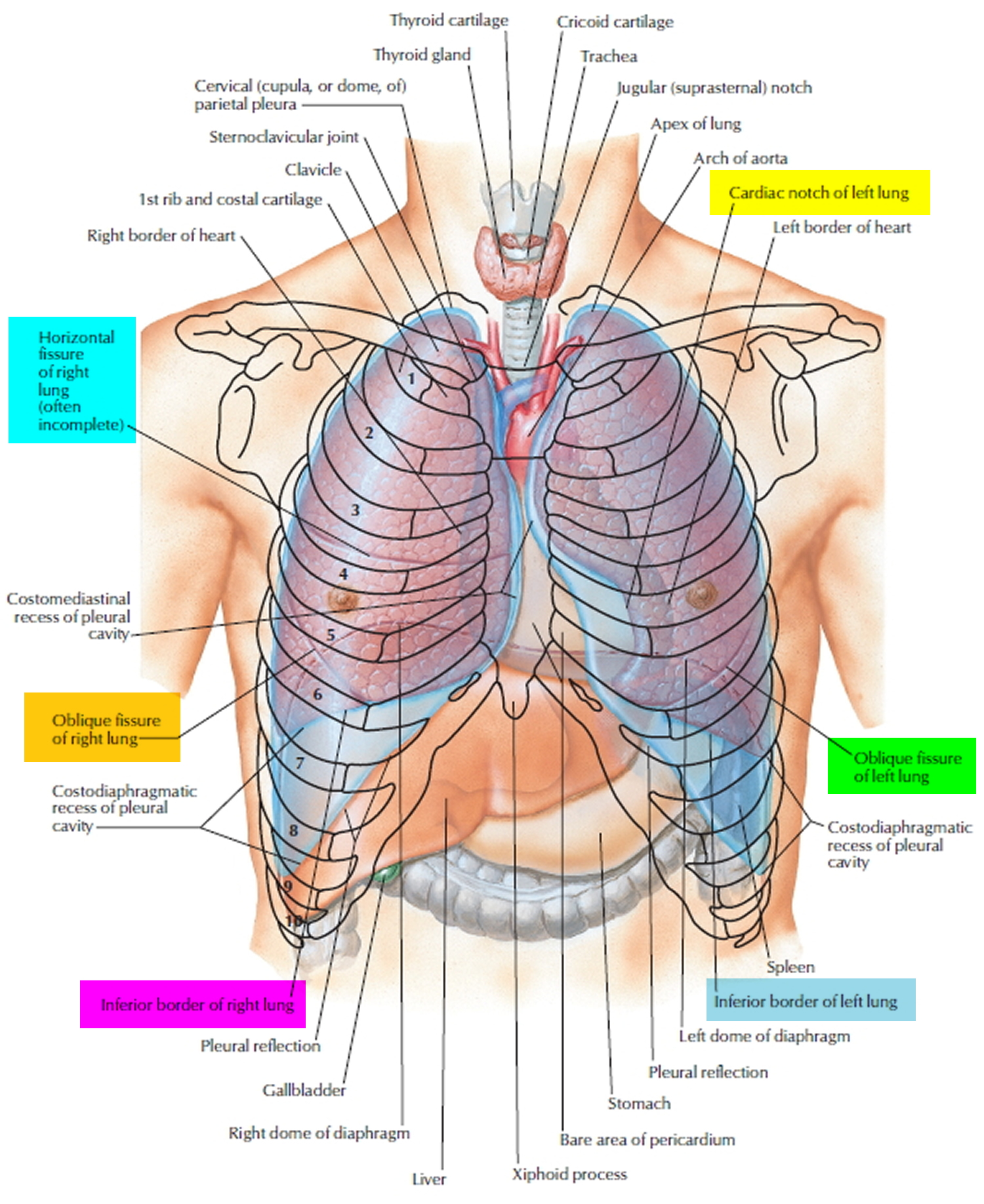
🏗️ 1) Gross Anatomy and Organisation
- Position: Each lung occupies a pleural cavity either side of the mediastinum, resting on the diaphragm.
- Apex: Projects above the 1st rib into the root of the neck.
- Base: Diaphragmatic surface; moves with respiration.
- Surfaces: Costal (ribs), mediastinal (hilum/root), diaphragmatic (base).
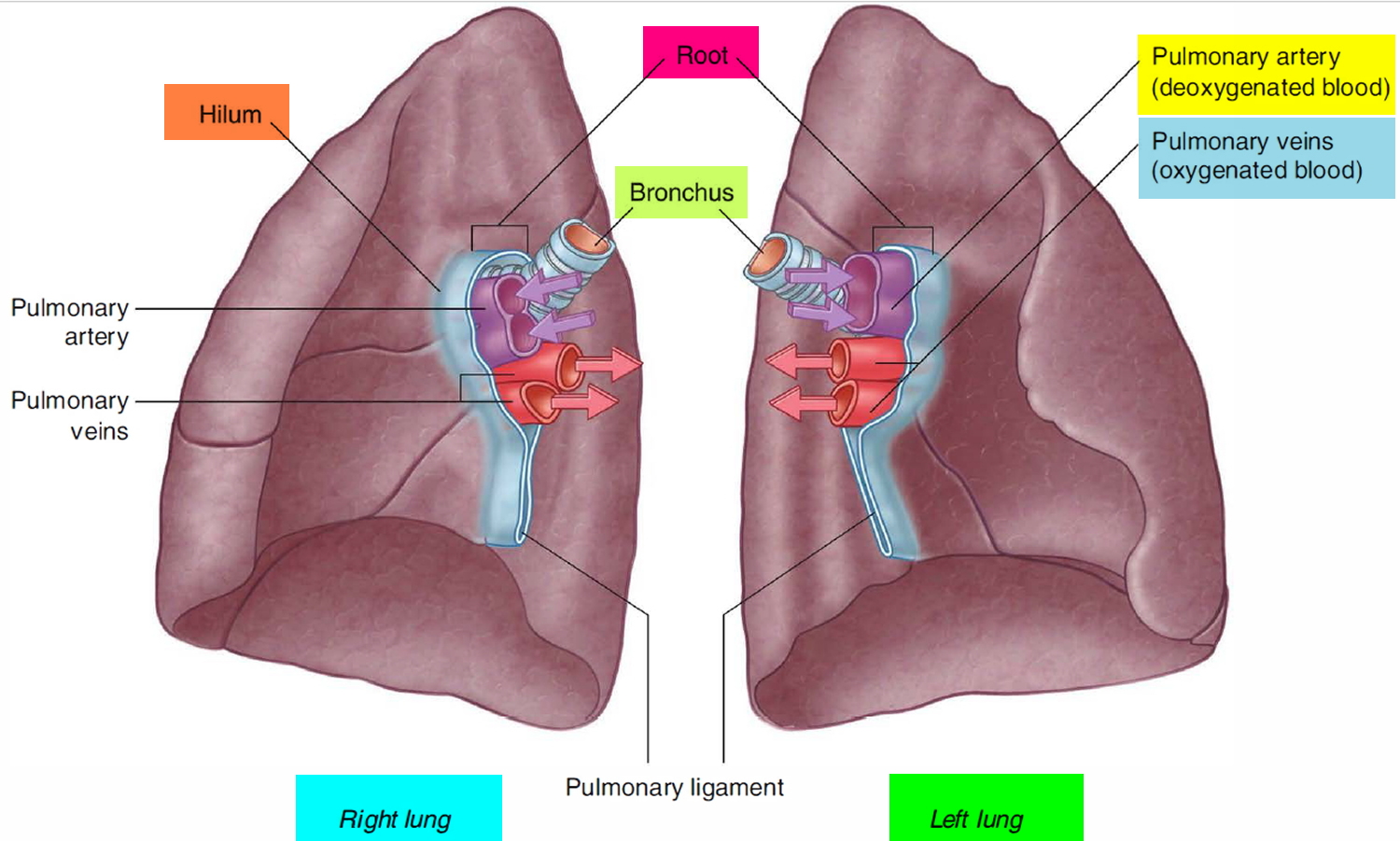
- Hilum (root): Main bronchus, pulmonary artery, pulmonary veins, bronchial vessels, lymphatics, autonomic nerves.
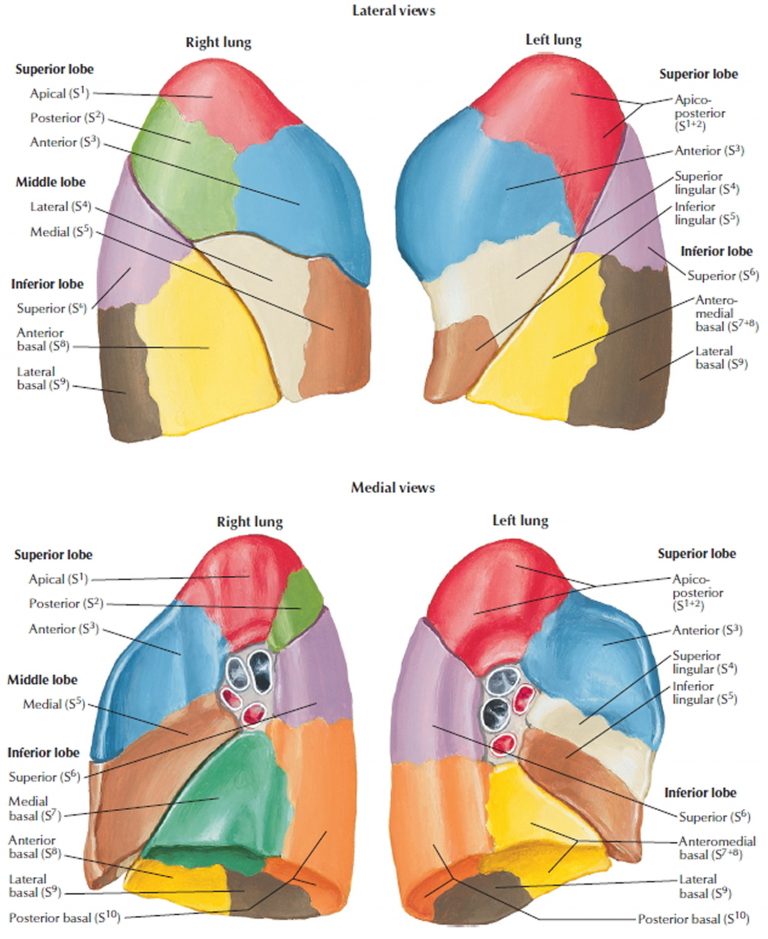
🧩 Lobes, Fissures, and Bronchopulmonary Segments
- Right lung: 3 lobes (upper, middle, lower) with horizontal and oblique fissures.
- Left lung: 2 lobes (upper, lower) with lingula (functional analogue of the right middle lobe).
- Bronchopulmonary segments: Discrete units each supplied by a segmental bronchus and a segmental pulmonary artery.
📌 Clinical: Segments can often be surgically removed (segmentectomy) with relatively preserved surrounding lung.
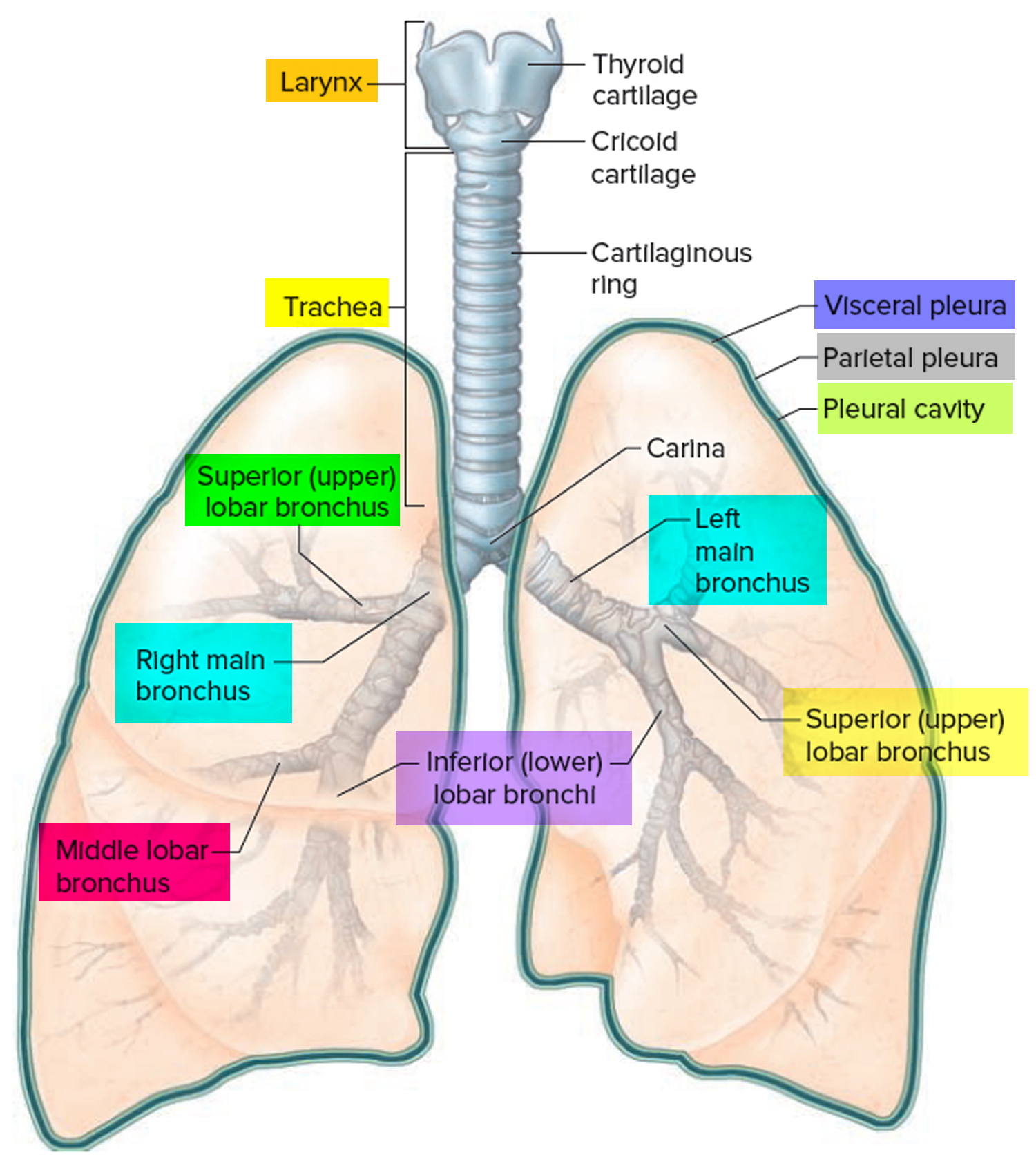
🫧 2) Pleura and Pleural Space
- Visceral pleura: Adherent to lung surface and fissures.
- Parietal pleura: Lines thoracic wall, diaphragm, mediastinum.
- Pleural space: Potential space with a thin lubricating fluid layer that reduces friction and “couples” lungs to chest wall movement.
- Intrapleural pressure: Normally negative at rest and becomes more negative during inspiration → helps keep lungs expanded.
📌 Clinical: In pneumothorax, the pleural seal is broken → intrapleural pressure equalises with atmospheric pressure → lung recoils and partially/fully collapses. In tension pneumothorax, a one-way valve mechanism increases intrathoracic pressure, impairs venous return, and can cause obstructive shock.
🌳 3) The Airway Tree — Conducting vs Respiratory Zones
- Conducting zone: Nose → pharynx → larynx → trachea → bronchi → bronchioles → terminal bronchioles.
Functions: warms, humidifies, filters air; provides low-resistance conduit. - Respiratory zone: respiratory bronchioles → alveolar ducts → alveolar sacs/alveoli.
Function: gas exchange.
🔎 Trachea and Main Bronchi
- Trachea: C-shaped cartilage rings with posterior trachealis muscle; bifurcates at the carina (T4/5).
- Right main bronchus: Wider, shorter, more vertical → aspiration/foreign bodies more commonly enter the right lung.
- Left main bronchus: Longer, more oblique; passes beneath the aortic arch.
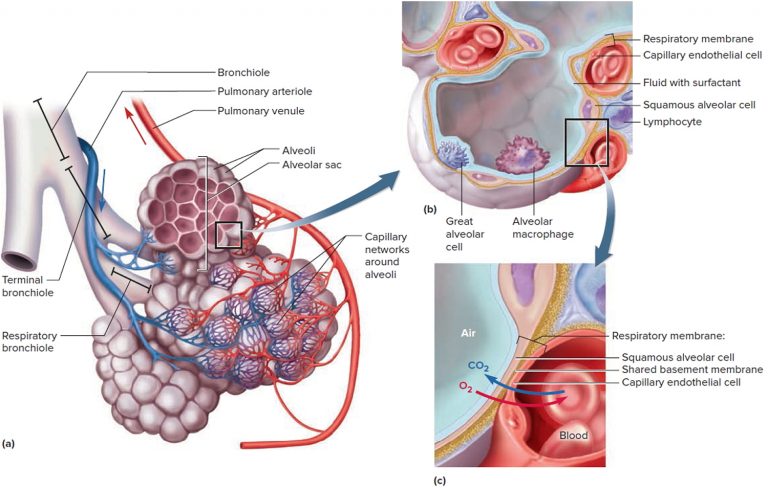
🧬 4) Microanatomy of the Alveoli
- Alveoli: ~300 million microscopic sacs; total surface area ~50–70 m² (adult).
- Type I pneumocytes: Thin squamous cells forming most of the gas-exchange surface.
- Type II pneumocytes: Produce surfactant and act as progenitors for alveolar epithelium repair.
- Alveolar macrophages: “Dust cells” providing immune surveillance and particle clearance.
- Alveolar–capillary membrane: Type I cell + fused basement membrane + capillary endothelium → ultra-thin diffusion barrier.
🫧 Surfactant (why it matters)
Surfactant reduces surface tension and stabilises alveoli (Laplace’s law: P = 2T/r), preventing small alveoli collapsing into larger ones and lowering the work of breathing. Deficiency (e.g., prematurity) causes neonatal respiratory distress syndrome with atelectasis and stiff lungs.
🩸 5) Pulmonary and Bronchial Circulations
- Pulmonary circulation: Right ventricle → pulmonary arteries → alveolar capillaries → pulmonary veins → left atrium.
Low-pressure, high-flow system specialised for gas exchange. - Bronchial circulation: Systemic arterial supply (thoracic aorta) to airways/supporting tissues.
Venous drainage partly returns to pulmonary veins → small physiological shunt.
📌 Clinical: A pulmonary embolism creates ventilated but under-perfused lung (↑ dead space). Chronic alveolar hypoxia triggers hypoxic pulmonary vasoconstriction, which can raise pulmonary vascular resistance and contribute to pulmonary hypertension and cor pulmonale.
⚙️ 6) Mechanics of Breathing
- Inspiration: Active — primarily diaphragm + external intercostals → thoracic volume ↑ → alveolar pressure ↓ → air flows in.
- Expiration: Passive at rest — elastic recoil. Active during exertion via internal intercostals + abdominal muscles.
- Compliance (ΔV/ΔP): Lung “stretchiness”.
↓ in fibrosis/ARDS/pneumonia (stiff), ↑ in emphysema (floppy). - Elastic recoil: Drives passive expiration; reduced recoil in emphysema → air trapping.
🧮 Airway Resistance (Why Small Changes Matter)
- In health, much resistance is in medium/large bronchi; small airways become important in disease.
- Poiseuille’s law: resistance ∝ 1/radius4 → small radius reduction causes a large rise in resistance (key in asthma).
📦 7) Lung Volumes, Capacities, and Dead Space
- Tidal volume (TV): ~500 mL (adult at rest).
- IRV: extra inspired beyond TV.
- ERV: extra expired beyond TV.
- Residual volume (RV): air remaining after maximal expiration (prevents collapse).
- Vital capacity (VC): IRV + TV + ERV.
- Total lung capacity (TLC): VC + RV.
- Functional residual capacity (FRC): end-expiratory volume (lung recoil inward vs chest wall recoil outward).
- Dead space: air not participating in gas exchange (anatomical + alveolar).
📌 Clinical: FRC falls with general anaesthesia and obesity → atelectasis risk. PEEP can help recruit alveoli and improve oxygenation (but excessive PEEP may reduce venous return).
🌬️ 8) Gas Exchange (Diffusion) and V/Q Matching
- Diffusion: Fick’s law — transfer ∝ surface area × pressure gradient / thickness.
- Diffusion limitation: fibrosis/oedema (↑ thickness) or emphysema (↓ area) → worsens oxygenation.
- V/Q matching: Efficient exchange requires matching airflow to blood flow across the lung.
🧭 Regional V/Q Differences
- Apex: High V/Q (perfusion falls more than ventilation) → higher alveolar O2, lower CO2.
- Base: Low V/Q → lower O2, higher CO2.
- Overall normal V/Q: ~0.8.
📌 Key concept: Shunt = perfused but not ventilated (pneumonia, atelectasis) → hypoxaemia responds poorly to oxygen. Dead space = ventilated but not perfused (PE) → increased ventilatory requirement and impaired CO2 clearance.
🩸 9) Oxygen and CO2 Transport
🟦 Oxygen transport
- ~98% bound to haemoglobin; 1 g Hb binds ~1.34 mL O2.
- Sigmoid dissociation curve due to cooperative binding.
- Right shift (easier tissue unloading): ↑ CO2, ↑ temperature, ↓ pH (Bohr effect), ↑ 2,3-BPG.
🟩 Carbon dioxide transport
- ~70% as bicarbonate via carbonic anhydrase.
- ~20% as carbamino-Hb; ~10% dissolved.
- Haldane effect: deoxygenated Hb binds more CO2 → improves CO2 carriage from tissues.
🧠 10) Control of Ventilation
- Medulla: generates respiratory rhythm; drives inspiratory and expiratory motor output.
- Pons: modulates pattern and smooths transitions.
- Central chemoreceptors: primarily sense CO2 via CSF pH (major ventilatory driver).
- Peripheral chemoreceptors: carotid/aortic bodies respond strongly to ↓ PaO2 (<60 mmHg / ~8 kPa), also ↑ CO2 and ↓ pH.
- Mechanoreceptors: stretch receptors limit overinflation (more prominent in infants).
- Higher centres: voluntary control (speech, breath-holding), emotion/pain/fever effects.
📌 Clinical: In some chronic hypercapnic COPD phenotypes, CO2 responsiveness is blunted. High-flow oxygen can worsen hypercapnia mainly via V/Q mismatch and loss of hypoxic pulmonary vasoconstriction (the “hypoxic drive” effect is smaller but can contribute).
🛡️ 11) Lung Defence Mechanisms
- Mucociliary escalator: cilia + mucus trap particles and move them upwards to be swallowed.
- Cough reflex: clears irritants and secretions from the lower airway.
- Alveolar macrophages: phagocytose particles/pathogens in distal airspaces.
- Mucosal immunity: IgA and innate immune factors protect airway surfaces.
📌 Clinical: Smoking impairs ciliary function and increases mucus → infection risk, chronic bronchitis, and impaired clearance.
🩺 12) Clinical Correlations (Physiology → Bedside)
- Asthma: reversible bronchoconstriction + inflammation → ↑ resistance, wheeze, variable peak flow.
- COPD: fixed airflow limitation; emphysema reduces recoil → air trapping and ↑ FRC; chronic bronchitis increases mucus and infection risk.
- Pulmonary fibrosis: ↓ compliance + diffusion limitation → rapid shallow breathing; ↓ DLCO.
- ARDS: diffuse alveolar damage → non-cardiogenic oedema and “stiff” lungs; requires PEEP and lung-protective ventilation.
- PE: ↑ dead space; hypoxaemia from V/Q mismatch.
- Pneumonia/atelectasis: shunt physiology → hypoxaemia less responsive to oxygen.
📊 Summary (High-Yield Integration)
Lung performance is built on ventilation, diffusion, and perfusion, with V/Q matching as the key integrator. Mechanical properties (compliance, recoil, resistance) determine the work of breathing, while haemoglobin chemistry enables efficient oxygen delivery and CO2 transport. When oxygenation fails, systematically ask: is the problem airflow (obstruction), alveoli (collapse/fill), blood flow (PE/shock), or membrane (fibrosis/oedema)?
💡 Teaching Tip: Think “pump + filter + controller”: pump = diaphragm/chest wall mechanics; filter = alveolar–capillary unit; controller = brainstem chemoreflexes. Most respiratory pathology is explainable by which component breaks and how that distorts V/Q.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
