| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Diabetes Mellitus Type 1 and DKA (children)
Related Subjects:Sick Neonate |APGAR Scoring |Approach to Assessing Sick Child |Sick Child with Acute Gastroenteritis |Sick Child with Respiratory Distress |Sick child Diabetes Mellitus Type 1 and DKA
💉 Type 1 Diabetes Mellitus (T1DM) is a chronic autoimmune condition caused by destruction of pancreatic β-cells ➝ absolute insulin deficiency ➝ persistent hyperglycaemia. Around 25% of children present in Diabetic Ketoacidosis (DKA) at first diagnosis 🚨.
📖 About
- Autoimmune destruction of insulin-producing β-cells in the pancreas.
- Usually presents in childhood or adolescence, though can occur at any age.
- Requires lifelong insulin therapy.
🧬 Aetiology
- Insulin produced by islets of Langerhans (β-cells).
- Autoantibodies (e.g. anti-GAD, anti-islet cell) target β-cells, leading to progressive destruction.
- Genetic predisposition (HLA types), with environmental triggers (viral infections, toxins) thought to play a role.
🩺 Clinical Features
- Classic triad: Polyuria 🚽, Polydipsia 💧, Weight loss ⚖️.
- Vomiting, lethargy, and dehydration in severe cases.
- Nocturnal enuresis (bedwetting) may be a presenting sign.
- Recurrent candida infections can be a clue.
- 25% present in DKA (abdominal pain, vomiting, Kussmaul breathing, acetone breath).
🧪 Investigations
- Blood glucose: Random ≥11.1 mmol/L with symptoms is diagnostic.
- Ketones: Urine or blood ketones (raised in DKA).
- HbA1c: Chronic hyperglycaemia marker (≥48 mmol/mol).
- Blood gas: Metabolic acidosis in DKA (pH <7.3, HCO₃⁻ <15).
- Autoantibodies: Anti-GAD, anti-islet cell (autoimmune confirmation).
- Screen for coeliac and thyroid disease (autoimmune associations).
💊 General Management of T1DM
- Education 👨👩👧: Self-monitoring of glucose, insulin administration, sick-day rules.
- Insulin therapy:
- Basal-bolus: Long-acting insulin once daily + rapid insulin with meals.
- Pump therapy: Subcutaneous infusion in selected children; risks: infection, pump failure.
- Diet & lifestyle: Carbohydrate counting, healthy diet, regular exercise.
🚨 Paediatric Diabetic Ketoacidosis (DKA) Management
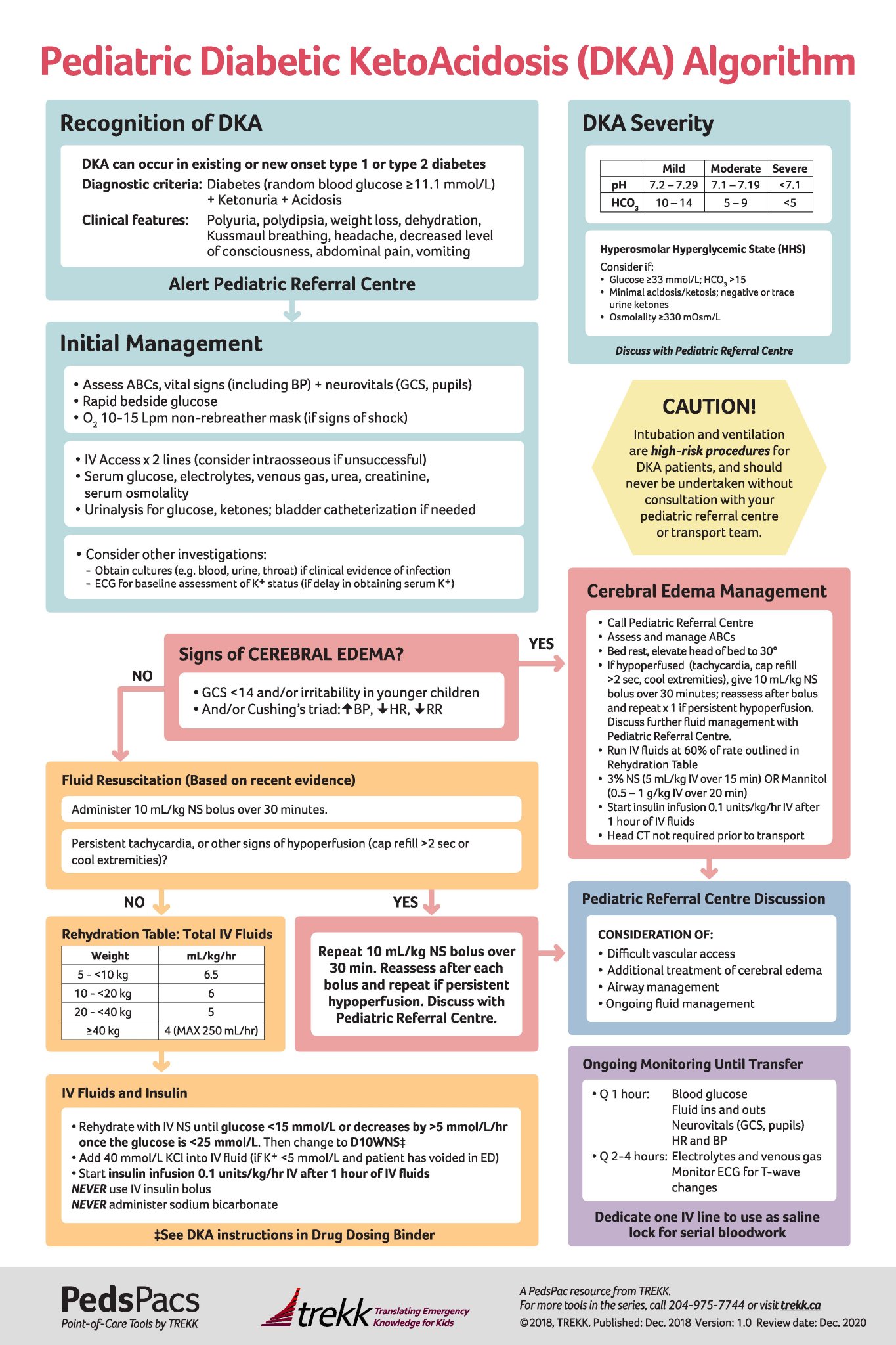
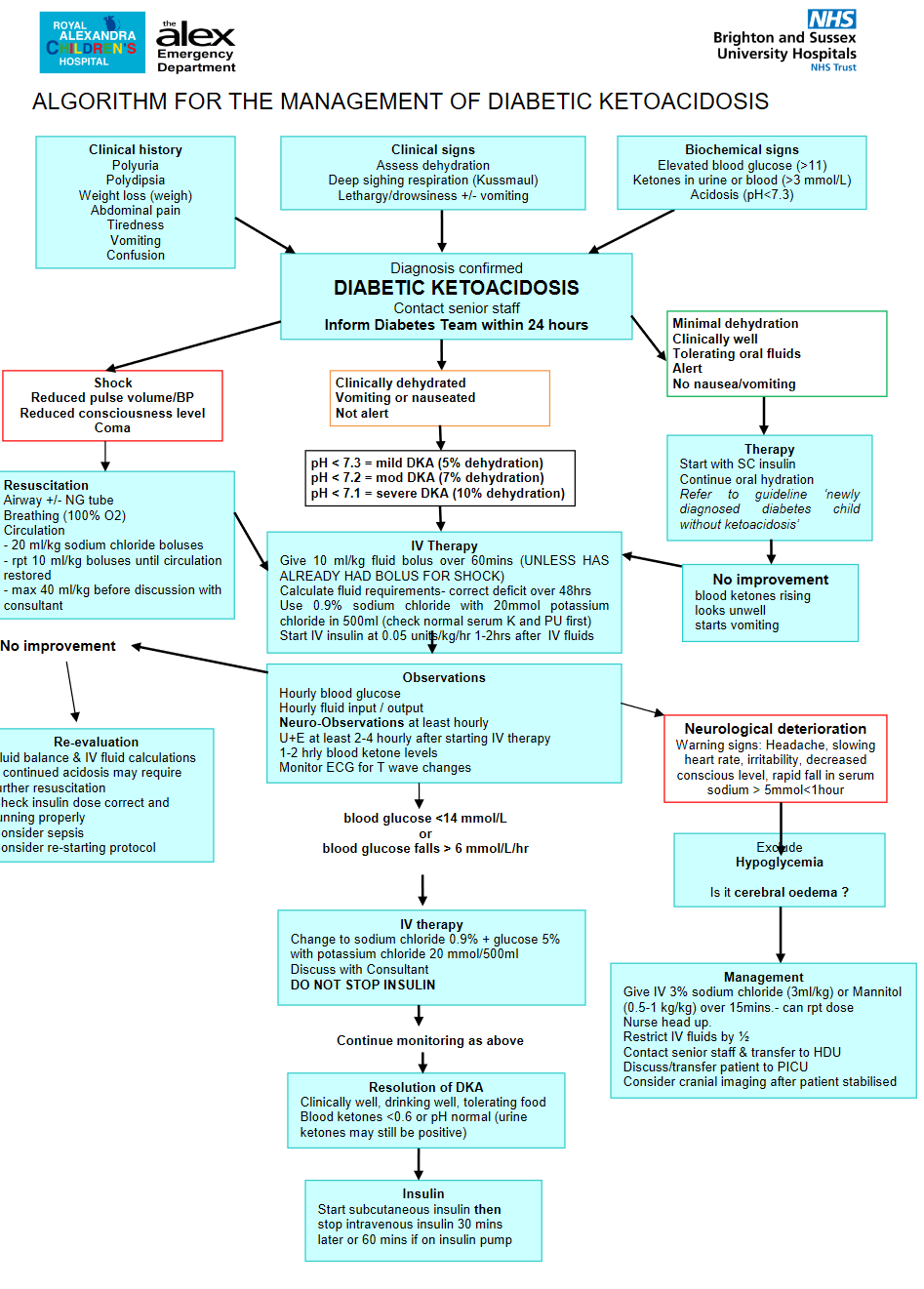
⚠️ Cerebral oedema is the most feared complication in paediatric DKA. Always monitor neurological status closely. Treat promptly with mannitol 20% (2.5 mL/kg IV over 10 min) or 3% hypertonic saline (5 mL/kg IV over 10–15 min) if suspected.
🩺 Stepwise Management
- 1️⃣ ABC & Monitoring
- Airway, Breathing, Circulation ➝ stabilise.
- Continuous monitoring: HR, BP, SpO₂, GCS, neuro obs hourly.
- Cardiac monitor (risk of arrhythmia if K⁺ deranged).
- 2️⃣ IV Access & Bloods
- Venous gas (pH, bicarbonate, ketones).
- FBC, U&E, glucose, lactate.
- Urinalysis for ketones.
- 3️⃣ Fluids 💧
- Correct dehydration slowly over 48 h (avoid cerebral oedema).
- Use 0.9% saline ± 5% dextrose when BG <14 mmol/L.
- Resus if shocked: 10 mL/kg 0.9% saline over 10–15 min (repeat once if needed).
- 4️⃣ Insulin 💉
- Start 1–2 h after fluids have begun.
- Continuous IV infusion at 0.05–0.1 units/kg/hr.
- Aim: fall in glucose 2–5 mmol/L/hr.
- 5️⃣ Potassium ⚡
- Total body K⁺ depleted even if serum appears normal/high.
- Add KCl once child is voiding and serum K⁺ <6 mmol/L.
- Typical: 20 mmol KCl per 500 mL bag.
- 6️⃣ Ongoing Care
- Hourly BG; 2–4 hourly VBG & electrolytes.
- Strict fluid balance (catheterise if necessary).
- Watch for headache, bradycardia, ↓GCS ➝ suspect cerebral oedema.
- 7️⃣ Transition to SC Insulin
- When ketones cleared, child well, eating & drinking.
- Overlap IV infusion with first SC dose by 30–60 min.
📚 References
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
