| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Fibromuscular Dysplasia
Related Subjects:Migraine |Basilar Migraine |Takayasu arteritis (pulseless disease) |Fibromuscular Dysplasia
⚠️ Fibromuscular Dysplasia (FMD) can cause four vascular changes: stenosis, aneurysm, dissection, or occlusion. Always consider in young stroke patients or those with refractory hypertension.
🧠 Introduction
- FMD is an idiopathic, non-inflammatory, and non-atherosclerotic disease of small- and medium-sized arteries.
- It leads to segmental arterial abnormalities affecting flow and structure.
- Most often affects the renal arteries and distal extracranial carotid arteries, but may involve multiple vascular beds.
- More common in young and middle-aged females (female:male ≈ 3:1).
- Accounts for a proportion of childhood strokes and young-onset renovascular hypertension.
🔍 Aetiology
- Found in ≈1% of carotid arteries at post-mortem studies.
- Segmental in nature: alternating areas of stenosis and dilation.
- Does not arise from atherosclerosis or vasculitis.
- Consider in ischaemic stroke or saccular aneurysms (with or without subarachnoid haemorrhage).
📑 Classification
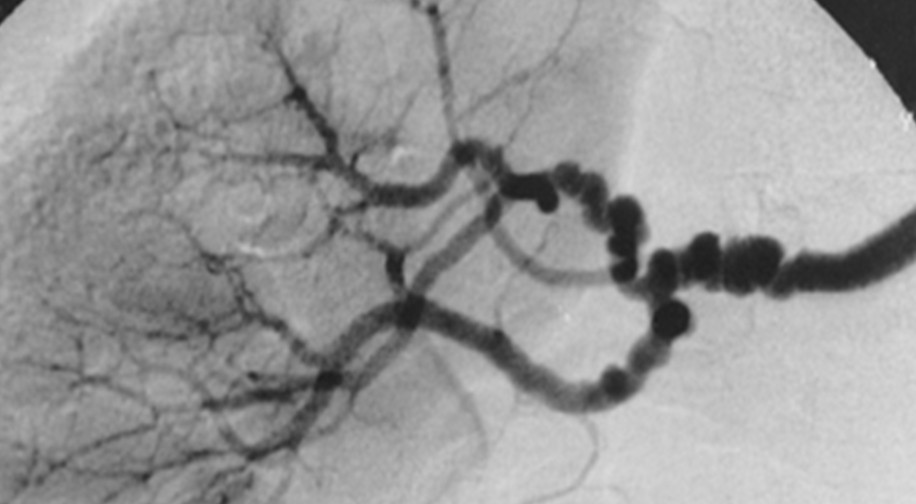
- 💢 Medial fibroplasia (≈80%) – Most common. Classic “string-of-beads” appearance on angiography. Multiple webs → stenosis with post-stenotic dilatation. Aneurysms frequent.
- 🧱 Intimal fibroplasia (≈10%) – Collagen deposition in intima. Appears as long tubular stenosis or concentric band-like narrowing.
- 👧 Perimedial fibroplasia (<10%) – Seen in young girls (5–15 years). Often presents with hypertension and renal dysfunction.
- 🔬 Medial hyperplasia (<1%) – Only confirmed pathologically.
- 🧩 Adventitial fibroplasia (<5%) – Seen on intravascular ultrasound (IVUS); angiography mimics intimal disease.
💡 Clinical Features
- Stroke or TIA due to carotid/vertebrobasilar infarction.
- Carotid/vertebral dissection causing headache, neck pain, or stroke.
- Renal artery stenosis → refractory hypertension.
- Carotid stenosis (with or without stroke).
- Spontaneous coronary artery dissection (SCAD) (link).
- Rare: pulmonary artery involvement.
- May present with subarachnoid haemorrhage from aneurysm rupture.
🧪 Investigations
- Bloods: FBC, U&E, creatinine (renal function).
- CT/MRI Brain: To detect infarction or SAH.
- Angiography (CTA / MRA / DSA): Shows stenosis with “string-of-beads”, dissections, or aneurysms.
- Histology (post-mortem/biopsy): Collagen deposition in intima/media, thinned media with beading.
- No validated genetic/ante-mortem biomarkers currently available.
🩺 Management
- 🚑 Ischaemic stroke: Follow standard stroke protocols (antiplatelets, BP control).
- 🩹 Dissections: Managed with antiplatelets short/long term.
- 🩻 Renal artery stenosis: May require percutaneous intervention or surgery.
- 💊 Hypertension: Treat with antihypertensive drugs.
- 🔁 Long-term follow-up with vascular imaging as disease can recur or progress.
📚 References & Further Reading
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
