| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Immune response
Related Subjects: |Major Histocompatibility complex |Immune response |Complement |Opsonisation |Toll-like Receptors (TLRs) |Immunoglobulins |Immunology |Antigen presenting cells |T lymphocytes |Beta-2 Microglobulin
🛡️ Overview of the Immune Response
- The immune system is a network of cells, tissues, and organs that protects against bacteria, viruses, fungi, and parasites.
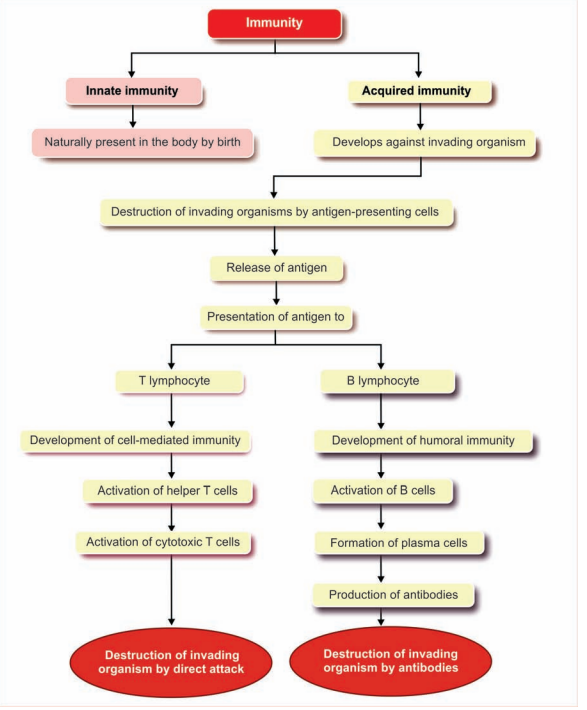
- Two arms work together: innate immunity (fast, non-specific) and adaptive immunity (slower, highly specific with memory).
- Goal: detect → contain → clear → remember pathogens for immediate defence and long-term protection.
⚡ Innate Immune Response
First line of defence, acting within minutes–hours. Recognises conserved patterns (not specific antigens) and buys time for adaptive immunity.
- Physical/Chemical barriers: Skin, tight junctions, mucous, low gastric pH, defensins, lysozyme in tears/saliva.
- Sentinel cells: Macrophages, dendritic cells, neutrophils; recognise PAMPs via PRRs (e.g., TLRs, NOD) → phagocytosis + cytokines.
- Cytokines: IL-1, IL-6, TNF-α (fever, acute-phase response), Type I interferons (IFN-α/β) induce antiviral state.
- NK cells: Kill “missing-self” (↓MHC I) virally infected/tumour cells via perforin/granzymes.
- Complement (3 pathways): Classical (antibody-C1q), Lectin (MBL), Alternative (C3 tick-over). Effects: opsonisation (C3b), inflammation (C3a/C5a), MAC lysis (C5b-9).
- Inflammation: Vasodilation and ↑permeability recruit neutrophils/monocytes (rubor, calor, tumor, dolor).
🎯 Adaptive Immune Response
Highly specific; generates memory. Requires antigen presentation and clonal selection.
- Antigen presentation: Dendritic cells present peptides on MHC II→CD4⁺ T cells; infected cells present on MHC I→CD8⁺ T cells.
- CD4⁺ T helper subsets:
- Th1 (IFN-γ): intracellular microbes; activates macrophages, supports CD8⁺.
- Th2 (IL-4/5/13): helminths; class switch to IgE, eosinophils, allergy.
- Th17 (IL-17/22): extracellular bacteria/fungi; neutrophil recruitment.
- Treg (IL-10, TGF-β): immune tolerance, dampens inflammation.
- CD8⁺ cytotoxic T cells: Kill infected/tumour cells via perforin/granzyme or Fas–FasL.
- B cells (Humoral): With T-cell help (CD40–CD40L + cytokines) undergo germinal-centre class switching and affinity maturation.
- IgM (first response), IgG (opsonisation, placenta), IgA (mucosa, milk), IgE (allergy/parasites), IgD (naïve B-cell receptor).
- Immunological memory: Memory B/T cells drive faster, stronger secondary responses (basis of vaccination).
🧩 Types of Immunity
- Active: Infection or vaccination → own antibodies + memory (durable).
- Passive: Transferred antibodies (placenta IgG, breast milk IgA, immunoglobulin therapy) → immediate, short-lived.
🦠 Examples
- Viral infection: IFN-α/β induced; NK early killing; APC→Th1; CD8⁺ clears infected cells; neutralising IgA/IgG prevent reinfection; memory persists.
- Bacterial infection: Neutrophils + macrophages; complement C3b opsonisation; Th17 recruitment; antibodies (IgG/IgM) neutralise toxins and opsonise.
🧪 Clinical Pearls
- 📈 Inflammatory biomarkers: CRP/ESR (inflammation), procalcitonin (bacterial sepsis guide).
- 🧫 Asplenia: Risk of encapsulated organisms (Strep pneumoniae, H. influenzae b, Neisseria) → vaccinate + prompt antibiotics for fever.
- 🧬 Complement deficiencies: C5–C9 → recurrent Neisseria; C1 esterase inhibitor deficiency → hereditary angioedema (avoid ACEi).
- 🧪 Primary immunodeficiencies: CGD (defective NADPH oxidase → catalase-positive infections); SCID (severe recurrent infections; urgent HSCT).
- 🔥 Hypersensitivity: I (IgE, anaphylaxis), II (cytotoxic), III (immune complex), IV (T-cell mediated, e.g., contact dermatitis).
💉 Vaccination & Adjuvants
- Vaccines simulate infection to generate memory (live-attenuated, inactivated, subunit, mRNA, conjugate).
- Adjuvants (e.g., aluminium salts) boost innate sensing → better T- and B-cell responses.
📌 Summary
Innate immunity provides rapid, pattern-based defence; adaptive immunity offers precision and memory. Effective protection requires antigen presentation, T-helper coordination, antibodies, cytotoxic T-cell killing, and a safe return to homeostasis. Disruption at any step predisposes to infection, autoimmunity, or immunodeficiency.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
