Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Atrioventricular Nodal Reentrant Tachycardia AVNRT
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Wolff-Parkinson White syndrome (WPW) AVRT |Lown Ganong Levine Syndrome AVRT |Supraventricular Tachycardia (SVT) |Atrioventricular Nodal Reentrant Tachycardia AVNRT |Atrial Flutter |Atrial Fibrillation |Sinus Tachycardia |Sinus Arrhythmia |Multifocal Atrial Tachycardia |Resuscitation - Adult Tachycardia Algorithm
📖 About
- Any tachycardia arising from above the level of the Bundle of His.
- Usually refers to reentrant tachycardias around the AV node (AVNRT).
- When the reentry pathway is beyond the node = AVRT (e.g., WPW, Lown-Ganong-Levine).
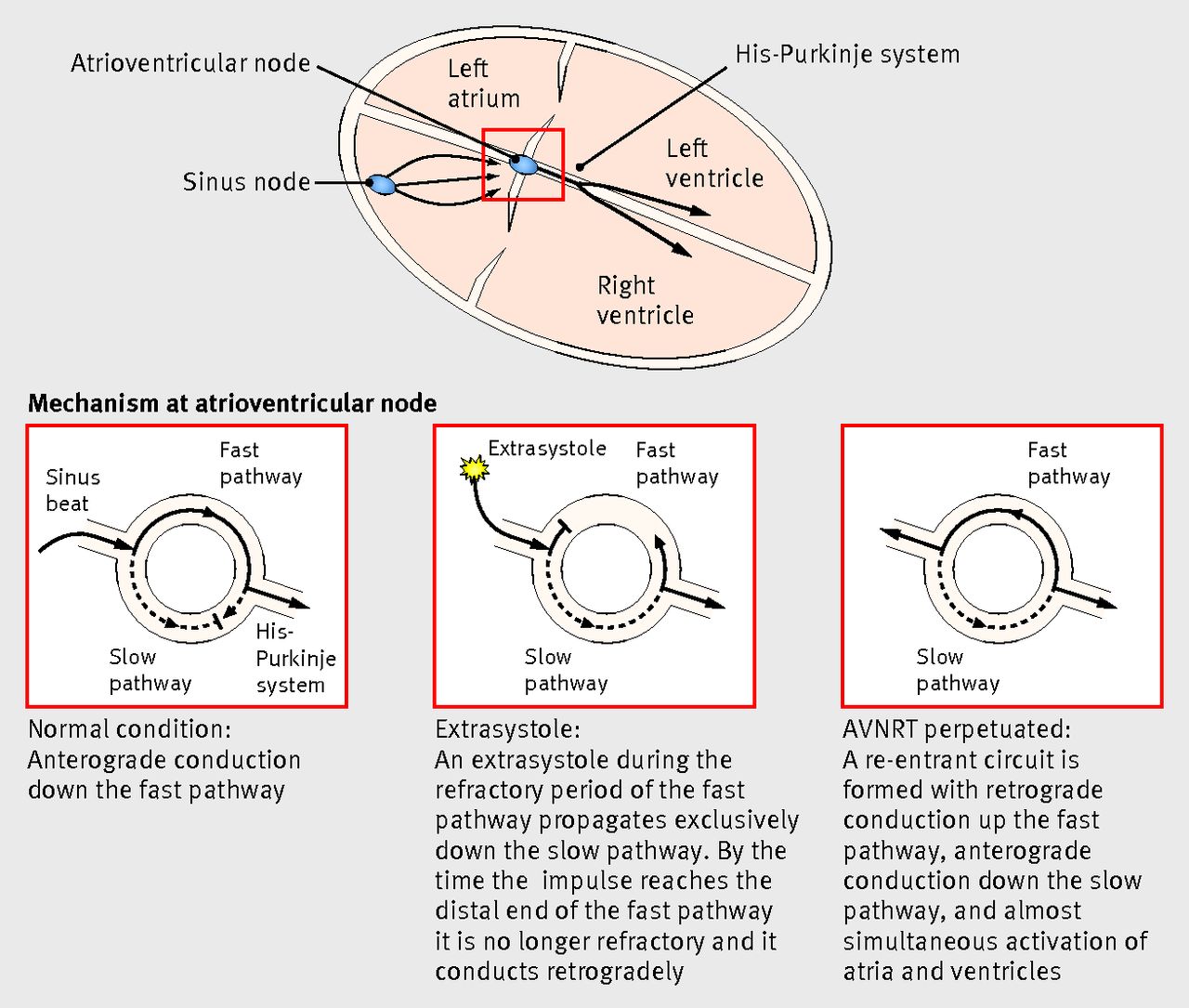
🧬 Aetiology of AVNRT
- Requires 2 pathways (dual physiology) around the AV node:
- ⚡ Slow pathway: short refractory period.
- ⚡ Fast pathway: long refractory period.
- An atrial ectopic impulse may travel down the slow and retrogradely up the fast pathway → like a “🎆 Catherine wheel firework”.
📊 Classification
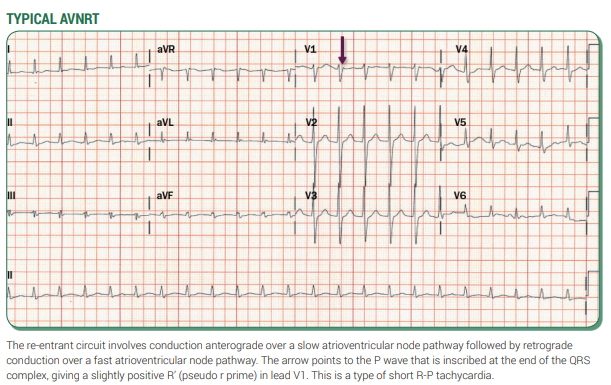
- 🔹 Slow–Fast (≈90%, RP′ < P′R).
- 🔹 Fast–Slow (≈10–15%, RP′ > P′R).
- 🔹 Slow–Slow (<5%).
🖼️ Diagram showing AVNRT
 🩺 Clinical
🩺 Clinical
- Occurs at any age; benign; more common in young females (2:1 ratio).
- Symptoms: palpitations, presyncope, breathlessness, dizziness, chest pain.
- Can be misdiagnosed as a panic attack (often delayed diagnosis).
- Triggers: stress, caffeine, alcohol, smoking, drugs.
🔍 Investigations
- Bloods: FBC, U&E, TFTs, LFTs. CXR.
- 12-lead ECG during episode: narrow complex tachycardia 120–240 bpm. May mimic VT if bundle branch block present.
- Implantable loop recorder if transient/undocumented episodes.
- Echo: exclude structural disease.
- Rarely: check for phaeochromocytoma if hypertension present.
💡 Clinical Pearls
- ⚡ Sudden onset/offset → suggests PSVT.
- 👔 “Shirt flapping” or “neck pounding” → highly suggestive of AVNRT.
- 🚨 Hypotension/syncope → poorly tolerated → urgent treatment/referral.
- Structural heart disease → consider atrial tachycardia.
- Pre-excitation (AVRT/WPW) → refer for specialist ablation.
📸 Examples
 💊 Management
💊 Management
- 🛑 If unstable → immediate DC cardioversion.
- Stable:
- ✅ Vagal manoeuvres (Valsalva, carotid sinus massage).
- ✅ IV adenosine (6–24 mg rapid bolus). Warn about transient unpleasant sensations.
- ✅ IV verapamil (2.5–5 mg slow IV) or diltiazem (if narrow complex only).
- ⚠️ If broad-complex SVT (aberrancy or accessory pathway) → get urgent expert advice. Avoid verapamil/diltiazem if pre-excited AF suspected.
- Pre-excited AF (AVRT): avoid AV nodal blockers (adenosine, digoxin, β-blockers, calcium blockers). Use IV flecainide/propafenone/amiodarone or cardioversion if unstable.
- 📅 Long-term: refer to electrophysiology for catheter ablation (high cure rates, low risk).
📚 References
Cases — AVNRT with Acute Management
- Case 1 — Young Woman with Palpitations: A 26-year-old woman presents to A&E with sudden-onset palpitations, HR 180 bpm, BP 120/70, regular narrow-complex tachycardia on ECG. Management: She is stable → start with modified Valsalva manoeuvre (reverts to sinus rhythm). Observe and discharge with cardiology follow-up. Education on avoiding triggers (caffeine, alcohol).
- Case 2 — Middle-aged Man with Dizziness: A 48-year-old man arrives with palpitations and dizziness. HR 170 bpm, BP 115/70, regular narrow-complex tachycardia. Vagal manoeuvres fail. Management: Give adenosine IV 6 mg rapid bolus → no effect. Repeat 12 mg → tachycardia terminates, sinus rhythm restored. Monitor in ED, advise GP/cardiology follow-up. If recurs frequently → consider prophylaxis or ablation.
- Case 3 — Elderly Patient with Chest Pain and Hypotension: A 70-year-old woman with history of hypertension presents with palpitations, chest pain, and lightheadedness. HR 190 bpm, BP 80/50. ECG: narrow-complex tachycardia. Management: She is unstable → immediate synchronised DC cardioversion. Once stabilised, admitted under cardiology, plan for further evaluation and long-term management (beta-blocker vs catheter ablation depending on comorbidities).
Teaching Commentary ⚡
These three cases highlight the spectrum: - Stable + young → vagal manoeuvres often suffice. - Stable but symptomatic → escalate to adenosine, with verapamil or beta-blocker as alternatives. - Unstable → don’t delay: immediate DC cardioversion. Always remember adenosine is contraindicated in asthma/COPD and should be avoided in patients on dipyridamole or with transplanted hearts (increased sensitivity). Long-term, radiofrequency ablation of the slow pathway is curative in most patients.