| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Trauma: Spinal Injury
Related Subjects: |Transverse myelitis |Acute Disseminated Encephalomyelitis |Cervical spondylosis |Spinal Cord Anatomy |Acute Disc Prolapse |Spinal Cord Compression |Spinal Cord Haematoma |Foix-Alajouanine syndrome |Cauda Equina |Conus Medullaris syndrome |Anterior Spinal Cord syndrome |Central Spinal Cord syndrome |Brown-Sequard Spinal Cord syndrome
🚨 Trauma patients with head injury/coma may also have neck injury. 👉 If in doubt → apply a hard collar to stabilise the cervical spine. 📸 If scanning the head → image the C-spine to at least C7/T1 to avoid missed injuries.
📖 About
- ⏱ Early recognition & stabilisation are vital → delays cause irreversible deficits.
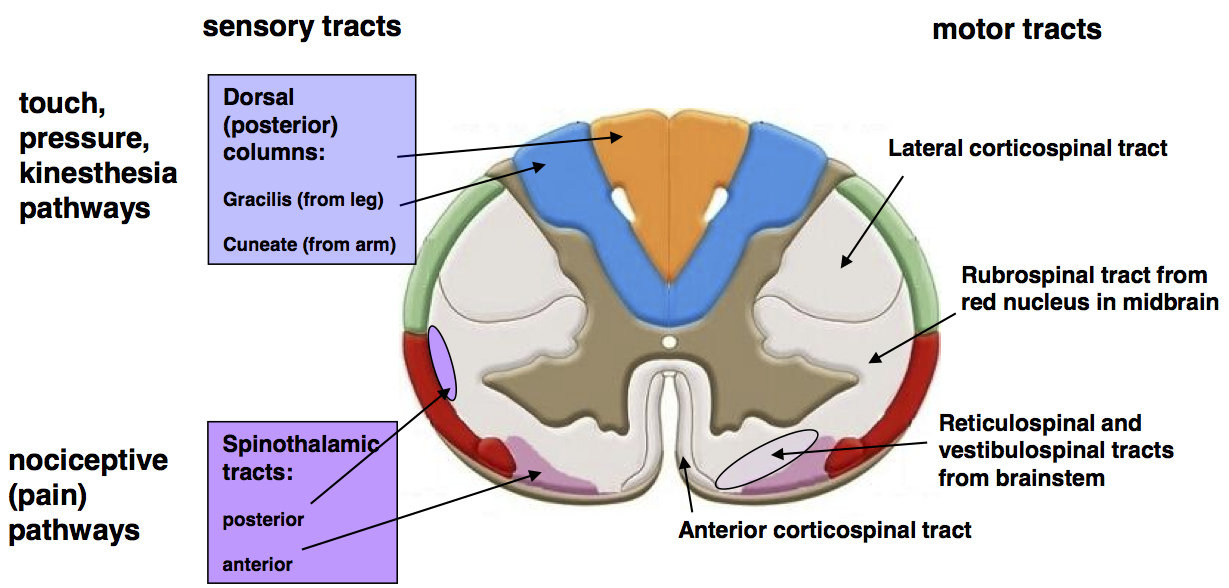
- 🧠 Spinal cord runs foramen magnum → L1; carries motor, sensory & autonomic tracts.
- 💨 C3–C5 innervate diaphragm → "C3, 4, 5 keeps the diaphragm alive".
- ✋ C5–T1 → arms/hands; injury here threatens independence.
🧩 Anatomy
- 31 pairs of spinal nerves:
- 🦴 Cervical: 8 (C1–C8)
- 🦴 Thoracic: 12 (T1–T12)
- 🦴 Lumbar: 5 (L1–L5)
- 🦴 Sacral: 5 (S1–S5)
- 🦴 Coccygeal: 1 (Co1)
⚡ Aetiology
- Traumatic: fracture-dislocation, retropulsed bone fragments, haematoma.
- Non-traumatic: tumour, infection (TB, epidural abscess), degenerative stenosis.
🏗 Structure
- Three spinal columns:
- Anterior: vertebral body front + anterior ligaments.
- Middle: posterior body + posterior longitudinal ligament.
- Posterior: laminae, pedicles, posterior ligaments.
- 💡 Instability = ≥2 columns damaged → surgical concern.
🚗 Causes
- Road traffic accidents (~50%).
- Falls (~25%, esp elderly).
- Violence (GSW/stab ~15%).
- Sports (~10% diving/rugby).
- Industrial/other (~5%).
⚠️ Risk Factors
- Ankylosing spondylitis (rigid fracture-prone spine).
- Cervical spondylosis, congenital/acquired stenosis.
🚨 Dangerous Mechanisms
- Falls >3 feet / >5 steps.
- Axial load (diving injury).
- High-speed RTA, rollover, ejection.
- Motorbike/ATV crashes.
- Bicycle vs vehicle collision.
🩺 Clinical Features
- ⚡ Spinal shock: flaccid paralysis, areflexia, atonic bladder (acute).
- ↗️ Later: hyperreflexia, spasticity, Babinski, autonomic overactivity.
- 📍 Midline pain, tenderness, sensory level on exam.
- 💨 Diaphragmatic breathing if C3–5 intact but intercostals lost.
- 🦽 Paraplegia (below T1), quadriplegia (cervical).
- 🍌 Priapism + hypotension/bradycardia → classic cord transection clue.
🔎 Incomplete Cord Syndromes
- Brown-Séquard: ipsilateral motor/proprioception loss + contralateral pain/temp loss.
- Anterior cord: bilateral motor + pain/temp loss, preserved vibration/proprioception.
- Central cord: arms > legs weakness, often post-hyperextension in cervical spondylosis.
🧪 Investigations
- 🩻 X-ray: AP, lateral, odontoid, ensure C7/T1 included.
- 💻 CT: gold standard for bone fractures/dislocation.
- 🖥 MRI: best for cord, discs, ligaments, haematoma.
- 🧠 Neuro exam: tone, reflexes, sensory level, Babinski.
🚑 Management
🛑 Treat all suspected spinal injuries as unstable until cleared.
- ABCDE trauma approach (manual in-line stabilisation).
- Immobilisation: hard collar, blocks, vacuum mattress.
- Airway/ventilation: high cervical injuries → early intubation.
- Steroids: methylprednisolone use is controversial; follow local/NICE policy.
- Surgery: urgent decompression + stabilisation if compression/instability.
- Supportive: catheterisation, VTE prophylaxis, pressure sore prevention.
- Rehabilitation: physio, OT, psychological/vocational support.
📊 Functional Outcome by Level
| Level | Functional Outcome |
|---|---|
| C1–C3 | Ventilator dependent, minimal movement. |
| C4 | Diaphragm intact, limited shoulder movement. |
| C5–C6 | Partial arm use; independent feeding with aids. |
| C7–C8 | Hand function improves; possible wheelchair independence. |
| T1–T12 | Paraplegia; wheelchair, independent upper limbs. |
| L1–S5 | Variable leg function; potential for assisted walking. |
🌅 Prognosis
- Depends on level + completeness.
- ⏱ Early decompression (<24h) → better recovery.
- High cervical complete = poor survival, often ventilator-dependent.
- Incomplete injuries (esp. central cord) = best recovery chance.
- Long-term issues: UTIs, pressure sores, DVT/PE, depression.
🛡 Prevention
- Seatbelts, helmets, sports safety gear.
- Fall prevention in elderly.
- Posture and back-strengthening programmes.
- Manage predisposing spinal diseases (e.g., AS, spondylosis).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
