| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Necrotising Enterocolitis
⚠️ Necrotising Enterocolitis (NEC) affects ~5% of infants with birth weights <1,500g. It often presents with abdominal distension, bloody stools, bile-stained vomiting, and the classic radiological finding of pneumatosis intestinalis.
🍼 About
- NEC is a life-threatening gastrointestinal emergency, almost exclusively affecting premature neonates.
- It can lead to bowel perforation, peritonitis, septic shock, and death.
- Mortality remains high (20–30%), especially with advanced disease.
⚡ Aetiology & Pathophysiology
- Immature intestinal mucosa + impaired barrier function.
- Combination of ischaemia–reperfusion injury, bacterial invasion, and an exaggerated inflammatory response.
- Inflammatory mediators (PAF, TNF, cytokines) → necrosis of intestinal wall.
📌 Risk Factors
- Prematurity & very low birth weight (VLBW).
- Formula feeding ❌ (breastfeeding protective).
- Congenital heart disease (↓ mesenteric perfusion).
- Polycythaemia, PDA, or use of umbilical arterial catheters near mesenteric arteries.
- Medications: Indomethacin, steroids (with indomethacin).
- Maternal factors: Cocaine exposure, perinatal hypoxia.
🩺 Clinical Presentation
- Feeding intolerance or bilious vomiting 💚.
- Abdominal distension, tenderness, wall oedema, or palpable mass.
- Blood-stained stools 💩.
- Absent bowel sounds, shock, apnoea, bradycardia in severe disease.
- Signs of perforation → rigid abdomen, peritonitis, rapid collapse.
🔬 Investigations
- Bloods: ↑ WCC/CRP, ↑ lactate, thrombocytopenia, coagulopathy (DIC).
- U&E: AKI, hyponatraemia.
- Blood gas: Metabolic acidosis (classic).
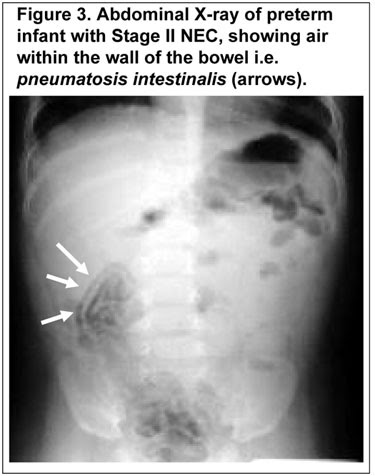
- AXR: Pneumatosis intestinalis (gas in bowel wall), portal venous gas, free air (if perforation).
📊 Staging – Bell’s Criteria
| Stage | Clinical Features | Investigations |
|---|---|---|
| Stage I (Suspected) | Feeding intolerance, abdominal distension, occult/visible blood in stool, apnoea, bradycardia | AXR: non-specific, mild distension |
| Stage II (Definite) | Absent bowel sounds, tenderness, systemic illness | Pneumatosis intestinalis or portal venous gas, metabolic acidosis, thrombocytopenia |
| Stage III (Advanced) | Severe illness, peritonitis, shock, DIC | Pneumoperitoneum = perforation |
🛠️ Management
- Resuscitation: ABC, fluids, correct acidosis, oxygen/ventilation if needed. Morphine for pain.
- Medical (first-line in suspected/early cases):
- Nil by mouth (NBM) 🚫🍼
- IV fluids & TPN
- Broad-spectrum IV antibiotics
- NG tube for decompression
- Surgical:
- Consult urgently if pneumoperitoneum, peritonitis, or clinical deterioration.
- Options: bowel resection ± stoma, or peritoneal drain in VLBW infants.
- Special situations: Avoid indomethacin in PDA with NEC. Consider PDA closure surgically.
⚠️ Complications
- Sepsis & peritonitis → multiorgan failure.
- Intestinal strictures (esp. colon).
- Short bowel syndrome → prolonged TPN dependence.
📚 References
Cases — Necrotising Enterocolitis (NEC) 👶🩺
- Case 1 — Preterm Baby with Distended Abdomen 🌡️: A 28-week preterm infant, day 10 of life, develops abdominal distension, bilious gastric aspirates, and bloody stools. Exam: tender abdomen, reduced bowel sounds. Abdominal X-ray: pneumatosis intestinalis. Diagnosis: NEC in very preterm infant. Management: Stop enteral feeds (NPO), NG decompression, IV antibiotics, supportive fluids; surgical review if perforation.
- Case 2 — Term Baby with Congenital Heart Disease 💔: A 3-day-old term neonate with hypoplastic left heart syndrome develops abdominal distension and fresh blood per rectum after formula feeding. CXR: portal venous gas. Diagnosis: NEC in term infant, precipitated by poor gut perfusion (CHD). Management: Supportive (IV fluids, antibiotics, NPO), optimise cardiac status, surgical team involvement if perforation/peritonitis suspected.
- Case 3 — Complicated NEC with Perforation ⚠️: A 2-week-old preterm neonate suddenly deteriorates with apnoea, abdominal wall erythema, and shock. Abdominal X-ray: free intraperitoneal air. Diagnosis: NEC complicated by intestinal perforation and peritonitis. Management: Emergency surgical intervention (laparotomy ± resection), broad-spectrum antibiotics, intensive care support.
Teaching Commentary 🧠
NEC = acute intestinal necrosis, mainly in preterm neonates. - Risk factors: prematurity, formula feeding, hypoxic/ischaemic events, congenital heart disease. - Clinical features: feeding intolerance, abdominal distension, bloody stools, sepsis. - Key radiology: pneumatosis intestinalis (air in bowel wall), portal venous gas, free air (perforation). - Management: Stop feeds, NG decompression, broad-spectrum antibiotics, fluid resuscitation, surgical referral if perforation/necrosis. ⚠️ Mortality is high; survivors may develop short bowel syndrome or strictures.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
