| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Cervical Spine Immobilisation and Management
Related Subjects: |Spinal Cord Anatomy |Initial Trauma Assessment and Management |Cervical Spine Immobilization and Management |Anatomy of the Cervical Vertebrae C1 (Atlas) and C2 (Axis) |Trauma: Spinal Injury
Indications for Cervical Spine Immobilization and Management
🦴 Cervical spine immobilisation is a cornerstone of trauma management, designed to prevent secondary spinal cord injury. It is particularly vital in patients presenting with trauma, altered consciousness, or neurological symptoms where cervical injury is suspected.
High-Risk Mechanisms of Injury
- ⬇️ Falls >3 metres
- 🤿 Axial head loading (e.g., diving injuries)
- 🚗 High-speed MVCs, rollovers, or ejections
- 🏍️ Motorised recreational vehicle accidents
- 🚲 Cyclist struck or collision
- 👴 Age >65 years with cervical pain post-trauma
- ⚡ Paraesthesia in extremities after trauma
🎯 Aim of Care: Prevent secondary spinal cord injury → prompt collar application, safe handling, and adherence to spinal precautions.
Spinal Precautions Protocols
- 👩⚕️ Staff Education: Regular training & accreditation in spinal handling.
- 🛡️ Prevent Complications:
- Meticulous collar fitting & skin care
- Frequent turning, pressure area care
- Early upright positioning once cleared
- 🧲 Early Spinal Clearance:
- Timely imaging (X-ray, CT, MRI as indicated)
- Clear communication between ED, radiology, ICU/ward teams
- Accurate documentation of clinical findings & clearance
Guidelines for Applying Semi-Rigid Cervical Collars
- 🟠 Apply to all patients with multi-trauma or head injury until cervical spine is excluded.
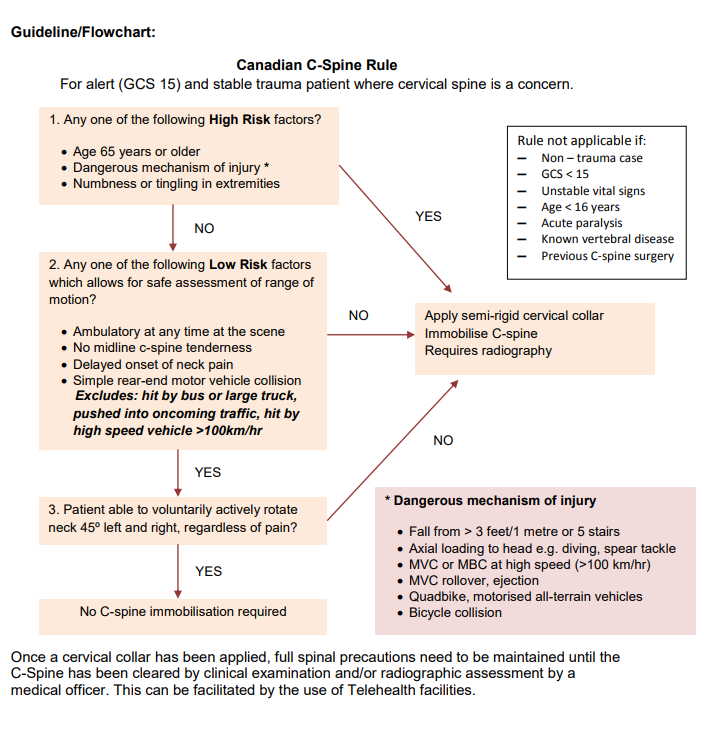
- 📏 Use the Canadian C-Spine Rule (preferred in UK/Europe) to assess need:
- High-risk factors (e.g., age >65, dangerous mechanism, paraesthesia) → imaging
- Low-risk factors (simple rear-end MVC, sitting in ED, ambulatory, delayed pain, no midline tenderness) → safe assessment
- Rotation of neck 45° left & right = clearance
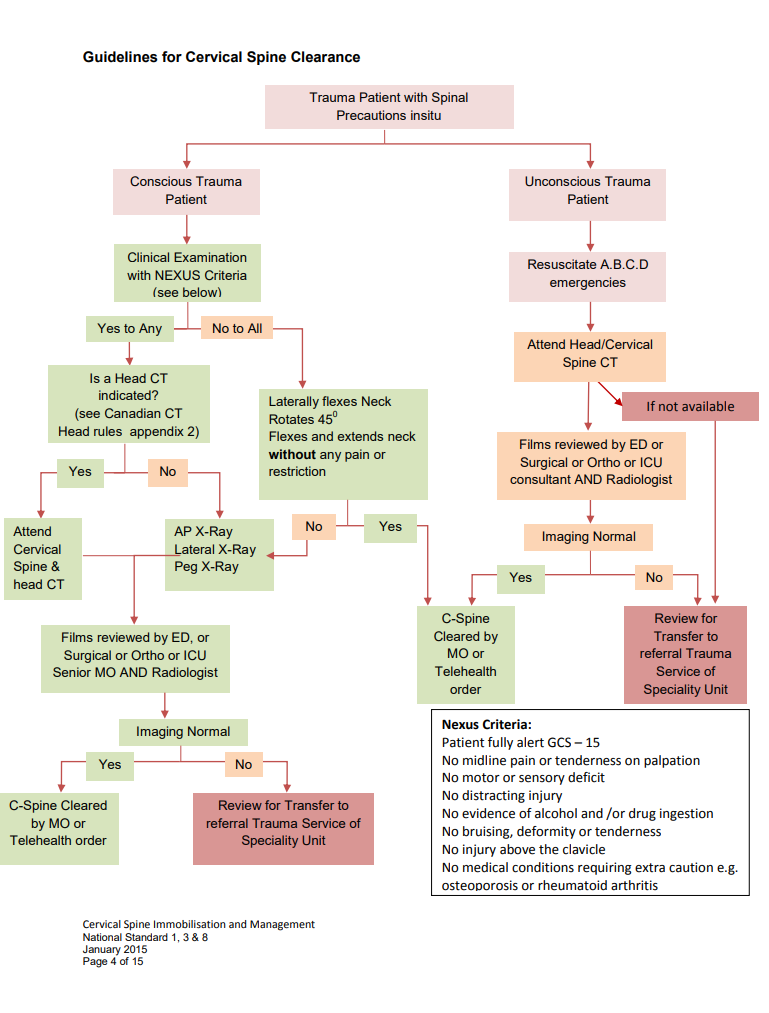
- 🇺🇸 The NEXUS criteria are an alternative (no midline tenderness, no neuro deficit, normal alertness, no intoxication, no distracting injury).
- ✅ Remove collar once clinical or radiological clearance is confirmed.
Equipment & Materials Required
- 🛏️ Trauma mattress (X-ray board optional)
- 📟 Cardiac-monitored bed within staff sight
- 🔔 Call system and log-roll equipment
- 👥 Minimum of 3 trained staff for safe handling
- 🦴 Semi-rigid cervical immobilisation device (e.g., Philadelphia collar)
- 🧤 PPE and hand hygiene facilities
- 🩻 Access to X-ray / CT / MRI
Key Principles of Spinal Immobilisation
- 🧍 Stable, alert patients may be cleared clinically if low-risk.
- 🧲 Imaging (CT preferred in adults, plain X-ray sometimes in children) required if criteria not met.
- 📌 Inline immobilisation maintained until clearance achieved.
- 😴 Patients with reduced GCS cannot be cleared until fully alert.
- 👨⚕️ Senior review essential if doubt exists.
Complications of Prolonged Spinal Immobilisation
- 🩹 Pressure ulcers from collars
- 🧠 Raised intracranial pressure
- 💨 Ventilation delays, aspiration risk
- 🥣 Intolerance of enteral feeding
- 🩸 DVT risk from immobility
- 🫁 Respiratory infections & secretion retention
⚖️ Balance of Risk: Over-immobilisation is harmful. Early and safe clearance prevents avoidable complications.
References
- Cervical Spine Immobilisation and Management – NSW ACI Guideline
- NICE CG176: Head Injury (with spinal injury considerations)
- Stiell IG et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA 2001.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
