| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Guillain Barre Syndrome
Related Subjects: |Herpes Varicella-Zoster (Shingles) Infection |Herpes Viruses |Herpes Zoster Ophthalmicus (HZO) Shingles |MonkeyPox |Mumps |Measles |Rubella (German Measles) |Epstein-Barr Virus infection |Cytomegalovirus (CMV) infections |CMV retinitis infections |Toxoplasmosis |Respiratory Failure
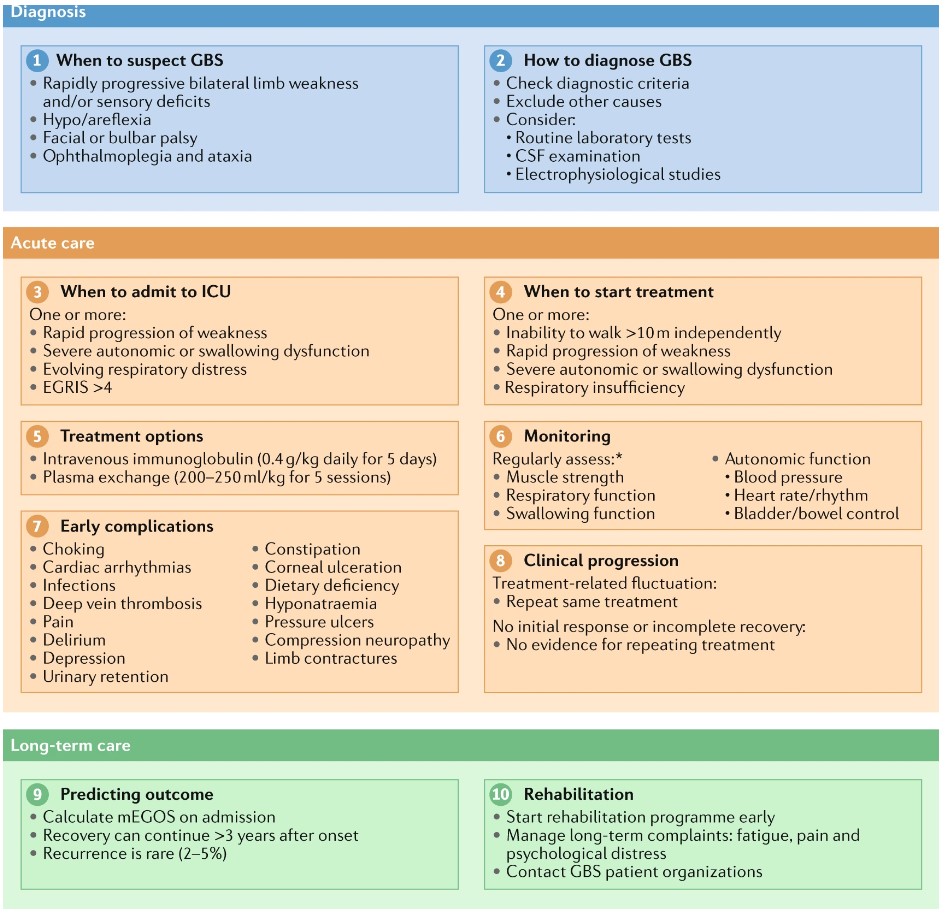
🧠 Guillain-Barré Syndrome (GBS): Respiratory function must always be monitored, as failure may occur silently without dyspnoea. ⚠️ Around 20% of patients need mechanical ventilation. 📏 Bedside test = Forced Vital Capacity (FVC); <1.5 L suggests ITU admission. 💉 IVIG within 2 weeks of onset is as effective as plasma exchange (Cochrane review) and more likely to be completed.
🩺 Initial Management of GBS
| Initial Priorities |
|---|
|
📖 About
- Acute onset ascending weakness + areflexia 🔽.
- Potentially life-threatening due to autonomic or respiratory failure.
- Also called Acute Inflammatory Demyelinating Polyneuropathy (AIDP).
🧬 Aetiology
- ⚔️ Autoimmune attack against peripheral nerves (molecular mimicry).
- 🌱 Infectious triggers: Campylobacter jejuni, CMV, HIV, HEV, EBV, Mycoplasma, Zika, Lyme.
- Pathology: multifocal demyelination + high CSF protein (albuminocytologic dissociation).
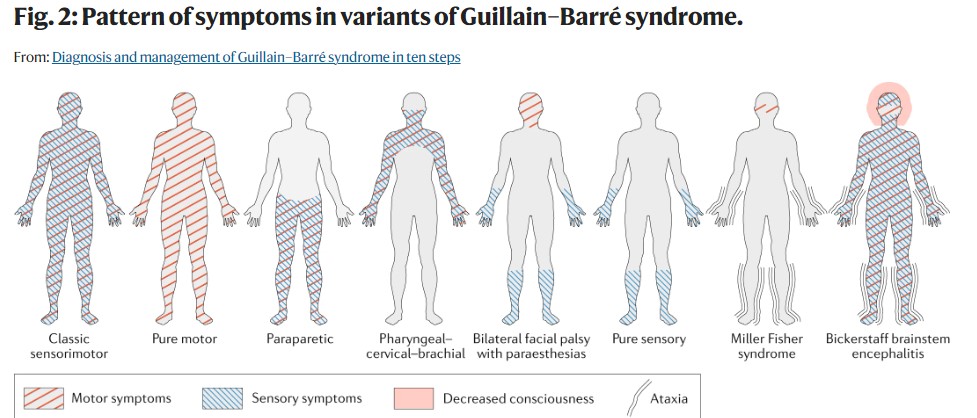
🔎 Subtypes of GBS
- AIDP (90%) – classic form, demyelinating.
- AMAN (5%) – acute motor axonal neuropathy, often after Campylobacter.
- Miller-Fisher (5%) – triad: ophthalmoplegia 👁️, ataxia 🚶, areflexia.
- AMSAN (1%) – motor + sensory axonal neuropathy.
⚠️ Clinical Features
- 🔼 Ascending weakness (legs → trunk → arms → cranial nerves).
- ❌ Areflexia.
- 🫁 Respiratory weakness ± need for ventilation.
- ❤️ Dysautonomia: BP swings, arrhythmias, pupillary changes.
- 🩻 Back pain, sensory loss, cranial neuropathies.
- 👀 Papilloedema possible due to high CSF protein.
🧪 Investigations
- 🧫 CSF: Protein ↑, normal WCC (may be normal early).
- ⚡ NCS: Slowed conduction, absent F-waves, conduction block.
- 🫀 ECG: monitor for arrhythmias.
- 🧬 Antibody testing rarely useful (anti-GD1a, anti-GQ1b in Miller-Fisher).
🩻 Differentials
- Spinal cord lesions (transverse myelitis).
- Myasthenia gravis, botulism.
- Tick paralysis, diphtheria, poliomyelitis.
- Acute porphyria.
🚨 Indications for ITU/Intubation
- FVC <15–20 ml/kg or <1 L.
- 🫁 Abnormal inspiratory/expiratory pressures.
- ❌ Severe bulbar weakness or impaired cough.
- 📉 Autonomic instability or abnormal gases.
💊 Management
- Specific: IVIG (within 2 weeks) or plasma exchange (within 4 weeks). 🚫 Steroids ineffective.
- Supportive: ITU if required, VTE prophylaxis, physiotherapy, speech therapy, nutrition support.
- Pain: Neuropathic analgesia (gabapentin, carbamazepine). Avoid amitriptyline (arrhythmia risk).
📈 Outcome
- Most improve within 12 months, but recovery may continue up to 5 years.
- 85% recover well; 15% left with disability.
- Poor prognosis: rapid onset, older age, preceding diarrhoea, severe initial weakness.
⚠️ Complications
- Bulbar dysfunction → aspiration, malnutrition.
- Autonomic storms → arrhythmias, BP swings.
- Immobility → pressure sores, DVT/PE, infections.
📚 References
Cases — Guillain–Barré Syndrome (GBS)
- Case 1 — Classic Post-Infectious Ascending Weakness 🦵: A 32-year-old man develops tingling in his feet one week after a Campylobacter gastroenteritis. Over 3 days, he develops progressive ascending weakness, now unable to climb stairs. Exam: bilateral foot drop, absent ankle reflexes, intact cranial nerves. Diagnosis: Acute inflammatory demyelinating polyneuropathy (AIDP, most common GBS subtype). Management: Admit for monitoring; IV immunoglobulin (IVIG) or plasma exchange; monitor vital capacity regularly.
- Case 2 — Miller–Fisher Variant 👁️: A 45-year-old woman presents with acute diplopia and unsteady gait. Exam: ophthalmoplegia, ataxia, and areflexia, but normal limb strength. CSF shows albuminocytologic dissociation. Anti-GQ1b antibodies positive. Diagnosis: Miller–Fisher variant of GBS. Management: IVIG; supportive physiotherapy and rehabilitation.
- Case 3 — Severe GBS with Respiratory Involvement 🫁: A 28-year-old man presents with progressive ascending weakness, facial diplegia, and dysphagia. Exam: bilateral flaccid paralysis, absent reflexes, reduced single-breath count. Diagnosis: Severe GBS with bulbar and respiratory muscle involvement. Management: Admit to ICU; intubation and ventilation if vital capacity falls; IVIG or plasma exchange; multidisciplinary supportive care.
Teaching Commentary 🧠
GBS is an acute, immune-mediated polyneuropathy triggered by infections (e.g. Campylobacter, EBV, CMV, HIV) or rarely vaccination. Hallmarks: progressive symmetrical weakness (usually ascending), areflexia, mild sensory symptoms, autonomic instability (arrhythmias, BP swings). Investigations: - CSF: albuminocytologic dissociation (↑protein, normal cells). - Nerve conduction: demyelination (slowed conduction, conduction block). Complications: respiratory failure (20–30%), autonomic dysfunction. Treatment: IVIG or plasma exchange (equally effective); steroids are not helpful. Monitor in hospital until clear plateau or recovery.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
