| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Vertebral artery dissection
Related Subjects: |Neurological History taking |Causes of Stroke |Ischaemic Stroke |Subarachnoid Haemorrhage |Cerebral Arterial Perfusion and Clinical Correlates |Anterior circulation Brain |Posterior circulation Brain |Acute Stroke Assessment (ROSIER&NIHSS) |Carotid Artery dissection |Vertebral artery dissection |Acute Stroke Assessment (ROSIER&NIHSS) |Atrial Fibrillation |Atrial Myxoma |Causes of Stroke |Ischaemic Stroke |Cancer and Stroke |Cerebral Venous thrombosis |Cardioembolic stroke |CT Basics for Stroke |Endocarditis and Stroke |Haemorrhagic Stroke |Stroke Thrombolysis |Hyperacute Stroke Care |Anatomy and Physiology of the Brain |Cryptogenic stroke |Carotid Web |Anterior / Medial Medullary Infarct (Dejerine Syndrome)
📖 About
- Always consider vertebral artery dissection in a young patient with posterior circulation stroke (esp. dizziness, ataxia, vision loss).
- Accounts for ~10–25% of strokes in young adults (<50 years).
- Pathology: vessel wall tear → intramural haematoma → luminal narrowing/thrombosis → emboli.
⚙️ Aetiology
- Dissection → intraluminal clot → embolisation or local occlusion.
- Common sites: at C1–C2 level or origin of the PICA.
- Connective tissue disorders (Ehlers–Danlos IV, fibromuscular dysplasia) predispose.
- Triggered by minor trauma or sudden neck movements (e.g. chiropractor, hairdresser basin, yoga, sports).
- Rare but severe: basilar artery dissection → high mortality.
🧬 Predisposing Factors
- 🦴 Neck trauma (rotation/flexion stresses).
- 🧬 Connective tissue disorders: Ehlers–Danlos IV, fibromuscular dysplasia, cystic medial necrosis.
- ⚡ Genetic conditions: Marfan, COL1 mutations, osteogenesis imperfecta type 1.
- 🧠 Migraine, family history of dissection.
- 🚺 Pregnancy and postpartum state.
- 🚬 Smoking as an acquired risk factor.
Normal Angiography with carotids removed
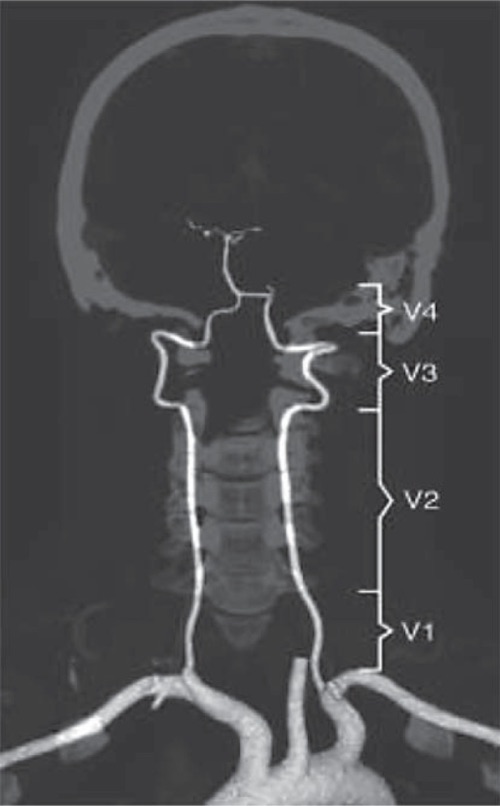
Left Proximal Vertebral dissection

🩺 Clinical Presentation
- 🪖 Headache/neck pain (often sudden, occipital, unilateral).
- 🎯 Posterior circulation stroke signs: dizziness, diplopia, vertigo, dysarthria, ataxia.
- 🧑⚕️ Lateral medullary (Wallenberg) syndrome: ipsilateral facial numbness, contralateral body numbness, dysphagia, hoarseness, Horner’s syndrome.
- 💢 Intracranial dissections: may rupture → subarachnoid haemorrhage (SAH) (up to 50% cases).
🔍 Investigations
- 🖼️ CTA: Best initial test – shows vessel narrowing, occlusion, or dissection flap.
- 🧲 MRI/MRA with fat suppression: Characteristic crescent sign = intramural haematoma.
- 📡 Doppler ultrasound: May suggest occlusion or flow turbulence, but less sensitive in vertebral arteries.
⚖️ Management
- 💊 Anticoagulation (warfarin) for 3–6 months was traditional; evidence is mixed.
- 💊 Dual antiplatelet therapy (aspirin + clopidogrel) is now often used as an alternative, esp. if SAH risk.
- 📉 Choice of antithrombotic depends on location: – Extracranial dissection → antithrombotic therapy reasonable. – Intracranial dissection → higher SAH risk → anticoagulation often avoided.
- 🧑⚕️ Basilar dissections: poor prognosis, sometimes considered for stenting but evidence limited.
- 📆 Follow-up vascular imaging at 3–6 months to assess healing.
💡 Exam Pearls:
– Think vertebral dissection in a young patient with posterior circulation stroke + neck pain.
– Crescent sign on MRI is classic.
– Management: antithrombotics (antiplatelet or anticoagulation) but intracranial dissections carry SAH risk.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
