| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Basal Cell Carcinoma (BCC)
Related Subjects: |Nikolsky's sign |Koebner phenomenon |Erythema Multiforme |Pyoderma gangrenosum |Erythema Nodosum |Dermatitis Herpetiformis |Lichen Planus |Acanthosis Nigricans |Acne Rosacea |Acne Vulgaris |Alopecia |Vitiligo |Urticaria |Basal Cell Carcinoma |Malignant Melanoma |Squamous Cell Carcinoma |Mycosis Fungoides (Sezary Syndrome) |Xeroderma pigmentosum |Bullous Pemphigoid |Pemphigus Vulgaris |Seborrheic Dermatitis |Pityriasis/Tinea versicolor infections |Pityriasis rosea |Scabies |Dermatomyositis |Toxic Epidermal Necrolysis |Stevens-Johnson Syndrome |Atopic Eczema/Atopic Dermatitis |Psoriasis
🧴 Basal Cell Carcinoma (BCC) is a slow-growing tumor originating from epidermal basal keratinocytes. It has a high cure rate (~95%) and very rarely metastasises. It is the most common type of skin cancer in the UK and often forms a classic “rodent ulcer.” 🐭
🧬 Pathology
- BCC is the most common skin malignancy.
- Originates from basal keratinocytes in the epidermis/adnexal structures.
- Gene defects in the sonic hedgehog signalling pathway are often present.
- Lack of metastases is thought to reflect stromal dependency (requires tumour stroma to survive).
☀️ Aetiology
- Main cause: ultraviolet (UV) radiation (sunlight or tanning beds).
- ~50% have defects in the P53 tumour suppressor gene.
- More common in those unable to tan (fair-skinned).
- Predominantly affects those >40 years old.
- Familial cases rare, except in Gorlin’s syndrome.
⚠️ Risk Factors
- Excessive UV exposure (sun/tanning beds).
- Sun-exposed sites: face, neck, scalp, ears.
- Outdoor workers, outdoor activities, sunny climates.
- Fair skin, burns easily, rarely tans.
- Other risks: radiation, arsenic, immunosuppression, xeroderma pigmentosum.
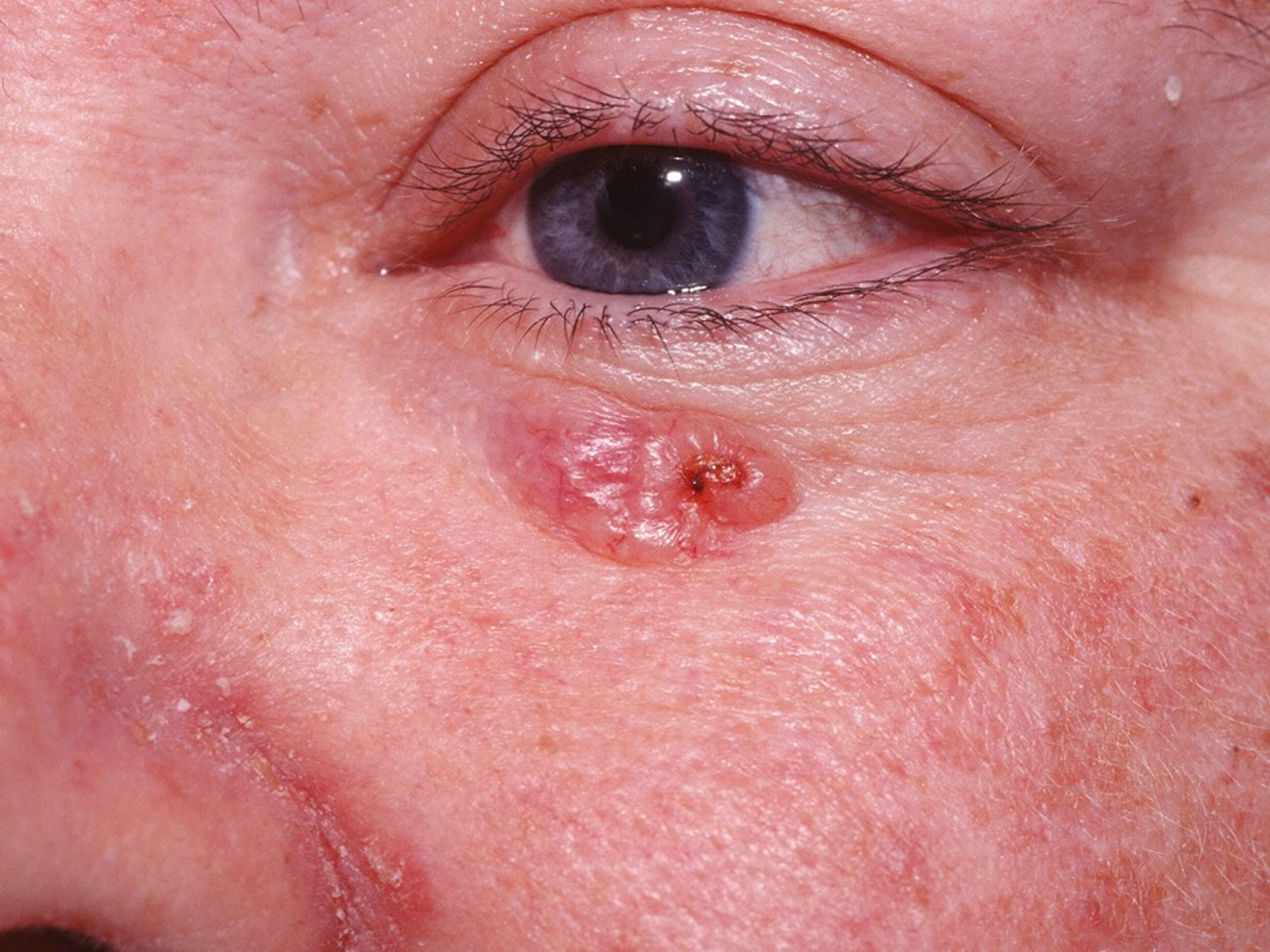

👁️ Clinical Presentation
- Sites: face, head, neck, inner canthus, behind ear.
- Appears as a non-healing scab or new skin lump.
- Superficial BCC: red, scaly, flat patch.
- Nodular: pearly rim, central ulcer, telangiectasia.
- If untreated → classic “rodent ulcer” with tissue destruction.
- Usually painless, may itch or bleed.
- Locally invasive; rarely spreads to nodes.
🔎 Clinical Subtypes
- Nodular: Pearly edges, ulcerative, cystic.
- Pigmented: Dark, mimics melanoma.
- Morpheic: Scar-like, pale plaques.
- Superficial: Flat, erythematous, less invasive.
🧪 Investigations
- Skin Biopsy: Excision biopsy is diagnostic and often therapeutic.
💉 Management
- Wide Local Excision: Main treatment (may require grafting if large).
- Mohs Micrographic Surgery: Best for sensitive/recurrent sites (nose, eyes, ears). Tissue is removed layer by layer until clear.
- Superficial BCCs: Curettage & cautery, cryotherapy, or topical 5-FU / imiquimod.
- Photodynamic Therapy: Light-activated cream; used in some dermatology units.
- Other: Radiotherapy, cryotherapy, intralesional interferon.
- Vismodegib: Oral therapy for advanced/metastatic BCC (hedgehog pathway inhibitor).
🛡️ Prevention & Self-Check
- Skin self-exams: Check monthly; ask partner/family to check back/hidden areas.
- Sunscreen: Use SPF ≥30, broad-spectrum (UVA + UVB). Reapply every 2h, after swimming or towel-drying.
- Sun avoidance: Stay in shade 10am–4pm. Use hats, sunglasses, clothing.
- Children: Never expose babies/young children to direct sunlight.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
