| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Superior Vena Caval Obstruction syndrome
Related Subjects: |Hypercalcaemia |Neutropenic Sepsis |Pulmonary Embolism |Lung Cancer |Superior vena caval obstruction syndrome |Cerebral Metastases |Metastatic bone disease |Oncological emergencies
🚨 Superior vena cava (SVC) obstruction develops in 5–10% of patients with right-sided malignant intrathoracic mass lesions. ⚡ Early recognition and treatment are crucial to prevent life-threatening complications.
📖 About
- Superior Vena Cava (SVC) Obstruction: Blockage of venous return from the head, neck, arms, and upper chest to the heart.
- 🫁 Usually due to external compression or intraluminal thrombosis.
- 🧑⚕️ Recognised as an oncological emergency in clinical practice.
🧬 Aetiology
- 🚫 Impedes venous return → ↑ venous pressure in upper body.
- 🧩 SVC has thin walls and low pressure → easily compressed by mediastinal structures.
- 📍 Location: lies adjacent to right upper lobe and mediastinum → vulnerable to compression by tumours.
- ~85% of cases = malignancy (lung cancer, lymphoma).
⚠️ Causes
- Malignancy: NSCLC, SCLC, lymphoma, metastatic disease.
- Thrombosis: Related to CVCs, pacemakers, or PICC lines.
- Fibrosis: Mediastinal fibrosis post-infection or radiotherapy.
- Vascular: Aortic aneurysm, AV fistula.
- Infections: TB, syphilis, histoplasmosis.
- Children: Non-Hodgkin’s lymphoma is a common cause.
🩺 Clinical Features
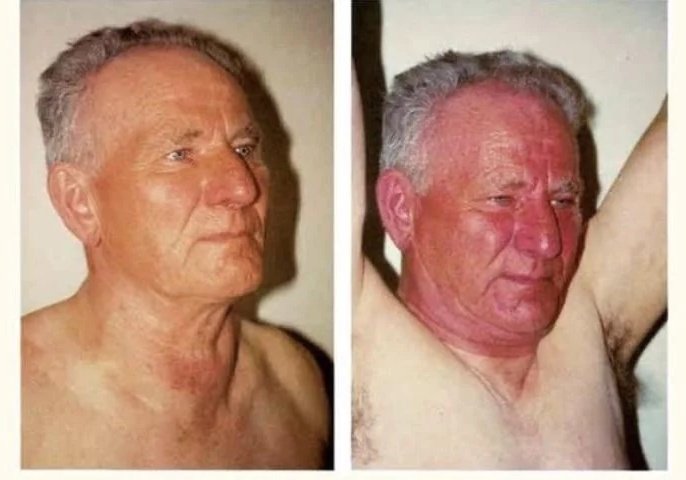
- 😶🌫️ Facial/neck swelling, plethora, dyspnoea, persistent cough.
- 🫁 Severe: stridor, wheeze, airway compromise (tracheal compression).
- 🧵 Dilated neck & chest wall veins (collaterals).
- 🙆♂️ Pemberton’s sign: Raising arms above head → facial congestion & cyanosis worsens.
🔬 Investigations
- Bloods: FBC, U&E, LFTs, CRP, calcium, ALP.
- CXR: Widened mediastinum; ± right pleural effusion (~25%).
- CT Chest: Gold standard – defines site, cause, biopsy planning.
- Sputum Cytology: May identify lung malignancy.
- Contrast Venography: Definitive but invasive – rarely required if CT sufficient.
🧪 Pathology
- 🔴 Majority = malignancy (lung ca, lymphoma).
- Either direct invasion or external compression of SVC wall.
💊 Management
- Supportive: ABC, oxygen, elevate head, secure airway if threatened.
- Steroids: May reduce swelling, esp. with lymphoma.
- Radiotherapy: Treatment of choice for NSCLC.
- Chemotherapy: Effective in SCLC and lymphoma.
- Venous Stenting: Rapid palliation; used if recurrent or severe obstruction.
- Thrombosis: Remove causative line/device, start anticoagulation.
📌 UK Exam Pearls
- 🚨 SVC obstruction is an oncological emergency → urgent oncology input needed.
- 🫁 Most common cause = lung cancer (esp. right-sided). In children → lymphoma.
- 🙆♂️ Pemberton’s sign is highly testable and a classic finding.
- ⚡ Stenting provides the fastest symptomatic relief, especially if airway/brain perfusion threatened.
- 📍 Distinguish malignant vs thrombotic cause → treatment strategy differs.
🚩 SVC Obstruction Red Flags:
- 🧠 Raised ICP: headache, confusion, papilloedema.
- 🫁 Airway compromise: stridor, severe dyspnoea.
- 👁️ Rapidly progressive facial/neck swelling with cyanosis.
- ⚡ Syncope or cardiovascular compromise.
📚 References
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
