| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Neurological examination - Eyes
🚨 Red flags: dysphagia, unplanned weight loss, anorexia, haematemesis/melaena, older age, lack of therapy response, chronic symptoms, long-term drug use.
👁️ Basics
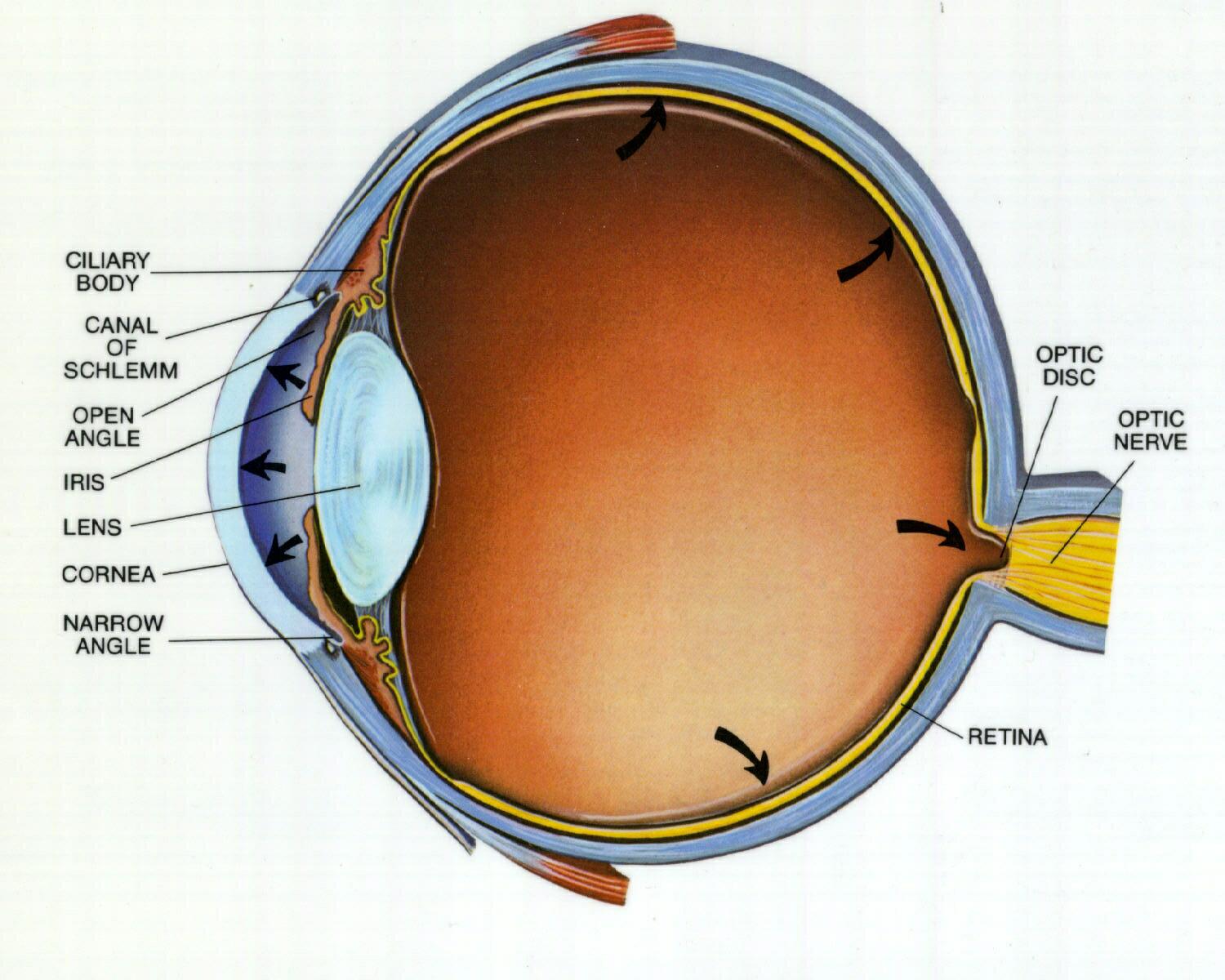
- Know retinal anatomy & physiology – cones 🎨 (central, colour) vs rods 🌙 (peripheral, low light).
- Optic nerve exits nasal side; macula packed with cones.
- Optic pathways – essential to draw for exams 📝.
- Brainstem & CN III, IV, VI → control of eye movements.
👀 External Appearance
- 👁️🗨️ Partial Ptosis: Horner’s, myasthenia, dystrophy.
- ⬇️ Full Ptosis: CN III palsy.
- ⬆️ Lid Retraction: Graves’ eye disease.
- 👀 Proptosis: Graves’, orbital tumours, carotid–cavernous fistula, cellulitis.
- 🔴 Red Eye: Conjunctivitis, acute glaucoma, cellulitis, orbital mass.
- ↘️ Enophthalmos: Horner’s syndrome.
🌗 Pupils – Light Reflex
- Bright light → optic nerve → Edinger–Westphal nucleus → bilateral constriction via CN III.
- Check for RAPD (Marcus Gunn pupil 🔦).
- Pathology: Argyll Robertson pupil (accommodates but no light reaction).
📏 Pupils – Accommodation
- Look at distant point → then near (10 cm) → constriction + adduction expected.
- Controlled by frontal lobes, same efferent as light reflex.
🔵 Dilated Pupil
- 💊 Cocaine, adrenaline, anticholinergics.
- CN III palsy with headache → think SAH/PCOMM aneurysm 🚨.
- Holmes–Adie pupil: young women, slow constriction, ↓ reflexes.
⚫ Small Pupil
- Opiates, senile miosis, Horner’s, Argyll Robertson.
- Argyll Robertson pupils: irregular, no light reflex but accommodate → neurosyphilis, diabetes, midbrain tumour.
🐎 Horner’s Syndrome
- Triad: miosis + ptosis + anhidrosis (± enophthalmos).
- Light reflex intact.
- Causes:
- Central: stroke, MS, syrinx.
- Peripheral: Pancoast tumour, carotid dissection, trauma, aortic aneurysm.
📊 Visual Acuity
- Test each eye separately with Snellen chart (record 6/x).
- If no chart → newsprint at 30 cm. Use pinhole if no glasses.
⬇️ Causes of Reduced Acuity
- Cornea (ulcer, oedema), cataract, vitreous haemorrhage.
- Retina (infarct, haemorrhage).
- Optic neuropathy (MS, ischaemia, compression).
- Pathway lesions (stroke, occipital tumour).
🔥 Optic Neuritis
- Loss of vision + painful eye movements + colour desaturation.
- Common in MS. Disc swelling may be seen.
⚪ Optic Atrophy
- Pale disc, ↓ acuity, impaired colour vision.
- Causes: glaucoma, MS, ischaemic neuropathy, trauma, chronic papilloedema, Leber’s hereditary neuropathy.
🔦 RAPD (Relative Afferent Pupillary Defect)
- Swinging torch: affected eye dilates despite light → Marcus Gunn pupil.
👓 Visual Fields
- Screen quadrants by finger movements.
- Left field → right cortex, and vice versa.
📌 Common Visual Field Defects
- 🎯 Tunnel vision → glaucoma, retinitis pigmentosa, papilloedema.
- 🚫 Blind eye → optic nerve/eye pathology.
- ⏸️ Bitemporal hemianopia → pituitary/chiasm lesion.
- ➡️ Homonymous hemianopia → post-chiasmal (stroke, tumour).
🪞 Fundoscopy
- Dark lesions → melanoma, retinitis pigmentosa.
- Macula → cherry-red spot (CRA occlusion).
- Haemorrhages → dot/blot/flame 🔴.
- Optic disc → papilloedema, atrophy, glaucoma cupping.
👁️ Eye Movements
- Pursuit: Smooth following in “H” pattern.
- Saccades: Rapid switching between targets.
🔢 Cranial Nerves III, IV, VI
- CN III (Oculomotor): All except LR + SO → lesion = ptosis, “down & out”, dilated pupil.
- CN IV (Trochlear): SO → lesion = vertical diplopia.
- CN VI (Abducens): LR → lesion = cannot abduct, horizontal diplopia.
⚡ Internuclear Ophthalmoplegia (INO)
- MLF lesion → impaired horizontal gaze coordination.
- Classically in MS, also pontine infarct, diabetes.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
