| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Non invasive ventilation (NIV)
Related Subjects: |Respiratory Failure |Non invasive ventilation (NIV) |Intubation and Mechanical Ventilation |Critical illness neuromuscular weakness |Multiple Organ Dysfunction Syndrome |Haemodialysis |Dobutamine
💡 Key Point: Patients must be conscious and have sufficient respiratory drive to benefit from NIV. 😴 Those who are drowsy or unable to protect their airway may need intubation and invasive ventilation.
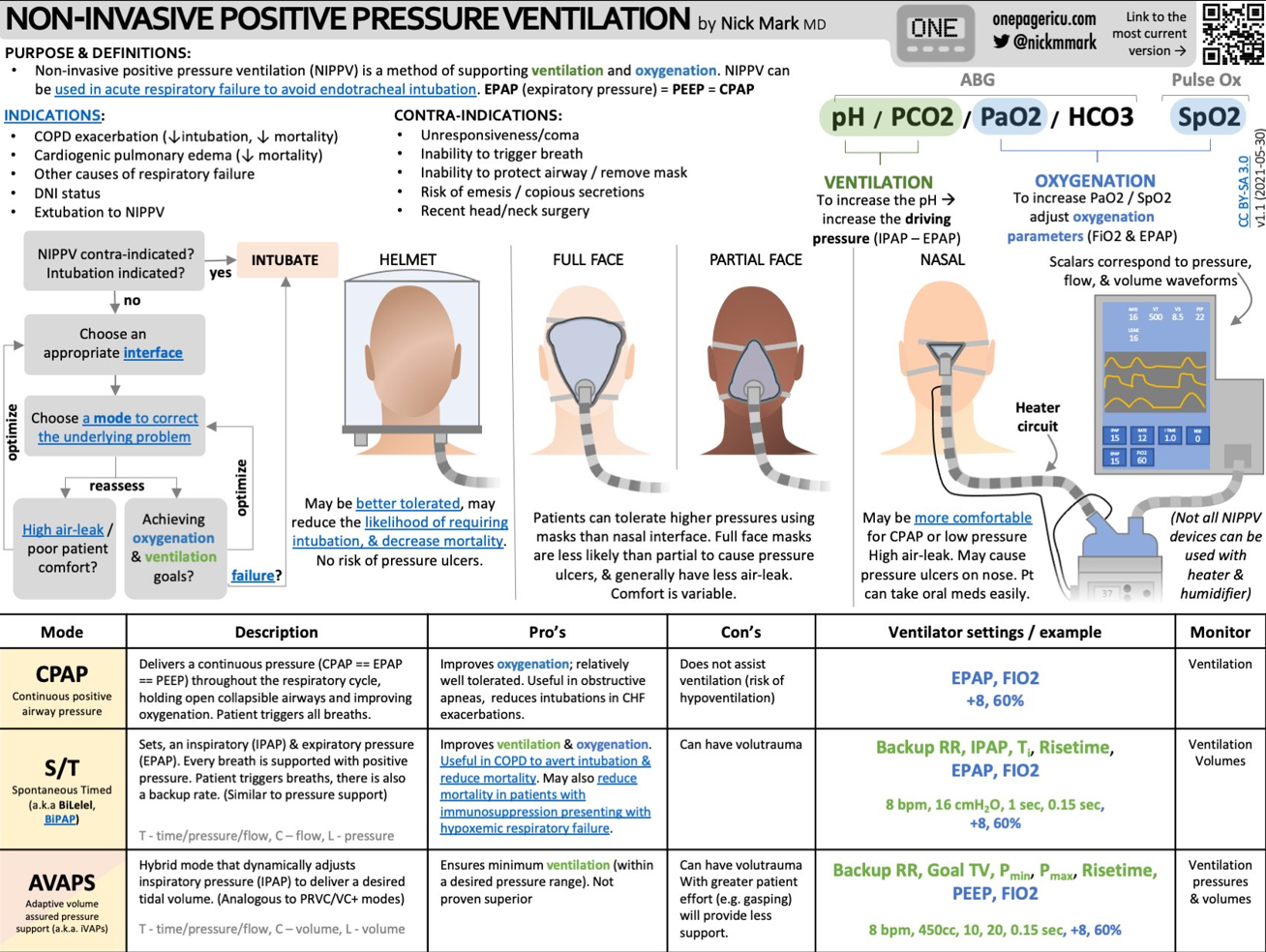
📖 Introduction
- 🫁 Normal breathing uses diaphragm + intercostals → negative intrathoracic pressure → air flows into alveoli.
- 💨 NIV: Tight mask/hood with ventilator provides positive pressure to push air in.
- ⚙️ Modes: CPAP (continuous) or BiPAP (two pressure levels).
- ✅ Benefits: avoids intubation, ↓ mortality, ↓ stay length, ↓ costs. Especially used in Type II RF.
🔄 Types of NIV
- 🌬️ CPAP: Constant pressure through cycle → used in Type I RF (e.g. pulmonary oedema, OSA).
- ↕️ BiPAP: Higher pressure in inspiration (IPAP) + lower in expiration (EPAP). Best for Type II RF with acidosis (e.g. COPD exacerbations).
⭐ Advantages over Invasive Ventilation
- 🛡️ ↓ Ventilator-associated pneumonia.
- 📉 Shorter admission + lower costs.
- 😌 Less sedation required.
- 💨 Particularly effective in COPD & hypercapnic RF.

🩺 Applications
- 👩⚕️ Used in both Type I & II RF: COPD exacerbations, pulmonary oedema, post-op support.
- 🎭 Requires tight-fitting mask + patient cooperation.
- ⚡ Reduces work of breathing, improves gas exchange, recruits alveoli.
- 🏠 Can be given at home or in hospital settings.
✅ Indications
- pH < 7.35 with hypercarbia (Type II RF).
- Cardiogenic pulmonary oedema without shock.
- Immunosuppressed patients with acute RF.
- Weaning support (esp. COPD).
- Post-op RF (e.g. after lung surgery).
- Palliative symptom relief (breathlessness).
⛔ Contraindications
- 🚨 Severe hypoxaemia (< 60 mmHg PaO₂ on 100% FiO₂).
- 😴 GCS < 9 / impaired consciousness.
- ❌ Inability to protect airway / excess secretions.
- 🤕 Facial trauma/burns preventing mask seal.
- 🫧 Untreated pneumothorax.
⚙️ NIV Settings
- BiPAP: Start IPAP 10 cmH₂O, EPAP 4–5 cmH₂O → adjust per ABG/response.
- CPAP: Start 5 cmH₂O → ↑ to 10 if needed.
- 🎯 Aim SaO₂ > 90% or PaO₂ > 60 mmHg with clinical stability.
- ⏳ If no improvement in 4h → consider intubation.
⚠️ Side Effects
- ⬇️ Venous return & CO → hypotension risk.
- 🤢 Gastric distension → discomfort + aspiration risk.
- 😣 Skin breakdown from mask pressure.
🏠 Home NIV
- Consider in chronic RF due to:
- Severe spinal deformity
- Neuromuscular disorders (e.g. DMD, MND)
- Cystic fibrosis
- Central hypoventilation syndrome
- 🌙 Often used overnight → improves sleep quality + daytime function.
🚨 Indications for Intubation
- Respiratory arrest or severe distress unresponsive to NIV.
- Severe hypoxaemia (PaO₂ < 8 kPa despite FiO₂/NIV).
- Persistent hypercapnia/acidosis despite NIV.
- GCS < 9 or unsafe airway.
- Failure to stabilise after 4h NIV trial.
📚 References
3 Clinical Cases — Non-Invasive Ventilation (NIV) 😷💨
- Case 1 — Acute exacerbation of COPD 🫁: A 68-year-old man with known COPD presents with worsening breathlessness, purulent sputum, and confusion. ABG: pH 7.25, PaCO₂ 9.2 kPa, PaO₂ 7.8 kPa on air. He is tachypnoeic and using accessory muscles. Teaching: This is type 2 respiratory failure with acidosis → clear indication for NIV (usually BiPAP). NIV improves alveolar ventilation, lowers CO₂, and reduces need for intubation. Also give controlled O₂ (target sats 88–92%), bronchodilators, steroids, and antibiotics if infective trigger.
- Case 2 — Acute cardiogenic pulmonary oedema ❤️: A 72-year-old woman with hypertension and ischaemic heart disease presents with severe breathlessness, orthopnoea, and pink frothy sputum. O₂ sats 82% on 15 L NRB. CXR: bilateral alveolar shadowing. Teaching: CPAP (continuous positive airway pressure) recruits alveoli, reduces preload/afterload, and improves oxygenation. NIV is often life-saving in acute pulmonary oedema alongside diuretics, nitrates, and treatment of the underlying cause (e.g. ACS, arrhythmia).
- Case 3 — Obesity hypoventilation syndrome (chronic use) ⚖️: A 55-year-old woman with BMI 48 presents with morning headaches, somnolence, and dyspnoea. ABG: pH 7.37, PaCO₂ 8.5 kPa, PaO₂ 7.9 kPa. Overnight oximetry shows desaturation. Teaching: Chronic type 2 respiratory failure due to obesity hypoventilation benefits from long-term nocturnal NIV (BiPAP). This offloads the work of breathing, improves sleep quality, and reduces admissions. Always rule out and treat co-existing OSA.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
