| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Acute Coronary Syndrome (ACS) STEMI
Related Subjects: |Acute Coronary Syndrome: Overview |Atherosclerosis |Ischaemic heart disease |Assessing Chest Pain |Acute Coronary Syndrome (ACS): Complications |ACS - General |ACS - STEMI |ACS - NSTEMI |ACS - GRACE Score |ACS - ECG Changes |ACS -Cardiac Troponins |ACS - Post MI arrhythmias |ACS: Right Ventricular STEMI |ACS: Sgarbossa Criteria |Wellen's syndrome
📊 Initial Management of Acute STEMI
| 🫀 STEMI Management (NICE NG185-aligned summary) |
|---|
🚑 Immediate (do in parallel)
NICE sources: NG185 recommendations | NG185 STEMI visual summary (PDF) |
The ECG + Chest Pain or can be silent is diagnostic

🫀 Management of Acute STEMI (Chest Pain + ECG) — NICE NG185 + ESC 2023 aligned
🚨 Key principle: STEMI is a time-critical reperfusion emergency. Do not delay reperfusion for CXR, routine bloods, or waiting for troponin.
NICE timing logic: offer primary PCI if it can be delivered within 120 minutes of the time fibrinolysis could have been given; otherwise offer fibrinolysis (if within 12 hours and no contraindications).
Time = myocardium ⏱️
⚡ Pathophysiology (why speed matters)
- Cause: usually plaque rupture/erosion → platelet activation + thrombin → acute coronary thrombotic occlusion.
- Wavefront necrosis: infarction spreads from endocardium → epicardium over hours; early reperfusion salvages myocardium and preserves LV function.
- Electrical instability: ischaemia triggers VT/VF risk early; hence monitoring and defib readiness.
🩺 Clinical features (typical + atypical)
- Typical pain: central crushing/tight chest pain >20 min ± radiation to jaw/left arm/neck/back.
- Associated symptoms: dyspnoea, diaphoresis 😰, nausea/vomiting, palpitations, syncope, sense of doom.
- Atypical presentations: older adults, women, diabetes, CKD: dyspnoea, collapse, epigastric discomfort, confusion.
- Examination clues: hypotension/shock, pulmonary oedema, new pansystolic murmur (papillary muscle rupture), bradycardia (inferior/RV MI), arrhythmia.
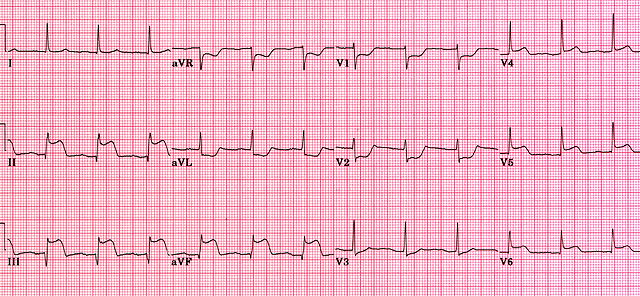
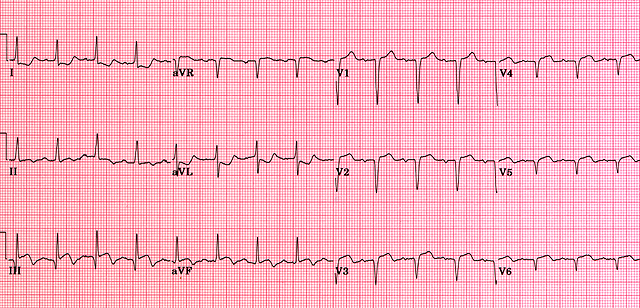
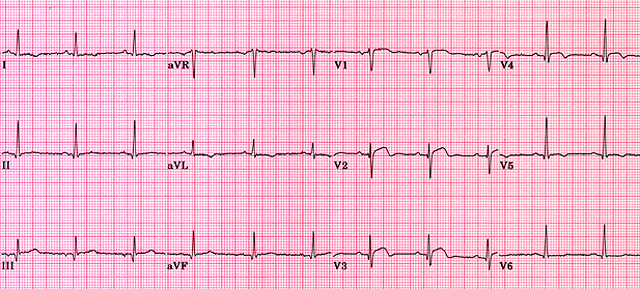
📉 ECG diagnosis (STEMI + STEMI equivalents)
- ST elevation in ≥2 contiguous leads:
- V2–V3: ≥2 mm (men) or ≥1.5 mm (women)
- Other leads: ≥1 mm
- Posterior MI: ST depression V1–V3 with tall R waves → record V7–V9 (posterior ST elevation supports STEMI pathway).
- Right ventricular MI: consider with inferior STEMI + hypotension → record V3R/V4R (avoid nitrates if RV infarct suspected).
- LBBB: new/presumed new LBBB with ischaemic symptoms is high risk; use clinical picture + ECG criteria (e.g., concordant changes) and act early if STEMI suspected.
- Repeat ECGs: if symptoms persist or evolve (dynamic STEMI can be missed on first trace).
🧪 Troponin (do not wait for it)
- Troponin supports diagnosis and risk, but STEMI is a clinical + ECG diagnosis requiring immediate action.
- High-sensitivity troponin typically rises within hours; repeating at 3 hours is useful when ECG is non-diagnostic.
- Bedside echo can help if diagnosis unclear (regional wall motion abnormality), but should not delay reperfusion when STEMI is clear.
🚑 Immediate actions (first 5–10 minutes)
- ABCDE, call cath lab / STEMI pathway early; senior decision-maker involved early.
- Cardiac monitor + defib ready ⚡; treat VT/VF per ALS.
- 12-lead ECG and repeat if evolving; consider posterior/right-sided leads when indicated.
- IV access x2; point-of-care glucose; bloods (FBC, U&E, clotting, troponin) but do not delay reperfusion.
- Oxygen only if hypoxaemic: target 94–98% (or 88–92% if risk of hypercapnic respiratory failure).
- Do not delay reperfusion for CXR unless you strongly suspect dissection/other alternative diagnosis needing immediate imaging.
💊 Symptom relief (analgesia + anti-ischaemic)
- Opioid analgesia: IV morphine/diamorphine titrated to pain, plus antiemetic (e.g., metoclopramide/ondansetron) as needed.
- GTN (sublingual or IV) for ongoing pain and hypertension if no contraindications:
- Avoid in hypotension, suspected RV infarct, severe aortic stenosis, or recent PDE5 inhibitor use.
- Positioning: upright if pulmonary oedema; supine/legs elevated if hypotensive (and treat shock protocol).
🩸 Antiplatelet therapy (NICE NG185)
✅ Core: Aspirin + a P2Y12 inhibitor (dual antiplatelet therapy, DAPT).
NICE specifies prasugrel + aspirin as the preferred option for STEMI undergoing primary PCI in those not on an oral anticoagulant, with age/bleeding cautions.
- Aspirin: 300 mg loading ASAP (chewed/crushed if needed), then 75 mg daily long-term unless contraindicated.
- If primary PCI planned (and not on an oral anticoagulant): offer prasugrel + aspirin.
- Prasugrel cautions: avoid if prior stroke/TIA; consider alternatives if age ≥75 or weight <60 kg (bleeding risk).
- If bleeding risk outweighs benefit (often ≥75): offer ticagrelor or clopidogrel instead (with aspirin).
- If already taking an oral anticoagulant: offer clopidogrel + aspirin (avoid prasugrel/ticagrelor in this setting per NICE pathway).
- If STEMI not treated with primary PCI (including after fibrinolysis): NICE supports ticagrelor + aspirin unless bleeding risk high (then consider clopidogrel + aspirin).
🧬 Antithrombin / anticoagulation (match to strategy — NICE NG185)
- Primary PCI with radial access: offer unfractionated heparin (UFH) with bailout glycoprotein IIb/IIIa inhibitor (not routine upfront).
- If femoral access needed: consider bivalirudin with bailout glycoprotein IIb/IIIa inhibitor.
- If fibrinolysis is given: give an antithrombin at the same time (agent per local protocol).
- Avoid routine pre-hospital fibrinolysis or routine GP IIb/IIIa inhibitor use when primary PCI is planned.
- Renal function: adjust dosing where relevant and monitor bleeding risk closely.
⚡ Reperfusion strategy (NICE NG185 + ESC 2023 framing)
- Primary PCI (preferred): offer coronary angiography with follow-on primary PCI if indicated when:
- presentation is within 12 hours of symptom onset, and
- primary PCI can be delivered within 120 minutes of the time fibrinolysis could have been given.
- Fibrinolysis: offer if within 12 hours and timely primary PCI (as above) is not achievable and no contraindications.
- Cardiogenic shock: offer urgent coronary angiography with follow-on PCI if indicated (within 12 hours; and consider even later if ongoing ischaemia/shock).
- Late presenters (>12 hours): consider angiography/PCI if ongoing ischaemia, haemodynamic instability, malignant arrhythmias, or shock.
- ESC practical emphasis: bypass non-PCI centres where possible; move directly to cath lab in confirmed STEMI to reduce system delay.
💉 If fibrinolysis is used (what to do next — NICE)
- Give antithrombin at the same time as fibrinolysis.
- Repeat ECG at 60–90 minutes after fibrinolysis.
- Failed reperfusion (e.g., persistent ST elevation): offer immediate coronary angiography with follow-on PCI if indicated; do not repeat fibrinolysis.
- Recurrent ischaemia after fibrinolysis: seek urgent cardiology advice and consider angiography/PCI.
- If clinically stable after successful fibrinolysis: consider angiography during the same admission.
🩻 Cath lab / in-hospital strategy (NICE NG185)
- Access: radial preferred when feasible (lower bleeding/vascular complications).
- Stent choice: offer drug-eluting stent if stenting is indicated.
- Multivessel disease:
- If no shock: offer complete revascularisation (often during index admission; may be staged).
- If cardiogenic shock: consider culprit-only revascularisation during index procedure.
- LV function: assess LV function in all STEMI patients (echo before discharge or early follow-up).
🧠 Special situations (high yield)
- Inferior STEMI + hypotension: think RV infarct; record right-sided leads; avoid nitrates; treat with cautious fluids and urgent reperfusion.
- Posterior MI: record V7–V9; treat as STEMI equivalent if posterior ST elevation present.
- Cardiac arrest with ROSC: if ECG/clinical picture suggests acute coronary occlusion, urgent cath lab discussion is warranted (local network protocol).
- Suspected aortic dissection: tearing pain radiating to back, pulse/BP differential, new AR murmur, mediastinal widening — avoid anticoagulants/thrombolysis and image urgently.
💓 Beta-blockers, ACEi/ARB, MRA (inpatient + discharge)
- ACEi/ARB: start when haemodynamically stable, especially with LV dysfunction, anterior MI, diabetes, or hypertension; titrate to target doses.
- Beta-blocker: offer particularly if LV dysfunction or heart failure; avoid/withhold in shock, acute pulmonary oedema, severe bradycardia/heart block, or severe asthma.
- Aldosterone antagonist (eplerenone): consider if LVEF ≤40% with heart failure or diabetes after MI (monitor K+ and renal function closely).
- High-intensity statin: start early unless contraindicated (dose per local post-MI pathway).
🩹 Secondary prevention (what saves lives long-term)
- DAPT: aspirin + P2Y12 inhibitor as directed (often up to 12 months; shorter if bleeding risk high; longer in selected high-ischaemic-risk cases — specialist decision).
- Statin: high-intensity statin long-term; consider add-on lipid therapy in very high risk if targets not met (cardiology/lipid clinic pathway).
- BP, diabetes, smoking: aggressive risk factor control (smoking cessation has one of the biggest absolute benefits).
- Cardiac rehab: structured rehab improves outcomes and adherence; include exercise prescription, education, psychosocial support.
- Vaccination: influenza (and other vaccinations per risk group policy) to reduce infection-triggered events.
📅 Inpatient monitoring and complications to watch for
- Arrhythmias: VT/VF early; AF; bradyarrhythmias (inferior MI); monitor and treat per ALS/cardiology.
- Heart failure / pulmonary oedema: diuretics, nitrates (if BP allows), ventilatory support as needed; assess LVEF.
- Mechanical complications (2–7 days): papillary muscle rupture (acute MR), VSD, free wall rupture (tamponade); suspect if sudden shock/new murmur.
- Pericarditis: pleuritic pain, pericardial rub (early); Dressler syndrome later.
📊 “Risk stratification” (use the right tools)
- Reperfusion decisions in STEMI are ECG + time + clinical status driven (not GRACE/TIMI).
- After reperfusion, prognosis is guided by:
- Killip class / heart failure severity
- LVEF (echo)
- Extent of coronary disease and success of revascularisation
- Bleeding risk, renal function, frailty, and complications during admission
- GRACE is primarily a NSTEMI/UA risk tool and is not the main determinant for acute STEMI reperfusion.
💡 Teaching pearl: A “normal” early troponin and a “normal” early CT head/chest X-ray do not exclude STEMI. The life-saving decision is whether the ECG/clinical picture demands immediate reperfusion.
📚 References (guidelines)
- NICE NG185: Acute coronary syndromes (overview)
- NICE NG185: Recommendations (STEMI pathway, antiplatelets, anticoagulation, reperfusion timings)
- NICE NG185: STEMI visual summary (PDF)
- ESC 2023 Guidelines: Acute Coronary Syndromes (ACS) (includes STEMI and NSTE-ACS)
- ESC 2023 ACS Guidelines (Eur Heart J) — PubMed record
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
