| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Penicillin Allergy
🧪 Penicillin allergy is often reported but rarely true: Around 10% of patients claim an allergy, yet <1% are truly allergic. Mislabeling leads to use of broader-spectrum, more toxic, and more expensive antibiotics, increasing risks of antimicrobial resistance and Clostridioides difficile infection.
- 🤔 Many “allergies” are side effects (e.g., nausea, vomiting) or viral rashes (e.g., amoxicillin + EBV infection) — not true allergies.
- ⌛ Sensitivity wanes: 50% lose penicillin allergy in 5 years, 80% in 10 years.
- 👶 Childhood penicillin “allergy” rarely persists into adulthood.
- 🔄 Cross-reactivity with cephalosporins is low (1–2%); most patients tolerate them.
- 🧪 Patients with mild, delayed reactions >10 years ago may be candidates for oral rechallenge under supervision.
- ✅ Careful assessment can often safely remove the penicillin allergy label.
- 💊 β-lactam allergies are the most common immune-mediated drug reactions encountered in clinical practice.
Taking a History of Penicillin Allergy
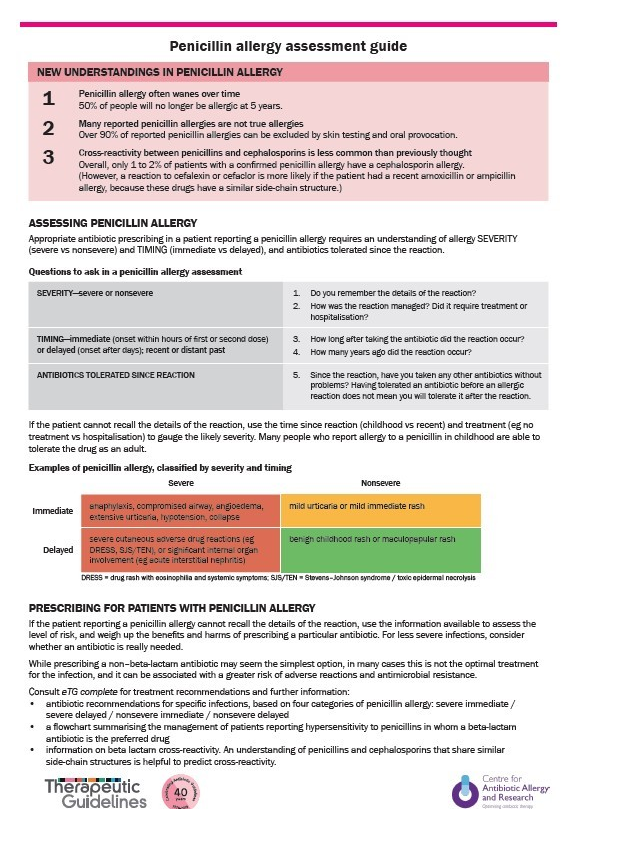
When a patient reports penicillin allergy, key questions include:
- 📜 Previous Reactions: Which antibiotics caused problems?
- 💊 Tolerated Antibiotics: Any β-lactams tolerated since?
- 🕒 Timing: How long ago did the reaction occur?
- ⚠️ Nature of Reaction: Was it diarrhoea, rash, swelling, breathing difficulty?
- 🎨 Rash Details: What type (maculopapular, urticarial, bullous)? Could it have been viral?
- ⏳ Onset: Minutes/hours (immediate IgE-mediated) vs days (delayed).
- 📍 Reason for antibiotic: Was it for a throat infection, skin infection, etc.?
- 🏥 Severity: Did it need hospitalisation or ICU?
- ✅ Resolution: Did it stop once the drug was discontinued?
- 📚 Sources: Ask patient, carers, GP, and check records.
Risk Stratification
- 🚨 Immediate reactions (minutes–hours, IgE-mediated): urticaria, angioedema, bronchospasm, hypotension, anaphylaxis.
- 📆 Delayed reactions (days–weeks, T-cell mediated): morbilliform rash, serum sickness, Stevens-Johnson syndrome.
- 🔑 Differentiation matters: delayed mild rashes often allow safe future use under supervision.
📝 Exam pearl: Only 1 in 10 patients labelled as penicillin allergic are truly allergic. Always clarify the history before defaulting to alternatives.
Assessment and Management
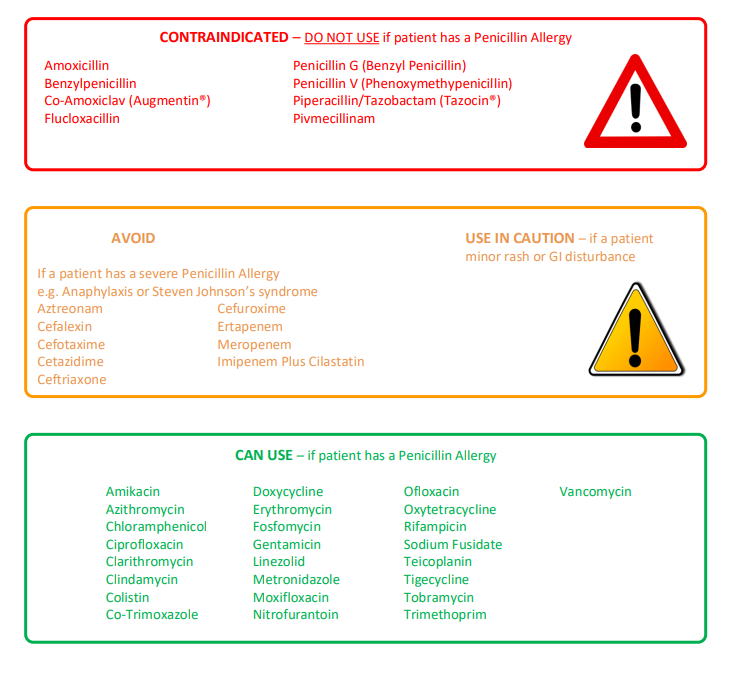
Understanding β-lactam classification helps guide safe prescribing:
- 🔴 Penicillins: Avoid in true allergy.
- 🟠 Other β-lactams (cephalosporins, carbapenems): Usually tolerated in mild allergy; caution in severe IgE-mediated cases.
- 🟢 Non-β-lactams: Always safe regardless of allergy history.
🌟 Delabelling strategies: Allergy testing (skin/IgE) and supervised oral challenge can safely remove false penicillin allergy labels, improving antibiotic stewardship.
Clinical Consequences of a False Allergy Label
- 💷 More expensive antibiotic prescriptions
- 🦠 Broader-spectrum antibiotics → antimicrobial resistance
- ⚠️ Higher rates of C. difficile infection
- ⏱️ Longer hospital stays & higher complication rates
References
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
