| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Anatomy and Physiology of the Parathyroid Gland
Related Subjects: |PTH Physiology |Calcium Physiology |Magnesium Physiology |Calcitonin |Hypocalcaemia |Hypercalcaemia |Hypomagnesaemia |Hypermagnesaemia |Primary Hyperparathyroidism |Familial hypocalciuric hypercalcaemia (FHH) |Sarcoidosis |Anatomy and Physiology of the Thyroid |Anatomy and Physiology of the Parathyroid
The parathyroid glands are small but vital endocrine organs responsible for maintaining calcium–phosphate homeostasis through secretion of parathyroid hormone (PTH). Tight regulation of extracellular calcium is essential for neuromuscular excitability, cardiac conduction, coagulation, and skeletal integrity.
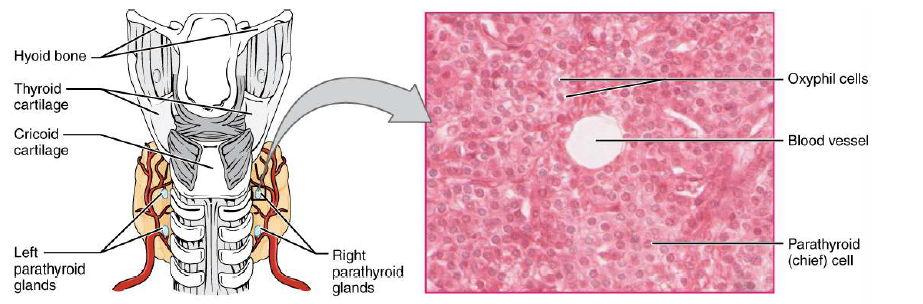
1️⃣ Gross Anatomy
- Number: Usually four glands (2 superior, 2 inferior).
- Size: ~3–5 mm; each weighs 30–60 mg.
- Colour: Yellow-brown (due to fat content).
- Location: Posterior surface of thyroid lobes, near upper and lower poles.
- Variability: Highly variable position → important in surgery.
📍 Ectopic Locations
- Mediastinum
- Thymus
- Carotid sheath
- Intrathyroidal
Ectopic locations are explained by embryological migration and are a major cause of failed parathyroid surgery.
2️⃣ Embryology
- Superior glands: Derived from 4th pharyngeal pouch.
- Inferior glands: Derived from 3rd pharyngeal pouch (descend with thymus).
Because inferior glands migrate further, they are more commonly ectopic.
3️⃣ Histology and Cellular Structure
- Chief Cells (main functional cells):
- Produce and secrete PTH.
- Contain CaSR (calcium-sensing receptors).
- Oxyphil Cells:
- Larger, eosinophilic cells.
- Function unclear (likely metabolic/mitochondrial role).
- Increase with age.
- Adipocytes:
- Increase with age.
- Explain yellow appearance.
4️⃣ Blood Supply and Innervation
🩸 Vascular Supply
- Primarily from inferior thyroid artery.
- Additional branches from superior thyroid artery.
- Venous drainage → thyroid plexus → internal jugular vein.
🧠 Innervation
- Autonomic fibres from cervical sympathetic chain.
- No direct neural control of secretion (hormonal control dominates).
5️⃣ Parathyroid Hormone (PTH): Synthesis and Secretion
PTH is an 84–amino acid peptide hormone that acts within minutes to hours to regulate calcium balance.
🧪 Synthesis
- Prepro-PTH → Pro-PTH → Active PTH.
- Occurs in rough ER and Golgi of chief cells.
- Stored in secretory granules.
🔄 Secretion Control
- Controlled by extracellular Ca²⁺ concentration.
- Mediated via CaSR on chief cells.
| Serum Calcium | CaSR Activity | PTH Secretion |
|---|---|---|
| Low | Reduced | Increased |
| Normal | Moderate | Basal |
| High | Activated | Suppressed |
6️⃣ Physiological Actions of PTH
PTH acts on bone, kidney, and indirectly intestine to increase serum calcium and reduce phosphate.
🦴 A) Bone
- PTH does NOT act directly on osteoclasts.
- Stimulates osteoblasts → ↑ RANKL → activates osteoclasts.
- Result → bone resorption.
- Releases Ca²⁺ and PO₄³⁻ into circulation.
Intermittent low-dose PTH stimulates bone formation (basis of teriparatide therapy in osteoporosis).
🩸 B) Kidneys
- ↑ Calcium reabsorption (distal tubule).
- ↓ Phosphate reabsorption (proximal tubule).
- ↑ 1α-hydroxylase activity → ↑ calcitriol.
🍽️ C) Intestine (Indirect)
- Via calcitriol (1,25-dihydroxyvitamin D).
- ↑ Ca²⁺ and phosphate absorption.
7️⃣ Integrated Calcium–Phosphate Homeostasis
Calcium regulation depends on interaction between PTH, vitamin D, kidneys, bone, and intestine.
| Hormone | Bone | Kidney | Intestine |
|---|---|---|---|
| PTH | ↑ Resorption | ↑ Ca²⁺, ↓ PO₄³⁻ | Indirect ↑ Ca²⁺ |
| Vitamin D | Mineralisation | ↑ Ca²⁺ | ↑ Ca²⁺/PO₄³⁻ |
| Calcitonin | ↓ Resorption | Minor | Minor |
8️⃣ Regulation of PTH
- Calcium: Primary regulator (via CaSR).
- Vitamin D: Suppresses PTH gene transcription.
- Phosphate: Indirect stimulation.
- Magnesium: Required for PTH release (severe deficiency → functional hypoparathyroidism).
9️⃣ Clinical Disorders
📈 Hyperparathyroidism
Primary
- Cause: adenoma (≈85%), hyperplasia, carcinoma.
- Labs: ↑ Ca²⁺, ↓ PO₄³⁻, ↑ PTH.
- Symptoms: “stones, bones, groans, psychiatric overtones”.
Secondary
- Usually due to chronic kidney disease.
- Mechanism: ↓ calcitriol + ↑ phosphate → hypocalcaemia.
- Labs: ↓/normal Ca²⁺, ↑ PO₄³⁻, ↑ PTH.
Tertiary
- Autonomous PTH secretion after prolonged secondary disease.
- Hypercalcaemia + very high PTH.
📉 Hypoparathyroidism
- Post-surgical (most common).
- Autoimmune.
- DiGeorge syndrome.
Features
- Tetany
- Perioral numbness
- Carpopedal spasm
- Seizures
- Prolonged QT
Chvostek’s and Trousseau’s signs reflect neuromuscular hyperexcitability from hypocalcaemia.
🔬 10️⃣ Diagnosis
- Serum Ca²⁺ (total + corrected).
- Ionised calcium.
- PTH.
- Phosphate.
- Vitamin D.
Imaging
- Neck ultrasound.
- Sestamibi scan.
- 4D-CT (specialist).
💊 11️⃣ Management
Hyperparathyroidism
- Parathyroidectomy (definitive).
- Cinacalcet (calcimimetic).
- Hydration + bisphosphonates (acute hypercalcaemia).
Hypoparathyroidism
- Oral calcium.
- Calcitriol / alfacalcidol.
- Magnesium replacement.
12️⃣ Key Exam & Clinical Pearls
- Low Ca²⁺ + high PTH = secondary hyperparathyroidism.
- High Ca²⁺ + high PTH = primary/tertiary.
- Post-thyroidectomy hypocalcaemia → check PTH urgently.
- CKD = most common cause of secondary disease.
- CaSR mutations → familial hypocalciuric hypercalcaemia.
✅ Summary
The parathyroid glands regulate extracellular calcium through secretion of PTH. PTH raises serum calcium by stimulating bone resorption, enhancing renal reabsorption, and increasing vitamin D activation. Disorders produce characteristic biochemical patterns and systemic effects, especially on bone, kidneys, and neuromuscular function. Understanding parathyroid anatomy and physiology is essential for managing hypercalcaemia, hypocalcaemia, and metabolic bone disease.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
