| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Accelerated Idioventricular Rhythm
🫀 Accelerated Idioventricular Rhythm (AIVR) is a transient ventricular rhythm often seen post-MI, particularly during reperfusion. It is usually benign, self-limiting, and haemodynamically well tolerated, so treatment is rarely required. The key challenge is distinguishing it from slow VT or CHB.
📖 About
- Commonly observed after reperfusion in acute MI (PCI or thrombolysis).
- Often resembles a "slow VT" but is not typically malignant.
- Most cases resolve spontaneously as sinus rate accelerates past the ventricular focus.
- Generally requires only observation and reassurance unless instability develops.
📊 ECG Characteristics
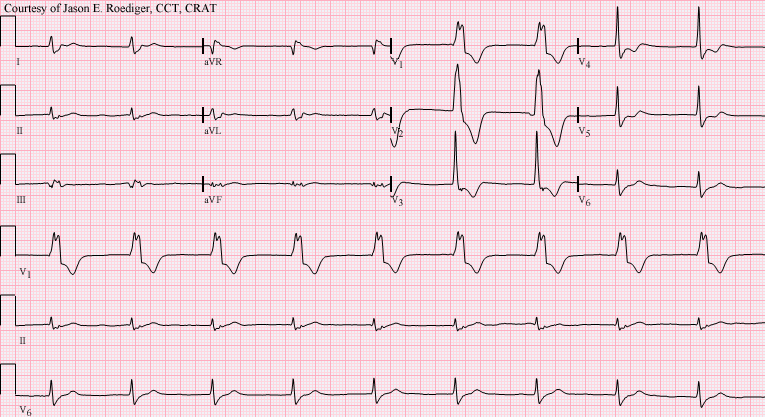
- Broad-complex rhythm, usually regular.
- Rate: 40–120 bpm (classic: 60–100). 🕒
- AV dissociation often present (cannon A waves may be seen clinically).
- At rates >110–120 bpm, consider slow VT instead.
🧾 Differential Diagnosis
- CHB with escape rhythm: if rate <50 bpm.
- Slow VT: if rate >110–120 bpm, particularly in scarred ventricles.
- Junctional rhythm with aberrancy: consider if QRS morphology varies.
⚠️ Causes / Associations
- 💔 Acute STEMI, especially reperfusion arrhythmia.
- Ischaemic heart disease, cardiomyopathy.
- Myocarditis, digoxin toxicity (check K⁺ and drug levels).
- Cocaine use.
- Normal finding in well-trained athletes (high vagal tone).
- During ROSC after cardiac arrest.
🩺 Clinical Features
- Often asymptomatic, may have variable heart sounds due to AV dissociation.
- Seen in acute MI context → always check for associated complications.
- Usually haemodynamically stable (key teaching pearl: instability is unusual).
💊 Management
- Observation only in most cases – treat the underlying condition (e.g., MI).
- Spontaneously resolves once sinus node regains dominance.
- Do NOT suppress with antiarrhythmics (lidocaine, amiodarone) unless unstable – risk of asystole ⚠️.
- Seek senior input if in doubt, particularly in the peri-MI setting.
📚 References
Cases - Accelerated Idioventricular Rhythm (AIVR)
- Case 1 - Post-Reperfusion MI: A 58-year-old man is admitted with an acute anterior STEMI. He undergoes primary PCI with stenting of the LAD. An hour later, telemetry shows a wide-complex rhythm at 70 bpm with gradual onset and offset. He is asymptomatic, BP stable, and the rhythm spontaneously reverts to sinus. Diagnosis: AIVR following reperfusion therapy for MI. Management: No treatment needed - benign rhythm. Monitor and continue post-MI care (dual antiplatelets, beta-blocker, ACEi, statin).
- Case 2 - Digoxin Toxicity: A 72-year-old woman with atrial fibrillation on digoxin presents with nausea and visual halos. ECG: regular wide-complex rhythm at 60 bpm, independent of atrial activity. Serum digoxin level high. Diagnosis: AIVR associated with digoxin toxicity. Management: Stop digoxin, correct electrolytes (especially potassium and magnesium), consider digoxin-specific antibody fragments if severe. Continuous cardiac monitoring until rhythm resolves.
Teaching Commentary ⚡
AIVR is a ventricular rhythm faster than the intrinsic ventricular escape rate (≈40 bpm) but slower than VT (usually 50–110 bpm). It typically occurs after reperfusion of acute MI (a “reperfusion arrhythmia”), but also in drug toxicity (digoxin), cardiomyopathy, and metabolic disturbances. ECG shows a regular, wide-complex rhythm with gradual onset/offset. Unlike VT, AIVR is benign and self-limiting, rarely requiring treatment. Management is to treat the underlying cause (e.g. reperfusion, stop digoxin, correct electrolytes) rather than antiarrhythmics.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
