| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Urinary tract calculi (stones)
Urinary tract stones are crystalline mineral deposits that form in the kidneys and may migrate into the ureters, causing obstruction. Stones <5 mm (especially distal ureteric) usually pass spontaneously within 4 weeks. Stones 5–10 mm may pass with medical expulsive therapy (MET) such as Tamsulosin 400 μg OD. Larger stones (>10 mm) often need surgical intervention.
📖 About
- Renal colic: Acute, severe, intermittent flank/loin pain caused by obstruction of urine flow, typically radiating “loin to groin”.
- Ureteric colic: Pain radiating to groin, scrotum, labia, or inner thigh due to stone migration.
- Common surgical referral. Always exclude other serious causes (e.g. ruptured AAA, appendicitis).
📊 Epidemiology
- Annual incidence: 1–2 per 1000 people; lifetime risk ~10–15%.
- Peak: men aged 20–50; men affected 2–3× more than women.
- Recurrence rate: 30–50% within 10 years.
🧬 Pathophysiology of Pain
- Stone obstructs urinary flow → ↑ intraluminal pressure → stretching of renal capsule and ureteric wall.
- Stimulates prostaglandin release → smooth muscle spasm and vasodilation.
- Results in severe, colicky pain + nausea/vomiting via vagal stimulation.
⚠️ Causes of Renal/Ureteric Obstruction
- Renal calculus (most common)
- Sloughed papilla (e.g. papillary necrosis in diabetes, sickle cell)
- Blood clot (trauma, renal tumour)
- Ureteric stricture or PUJ obstruction
- Rare: tumour, foreign body
🧪 Types of Stones
- 🧂 Calcium oxalate/phosphate (70–80%): Hypercalciuria, hyperoxaluria, hyperparathyroidism.
- 🦠 Struvite (Mg ammonium phosphate): Infection with urease-producing bacteria (Proteus, Klebsiella).
- 🧬 Cystine stones: Due to cystinuria, rare, recurrent, often large.
- 💡 Urate stones: Idiopathic, gout, hyperuricosuria, chemotherapy (tumour lysis).
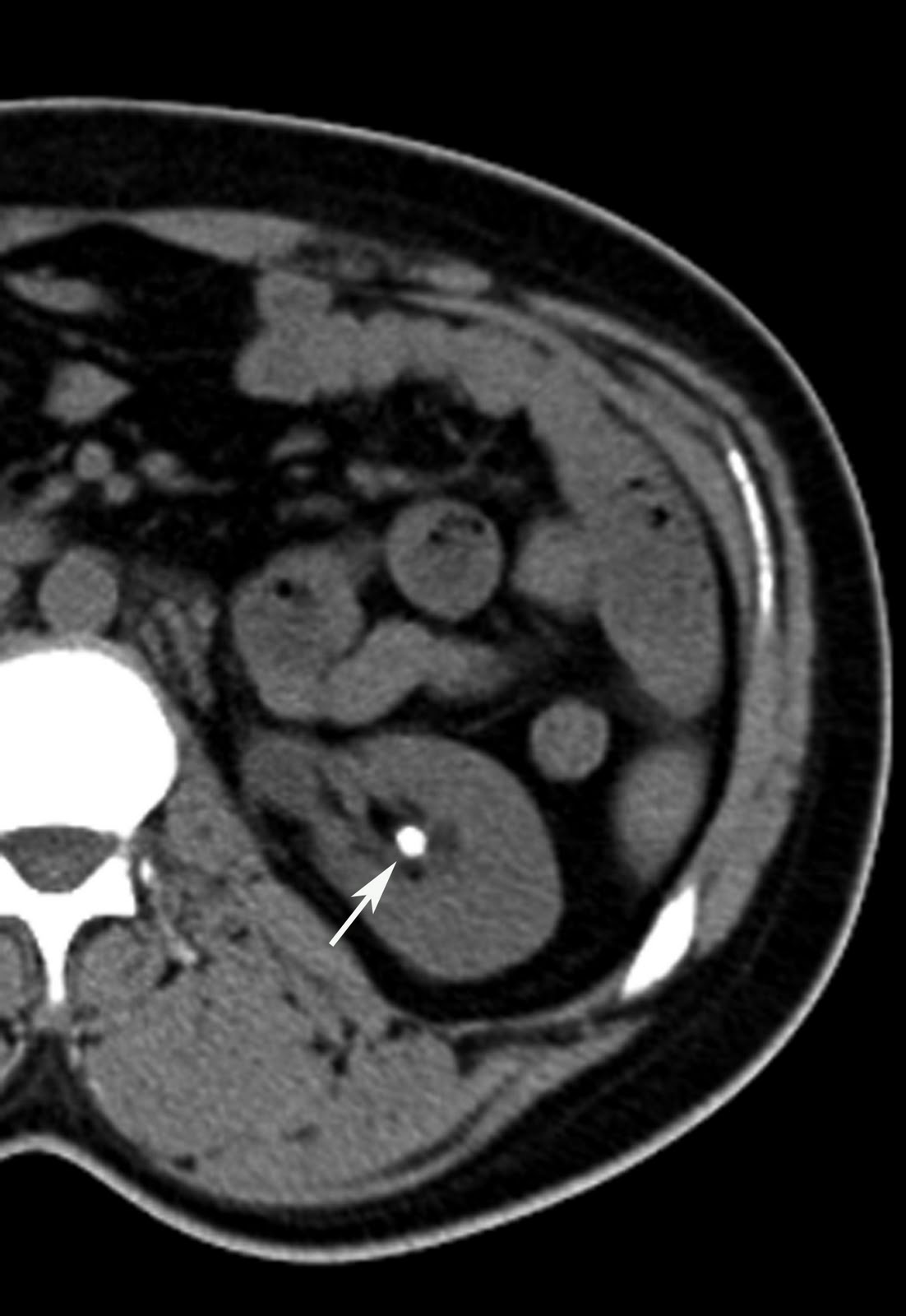
📸 Images

🎯 Risk Factors
- Chronic dehydration, hot climates
- Family history of stones
- Metabolic: hyperparathyroidism, gout, obesity
- GI disease: Crohn’s, ileal resection, malabsorption
- Medications: protease inhibitors, acetazolamide, loop diuretics, topiramate
- Diet: high sodium, animal protein, vitamin C/D excess
🩺 Clinical Features
- Pain: Sudden, severe, colicky, radiates loin → groin/scrotum/labia.
- Behaviour: Patients restless, unable to lie still (contrast with peritonitis).
- Haematuria (microscopic or macroscopic).
- Lower urinary tract symptoms (frequency, hesitancy, weak stream).
- Fever, rigors, tachycardia, hypotension → red flag for urosepsis.
- Nausea, vomiting, ileus.
🧾 History to Elicit
- Past episodes of stones or UTI.
- Family history of nephrolithiasis.
- History of fractures, immobility (hypercalciuria).
- Dietary intake: milk/alkali, high salt, vitamin supplements.
- Medications (esp. antiretrovirals, diuretics, antiepileptics).
🔎 Investigations
- Bloods: FBC, U&E, Ca, phosphate, urate, PTH, CRP, glucose.
- Urinalysis: Haematuria (80–90%), pyuria ± bacteriuria if infected.
- Imaging:
- CT KUB (non-contrast): Gold standard, >95% sensitive; perform within 24 h (ambulatory if stable).
- USS: First-line in pregnancy, children, young adults.
- Plain KUB X-ray: Limited (misses urate/cystine stones), but useful for follow-up.
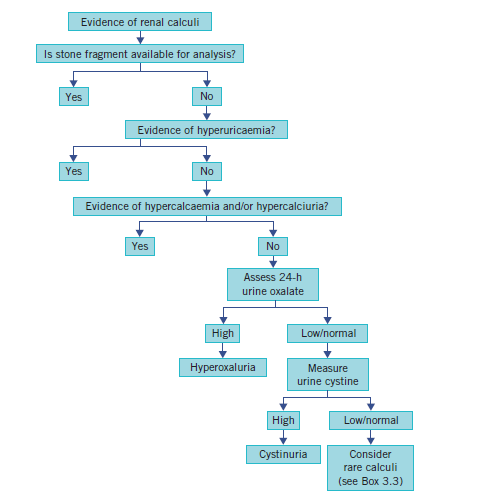
- Stone analysis: All passed/removed stones should undergo biochemical analysis.
- 24h urine collection: Assess calcium, oxalate, urate, citrate, cystine (recurrent formers).
🧾 Differential Diagnosis
- Abdominal aortic aneurysm (AAA) – MUST exclude.
- Appendicitis.
- Diverticulitis.
- Gynaecological causes: ovarian torsion, ectopic pregnancy.
🚑 Indications for Admission
- Sepsis/urosepsis (fever, hypotension, rigors).
- Uncontrolled pain or vomiting.
- Solitary kidney or transplanted kidney.
- Worsening renal function/AKI.
- Diagnostic uncertainty (AAA, appendicitis).
- Suspected bilateral obstruction.
💊 Management
- Supportive:
- Analgesia: NSAIDs (diclofenac 75 mg IV/PR) are first-line; opioids second-line if NSAIDs contraindicated.
- IV fluids: 2L/day if dehydrated or vomiting.
- Antiemetics: ondansetron, cyclizine.
- Medical expulsive therapy (MET):
- Tamsulosin 400 μg OD for distal ureteric stones ≤10 mm.
- Increases stone passage rates and reduces analgesic requirements.
- Indications for urgent urology: sepsis + obstruction → nephrostomy or ureteric stent.
- Observation (watchful waiting): stones <5 mm likely to pass; larger stones may be trialled if pain controlled.
🔨 Surgical Treatment
- ⚡ Shockwave lithotripsy (SWL): Non-invasive, outpatient; fragments stones with shockwaves.
- 🔍 Ureteroscopy (URS): Endoscopic laser fragmentation + retrieval.
- 🩻 Percutaneous nephrolithotomy (PCNL): For large (>20 mm) or staghorn calculi.
- ✂️ Open/laparoscopic surgery: Rare; reserved for complex or failed minimally invasive options.
🛡️ Prevention
- Hydration: target urine output 2–3 L/day.
- Dietary: reduce salt/protein, normal calcium intake, avoid cola (phosphoric acid), add citrus (↑ citrate, alkalinises urine).
- Specific:
- Potassium citrate for recurrent calcium oxalate stones with hypocitraturia.
- Thiazides for recurrent calcium stones with hypercalciuria (with low Na diet).
- Allopurinol for uric acid stones with hyperuricosuria.
- Address underlying causes: hyperparathyroidism, metabolic disorders.
📚 References
- NICE CKS: Acute Renal/Ureteric Colic
- Campbell-Walsh Urology, 12th Edition
- Bailey & Love’s Short Practice of Surgery, 28th Edition
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
