| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Acute Glaucoma
Related Subjects: |Episcleritis |Scleritis |Assessing a Red eye |Acute Angle Closure Glaucoma |Allergic and Infective Conjunctivitis |Anterior and Posterior Uveitis |Herpes simplex keratitis (HSK)
Acute Angle Closure Glaucoma (AACG) is a true ophthalmic emergency 🚨. A sudden rise in intraocular pressure (IOP) causes severe ocular pain, visual loss, and systemic upset. If untreated, optic nerve damage and permanent blindness may occur within hours to days.
📖 About
- Caused by pupillary block in predisposed eyes with shallow anterior chambers → iris bows forward → blocks aqueous outflow.
- Often triggered by pupillary dilation (dim light 🌙, stress, drugs such as anticholinergics or sympathomimetics).
- Rare after cataract surgery (lens removal deepens the chamber).
- “Golf ball hardness” globe on palpation = classic bedside clue.
- More common in older females (narrower anterior chambers).
🧬 Aetiology & Pathophysiology
- Pupillary block: aqueous humour cannot pass through pupil → pressure gradient pushes iris forward → trabecular meshwork blocked → IOP rises.
- Precipitating factors:
- Dim light → physiological mydriasis.
- Drugs: anticholinergics (atropine, tricyclics), sympathomimetics (decongestants), topiramate.
- Emotional stress.
- Prolonged high IOP → ischaemic optic neuropathy → irreversible vision loss.
📊 Epidemiology
- Incidence: ~1 in 1,000 White, 1 in 100 Asian, up to 4 in 100 Inuit populations.
- Age: typically >60 years.
- Sex: female > male (~4:1).
- Risk factors: hyperopia, family history, shallow anterior chamber (short axial length).
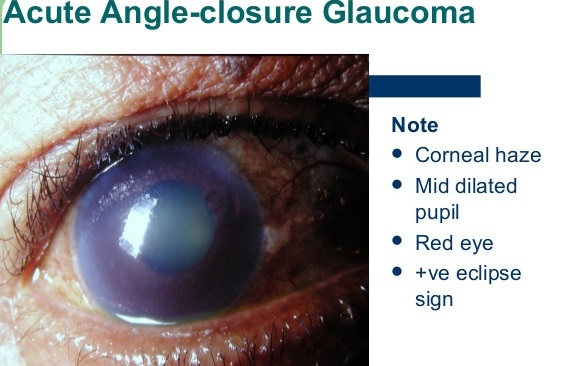
🩺 Clinical Features
- ⚡ Sudden severe ocular pain + headache.
- 🌈 Blurred vision, halos around lights.
- 👁️ Red eye with mid-dilated, fixed pupil.
- 🥴 Nausea, vomiting, systemic upset (can mimic GI pathology).
- 🌫️ Corneal edema (“steamy cornea”).
- IOP usually >40 mmHg (normal 10–21).
🔎 Differential Diagnosis of a Painful Red Eye
| Condition | Features | Distinguishing Points |
|---|---|---|
| AACG | Sudden pain, halos, mid-dilated pupil, hazy cornea, hard globe | Systemic upset (nausea/vomiting), halos 🌈 |
| Anterior Uveitis | Pain, photophobia, small irregular pupil | Pupil constricted, no halos, responds to steroids |
| Keratitis | Red, gritty eye, photophobia | Contact lens use, fluorescein staining shows ulcer |
| Conjunctivitis | Red, sticky eye, mild discomfort | No vision loss, globe not hard |
🧪 Investigations
- Tonometry: IOP usually >40–70 mmHg.
- Slit-lamp: Corneal edema, shallow chamber, fixed pupil.
- Gonioscopy: Closed anterior chamber angle.
- Visual fields: For long-term glaucomatous damage monitoring.
🚑 Stepwise Management
- Immediate (ED/GP setting)
- IV Acetazolamide 500 mg stat (carbonic anhydrase inhibitor).
- Topical Timolol 0.5% (beta-blocker) – reduces aqueous production.
- Analgesia + antiemetics for distress.
- O₂ if hypoxic.
- Next (once IOP begins to fall)
- Pilocarpine 2% drops – miotic → pulls iris away from angle.
- IV Mannitol 20% if refractory to initial measures.
- Definitive
- Laser peripheral iridotomy (LPI) in affected + fellow eye (prophylaxis).
- Surgical iridectomy if LPI unavailable.
🧾 Clinical Pearls
- Any elderly patient with sudden red eye + vomiting → assume AACG until proven otherwise.
- Never dilate pupils if AACG is suspected ❌.
- Fellow eye must always be treated prophylactically with iridotomy.
- Digital palpation: AACG feels like a “rock-hard” eye 🎾.
🖼️ Key Illustrations

💡 Teaching Pearl: AACG is one of the few causes of a painful red eye with systemic upset. Always compare to anterior uveitis (small irregular pupil) and keratitis (corneal ulcer in contact lens wearers). Rapid recognition + immediate acetazolamide + ophthalmology referral = sight-saving intervention.
Cases — Acute Angle-Closure Glaucoma (AACG)
- Case 1 — Classic sudden attack 👁️: A 64-year-old woman presents with sudden severe right eye pain, blurred vision, and halos around lights. She has nausea and vomiting. Exam: red eye with hazy cornea, fixed mid-dilated pupil, hard globe. Intraocular pressure (IOP): 56 mmHg. Diagnosis: acute angle-closure glaucoma. Managed with immediate IV acetazolamide, topical beta-blocker, pilocarpine, and urgent ophthalmology referral for laser iridotomy.
- Case 2 — Triggered by dark environment 🌙: A 58-year-old man develops severe eye pain and headache after spending several hours in a cinema. Exam: conjunctival injection, cloudy cornea, fixed semi-dilated pupil. Diagnosis: AACG precipitated by pupillary dilation in dark. Managed with emergency IOP-lowering drops and definitive laser peripheral iridotomy to both eyes (prophylactic in fellow eye).
- Case 3 — Subacute/recurrent AACG ⚠️: A 62-year-old woman presents with intermittent blurred vision, halos, and mild ocular pain after reading for long periods. Episodes resolve spontaneously but recur. Exam between episodes: shallow anterior chamber, narrow drainage angle on gonioscopy. Diagnosis: subacute angle-closure glaucoma. Managed with prophylactic laser peripheral iridotomy to prevent a full-blown acute attack.
Teaching Point 🩺: AACG occurs when the trabecular meshwork is suddenly blocked by the iris, rapidly raising IOP. Symptoms: sudden eye pain, blurred vision, halos, headache, nausea/vomiting. Signs: red eye, hazy cornea, mid-dilated fixed pupil, hard globe, very high IOP. Risk factors: hypermetropia, older age, female sex, Asian ethnicity, pupillary dilation. Management: emergency IOP-lowering (acetazolamide, beta-blocker, pilocarpine, mannitol) and definitive laser iridotomy.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
