| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Trauma Physiology
Related Subjects:
|High Altitude Physiology
|Diving Physiology
|Trauma Physiology
|Exercise Physiology
|Gastric Physiology
|Rectal Physiology
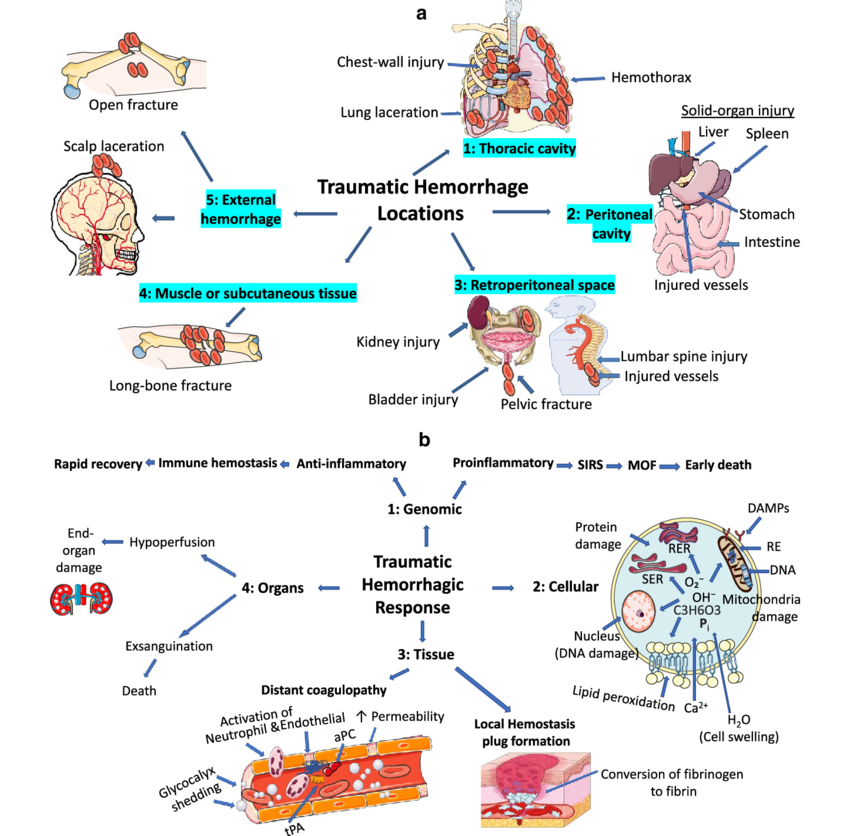
🩸 Trauma physiology examines how the body responds to severe injury.
Understanding these responses is crucial for effective trauma care: stabilising vital functions, preventing secondary injury, and optimising recovery.
Trauma physiology integrates shock, inflammation, and metabolic stress.
Effective care requires rapid resuscitation, vigilant monitoring of organ systems, and multidisciplinary rehabilitation.
A trauma team must anticipate complications early — survival depends on recognising patterns of physiology as much as on treating the injuries themselves.
⚡ Physiological Responses to Trauma
🕑 Phases of Trauma Response
🫁 Key Organ Systems Affected
🛠️ Trauma Assessment & Management
⚠️ Complications
💪 Recovery & Rehabilitation
📌 Summary
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
