| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Osteogenic sarcoma (Osteosarcoma)
🦴⚡ Osteosarcoma is the most common primary malignant bone tumour of adolescence. It is radio-resistant ❌, so radiotherapy is usually not part of the treatment plan.
📖 About
- Most common primary malignant bone tumour in adolescents & young adults (peak age 15–18).
- Arises in the metaphysis of long bones near growth plates (rapid growth zones during puberty).
- Produces immature bone (osteoid) as its pathological hallmark.
- Most common sites: distal femur, proximal tibia, proximal humerus.
🧬 Aetiology & Genetics
- Genetic predisposition:
- Li-Fraumeni syndrome (TP53 mutation) 🧬
- Hereditary retinoblastoma (RB1 gene) 👁️
- Other associations:
- Paget’s disease of bone (older adults) 🦴
- Prior exposure to ionising radiation ☢️
- Pathology: malignant cells producing disorganised osteoid → bone destruction & replacement.
🩺 Clinical Features
- Persistent, progressive pain (often worse at night) 😣.
- Swelling & tenderness around the joint.
- Palpable, firm mass in advanced cases.
- Restricted joint movement; limp if lower limb affected.
- Pathological fracture due to weakened bone 🦴💥.
- Systemic symptoms (weight loss, fever, malaise) usually appear late.
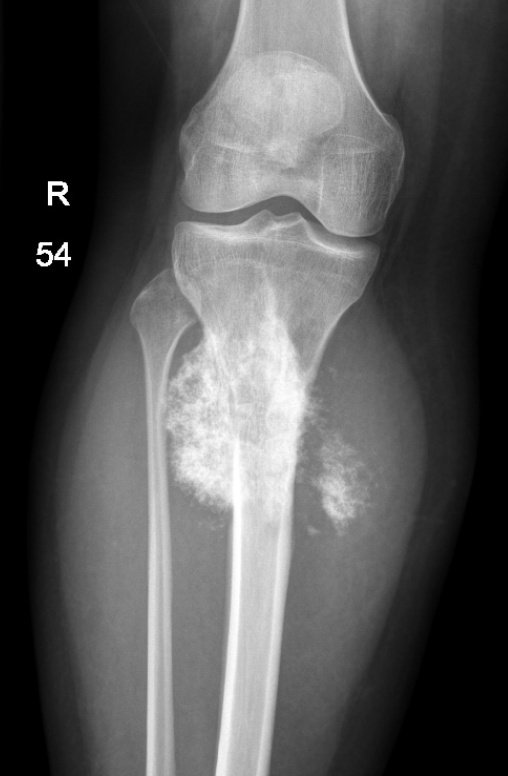
🖼️ Classic Imaging Signs
- Plain X-ray: “Sunburst appearance” 🌞 = spiculated periosteal bone growth.
- Codman’s Triangle: periosteal elevation due to aggressive tumour growth 📐.
- MRI: Defines local extent & soft-tissue invasion (surgical planning).
- CT chest: Essential to look for lung metastases (most common site 🌬️).

🧪 Other Investigations
- Biopsy: Core/open biopsy = gold standard for histological diagnosis.
- Labs: ↑ Alkaline phosphatase & LDH → correlate with tumour burden & prognosis.
- Bone scan: Detects multifocal disease or bone metastases.
💊 Treatment
- Surgery: Mainstay of treatment 🩺✂️
- Limb-salvage surgery now preferred in many cases.
- Amputation still used if tumour encases vital neurovascular structures.
- Chemotherapy: 💉
- Given pre-operatively (neoadjuvant) to shrink tumour.
- Post-operatively (adjuvant) to eliminate micrometastases.
- Common agents: Methotrexate, Doxorubicin, Cisplatin, Ifosfamide (MAP regimen).
- Radiotherapy: ❌ Not effective (radio-resistant).
📈 Prognosis
- With modern therapy: 5-year survival for localised disease ≈ 60–70% 🌟.
- Poorer outcomes in:
- Axial tumours (pelvis/spine/skull).
- Metastatic disease at diagnosis (esp. lungs) 🌬️.
- Poor histological response to neoadjuvant chemo.
🧑🏫 Exam Tip
Remember the triad for imaging OSCEs: Sunburst pattern 🌞, Codman’s triangle 📐, and metaphyseal location near growth plates. Always link osteosarcoma to adolescents with bone pain + swelling and highlight that radiotherapy is not used 🚫.
📚 References
- Oxford Handbook of Oncology
- Campbell’s Operative Orthopaedics
Cases — Osteogenic Sarcoma (Osteosarcoma)
- Case 1 — Adolescent with knee pain 🦴: A 15-year-old boy presents with progressive pain and swelling around his left knee, worse at night and not relieved by rest. Exam: firm, tender mass around distal femur. X-ray: mixed lytic–sclerotic lesion with periosteal elevation (“sunburst” pattern, Codman’s triangle). Diagnosis: osteosarcoma of distal femur. Managed with neoadjuvant chemotherapy followed by limb-salvage surgery.
- Case 2 — Pathological fracture ⚡: A 17-year-old girl presents after a minor fall causing a mid-femoral fracture. History: 3 months of dull bone pain. X-ray: destructive metaphyseal lesion with cortical breach. Biopsy: malignant osteoid production. Diagnosis: osteosarcoma presenting with pathological fracture. Managed with chemo and surgical resection; orthopaedic oncology team involved.
- Case 3 — Metastatic disease 🌬️: A 14-year-old boy with known osteosarcoma of the proximal tibia (diagnosed 6 months ago) presents with cough and breathlessness. CT chest: multiple cannonball pulmonary metastases. Diagnosis: osteosarcoma with lung metastases. Managed with systemic chemotherapy, resection of primary tumour, and palliative resection of lung mets if feasible.
Teaching Point 🩺: Osteosarcoma is the most common primary malignant bone tumour in adolescents, usually affecting metaphyses of long bones (distal femur, proximal tibia, proximal humerus). Key features: progressive bone pain, swelling, pathological fractures. X-ray: sunburst periosteal reaction, Codman’s triangle. Metastasis: commonly to lungs. Management: multi-agent chemotherapy + surgical resection (limb-salvage or amputation).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
