| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Juvenile Idiopathic Arthritis (Stills Disease)
Related Subjects: | Monoarticular Arthritis | Polyarticular Arthritis | Seronegative Spondyloarthropathies | Ankylosing Spondylitis | Enteropathic Spondyloarthritis | Reactive Arthritis | Psoriatic Arthritis
🧒 Juvenile Idiopathic Arthritis (JIA) is the most common chronic rheumatic disease of childhood. Aspirin should be avoided in children <12 due to the risk of Reye’s syndrome ⚠️. Tumour necrosis factor (TNF) 🧬 is a key pro-inflammatory cytokine in JIA pathogenesis.
📖 About
- Accounts for ~10% of all chronic arthritis in children.
- Onset usually <16 years (often <5 years).
- Systemic form may mimic infection or malignancy.
- Adult-onset Still’s disease is the adult equivalent, but rare.
🧬 Aetiology
- Equal male:female in systemic type; other subtypes more female.
- Genetic predisposition – HLA associations.
- Environmental triggers (infections, stress, trauma) may unmask disease.
- Pathogenesis: imbalance of Th1 (IFN-γ) and Th17 (IL-17) cells + dysregulated innate immunity (IL-1, IL-6, TNF-α).
🔑 Definitions
- Oligoarthritis: ≤4 joints in first 6 months.
- Polyarthritis: ≥5 joints in first 6 months.
- Systemic JIA (sJIA): Autoinflammatory form with fever + rash + organ involvement.
🌈 Subtypes
- Oligoarthritis – 50–60%.
- RF+ polyarthritis – 11–28% (resembles adult RA).
- RF– polyarthritis – 2–7%.
- Systemic JIA: 🩸 High spiking fevers, salmon-pink rash, lymphadenopathy, hepatosplenomegaly, serositis.
- Psoriatic arthritis 🎨.
- Enthesitis-related arthritis 🦶 – HLA-B27 associated.
- Undifferentiated arthritis.
🤒 Classic Clinical Features (Systemic JIA)
- Daily high fevers (>39°C), often evening spikes 🌡️.
- Transient pink/salmon maculopapular rash 🌸.
- Arthralgia/arthritis (sometimes late feature).
- Other: lymphadenopathy, hepatosplenomegaly, myocarditis, pericarditis, pleurisy, dry eyes (uveitis risk).
- ~50% risk of chronic destructive arthritis long-term 🦴.
🔎 Investigations
- Bloods: ↑ ESR, ↑ CRP, ↑ ferritin 📈 (esp. systemic JIA).
- FBC: Anaemia of chronic disease, ↑ neutrophils, ↑ platelets.
- Autoantibodies usually negative (ANA, RF, HLA-B27). ⚠️ High RF or ANA positivity may point to alternative diagnoses.
- Imaging: – X-rays may be normal early. – 🖥️ Ultrasound: synovial thickening, effusion, tenosynovitis. – MRI: 🥇 gold standard – detects bone marrow oedema and erosions.
🩺 Differentials
- Oligoarthritis mimics: Reactive arthritis, toxic synovitis, septic arthritis, osteomyelitis, haemophilia, sickle cell, trauma/NAT, tumours.
- Polyarthritis mimics: SLE, MCTD, rheumatic fever, IBD-related arthritis, sarcoid, CRMO.
- Systemic mimics: Infections (mycoplasma, EBV, endocarditis), Kawasaki disease, PFAPA, malignancy (ALL, lymphoma), autoinflammatory syndromes.
⚠️ Complications
- Growth disturbance & leg-length discrepancy.
- Joint contractures & disability.
- Macrophage activation syndrome (MAS) – life-threatening cytokine storm 🛑.
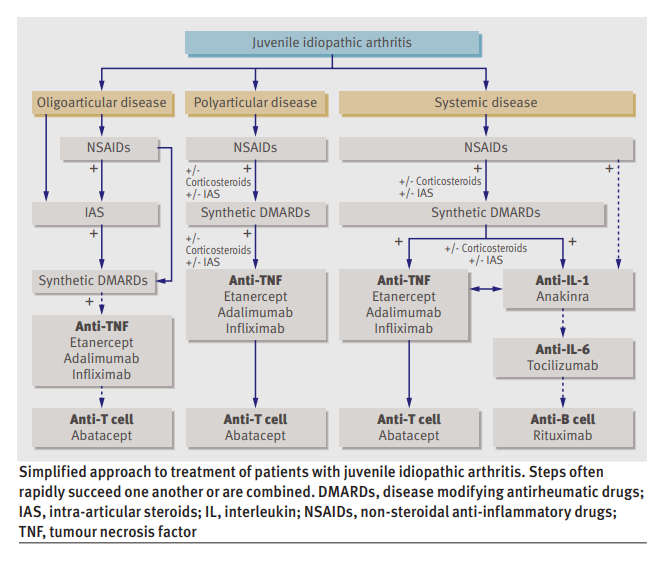
💊 Management
- All suspected JIA → urgent referral to paediatric rheumatology 👩⚕️.
- NSAIDs for pain & stiffness (avoid aspirin in <12).
- Steroids (systemic or intra-articular) for acute flares or organ involvement.
- Methotrexate – cornerstone steroid-sparing agent.
- Biologics: Anti-TNF (etanercept, adalimumab), IL-1 (anakinra), IL-6 (tocilizumab) for refractory cases 🧬.
- Vaccination: Avoid live vaccines if immunosuppressed. Annual flu 💉 recommended.
- Monitor growth, eye health (uveitis risk), and bone health (steroids + inactivity risk).
📚 References
Case – Systemic Juvenile Idiopathic Arthritis (Still’s disease)
A 9-year-old presents with 2 weeks of daily quotidian fevers peaking late afternoon, an evanescent salmon-pink rash appearing with fever, migratory arthralgia now localising to both knees, and sore throat; exam shows hepatosplenomegaly and mild lymphadenopathy. Labs: markedly ↑CRP/ESR, neutrophilia, anaemia, thrombocytosis, and very high ferritin (low glycosylated fraction if tested); cultures negative; CXR normal. After excluding infection and malignancy, diagnose systemic JIA; screen vigilantly for macrophage activation syndrome (MAS) (cytopenias, rising ferritin with falling ESR, ↑ALT, ↑triglycerides). Management: start systemic glucocorticoids for control and escalate early to targeted therapy—IL-1 blockade (anakinra) or IL-6 blockade (tocilizumab)—with physiotherapy and bone/gastroprotection; involve paediatric rheumatology and monitor joints, growth, LFTs, and MAS red flags.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Disease
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
