| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
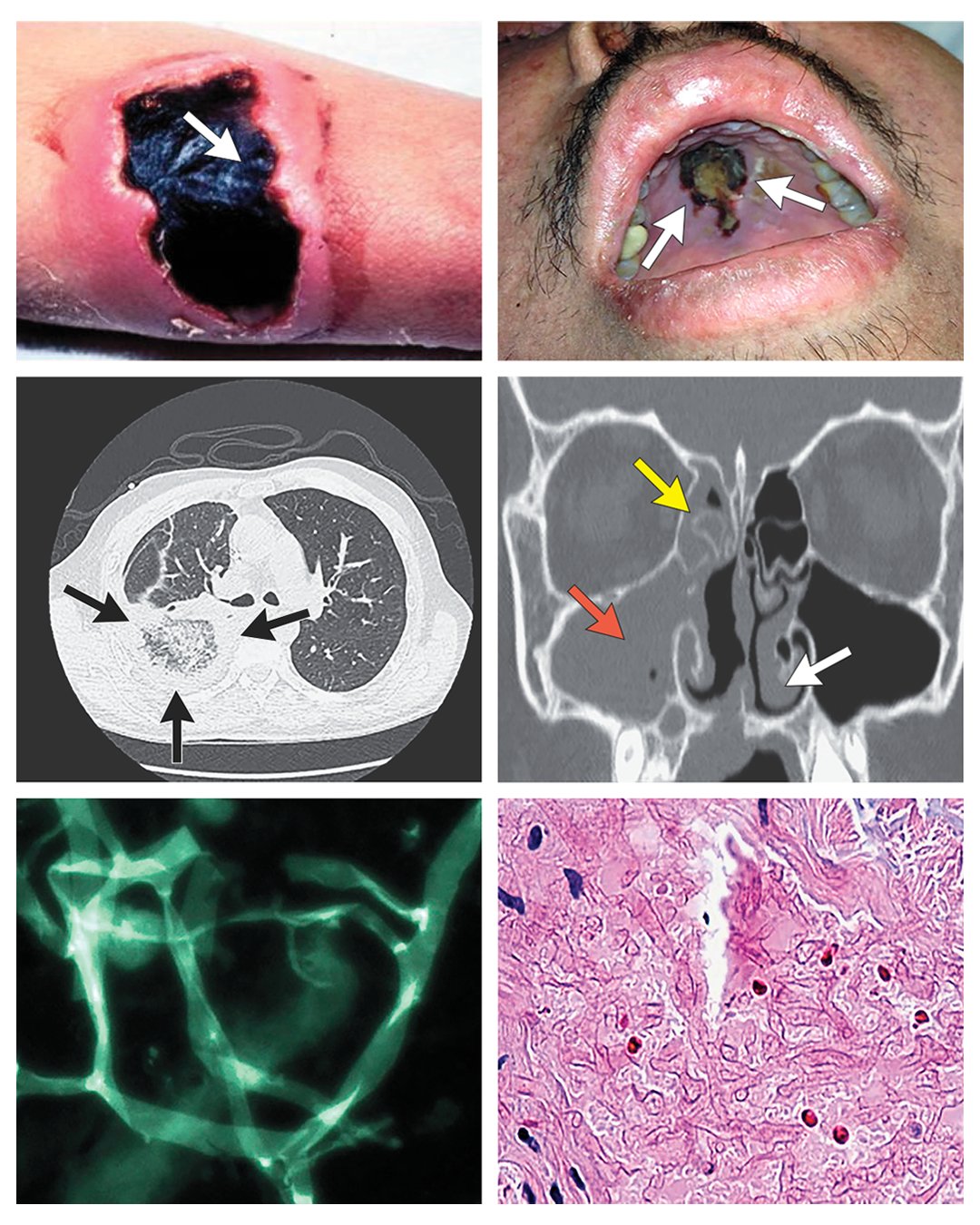
Rhino-Orbital-Cerebral Mucormycosis
⚠️ Mucormycosis (“Black Fungus”) is an aggressive, invasive fungal infection with high mortality (50–80%). Cases surged post-COVID, especially in diabetic patients treated with corticosteroids. It is a medical emergency requiring rapid recognition and multidisciplinary care.
🦠 About
- Opportunistic infection caused by fungi of the order Mucorales, thriving in immunocompromised states (notably diabetes and DKA).
- Mortality remains high unless both antifungal therapy and surgical debridement are initiated promptly.
- Nicknamed the “Black Fungus” due to necrotic tissue caused by angioinvasion and thrombosis.
📚 Aetiology
- Mucorales invade blood vessels → thrombosis → infarction → necrosis.
- Most infections start via inhalation of spores in the paranasal sinuses or lungs.
- Rhizopus species produce ketone reductase, allowing survival in acidic, glucose-rich environments (classic in DKA).
- Iron overload and Desferrioxamine therapy increase susceptibility (fungi exploit the iron shuttle effect).
🔬 Common Organisms
- Genera most often isolated:
- Rhizopus spp.
- Mucor spp.
- Rhizomucor spp.
- Myocladus spp.
⚡ Risk Factors
- Uncontrolled diabetes ± DKA (most common risk worldwide).
- Post-COVID recovery with high-dose steroids or immune suppression.
- Haematological malignancies, chemotherapy, malnutrition.
- Solid organ transplant, AIDS, severe burns.
- Iron overload or desferrioxamine therapy.

🩺 Clinical Presentation
- Rhino-Orbital-Cerebral: Sinus pain, headache, black necrotic eschar on palate/turbinates, orbital swelling, proptosis, cranial nerve palsies. Can extend to brain causing seizures or hemiplegia.
- Pulmonary: Fever, cough, pleuritic pain, haemoptysis, cavitary necrotic lesions on CT. Often mistaken for TB/aspergillosis.
- Cutaneous: Necrotic ulcers after trauma or burns, progressing rapidly to black gangrenous lesions.
- Disseminated: Spread from lungs/sinuses → brain, spleen, liver. Very poor prognosis.
🧪 Investigations
- Bloods: FBC, glucose, ABG (check for metabolic acidosis in DKA).
- Histopathology: Broad, non-septate hyphae with right-angle branching invading tissue/vessels.
- Culture: Confirms diagnosis but hazardous – requires specialist lab.
- Imaging:
- CT/MRI sinuses/orbit/brain: Evaluate spread in rhino-orbital disease.
- HRCT chest: Cavitation, consolidation, halo or reverse-halo signs.
💊 Management
- Immediate combined approach: Antifungals + urgent surgical debridement + reversal of risk factors (e.g. optimise diabetes, reduce steroids).
- Antifungal therapy:
- Liposomal Amphotericin B (preferred, high dose).
- Posaconazole or Isavuconazole for step-down/maintenance.
- Surgery: Aggressive debridement of necrotic tissue is often life-saving.
- Supportive care: Glycaemic control, fluids, and electrolyte balance.
- Note: Mucormycosis is not contagious.
⚠️ Poor Prognostic Factors
- Delayed diagnosis (>5 days from symptom onset).
- Antifungal therapy without surgical debridement.
- Intracranial extension (meningitis, hemiplegia).
- Persistent DKA or severe immunosuppression.
📖 References
- Rhino-Orbital-Cerebral Mucormycosis – EyeWiki
- Rodriguez MM et al. Clinical Microbiology Reviews, 2020.
- NICE COVID-19 Rapid Guideline: Fungal Infections (2021).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
