| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Anaromy and Physiology of the Brain
Related Subjects: | |Anaromy and Physiology of the Brain
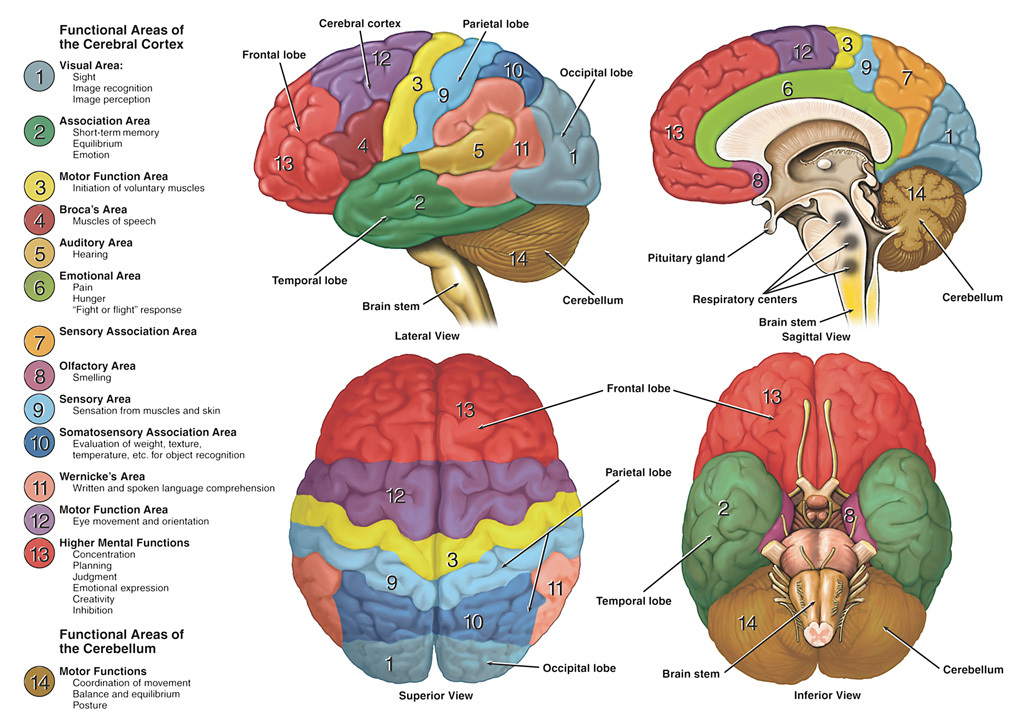
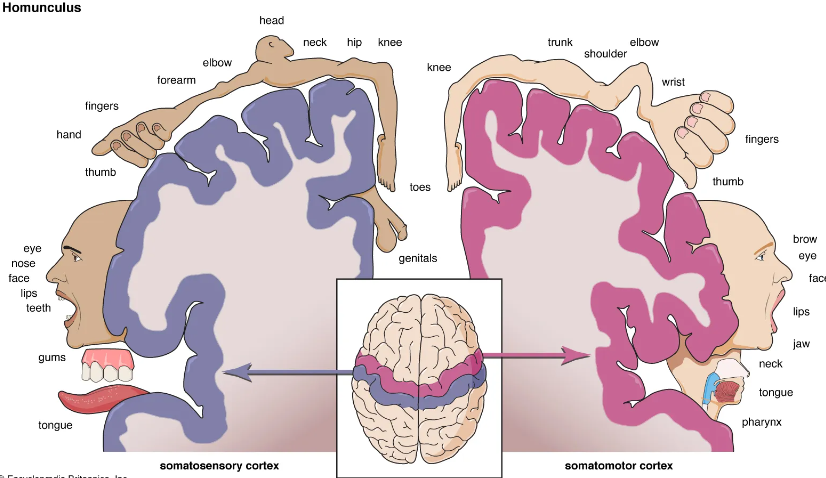
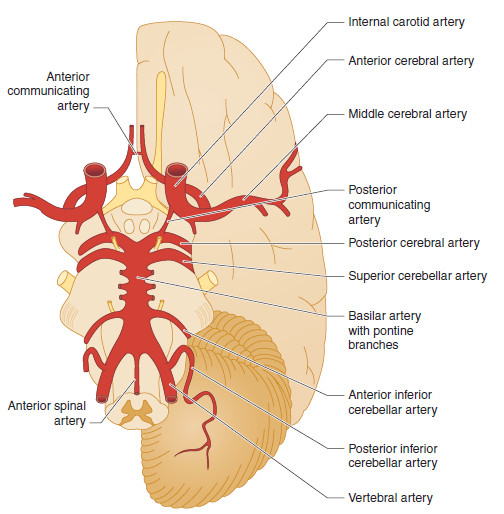
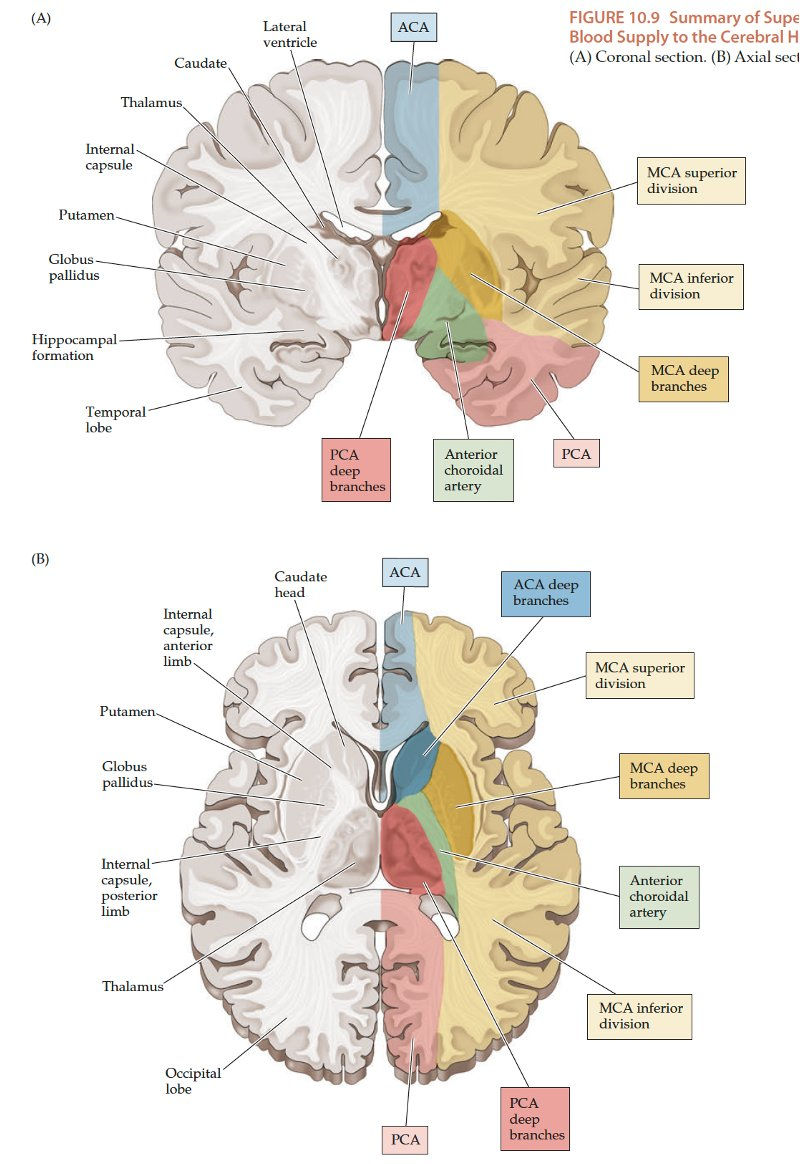
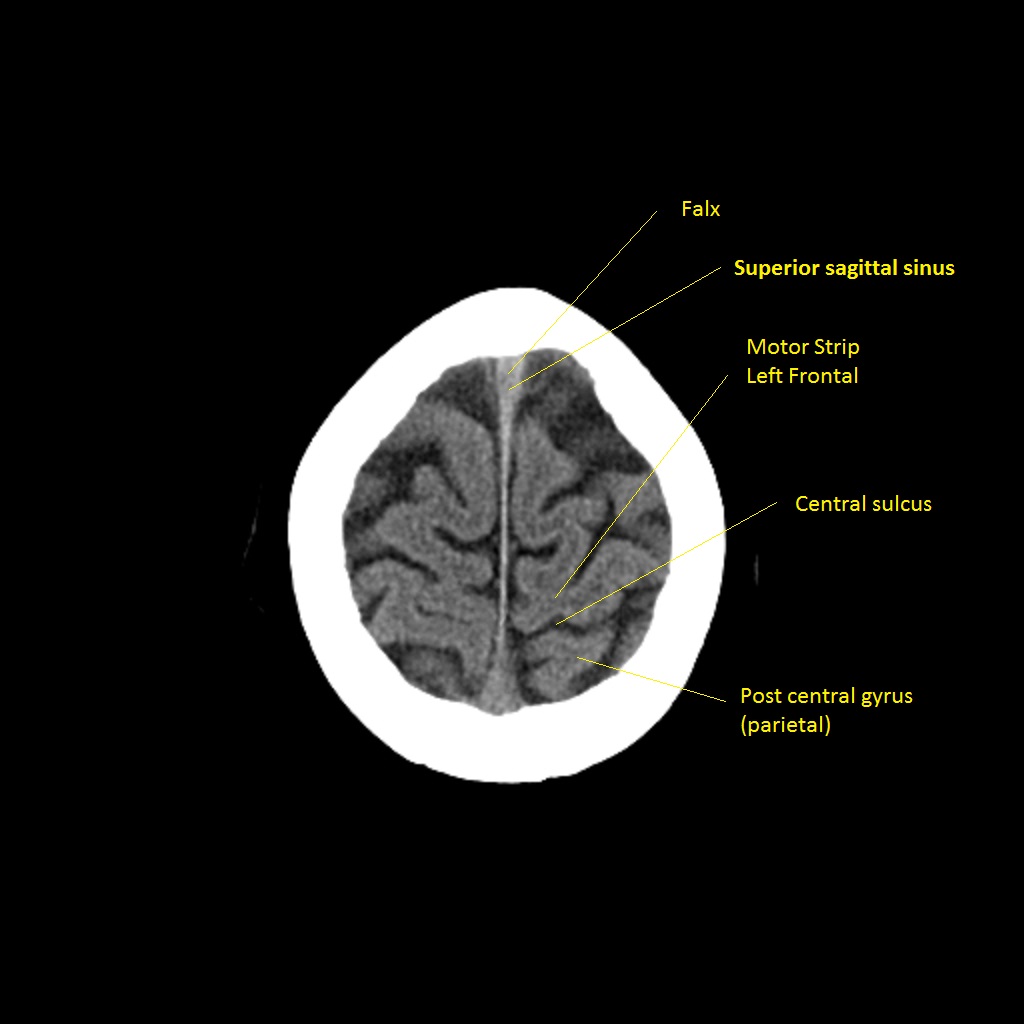
Understanding arterial territories helps you predict the clinical pattern from the scan, and vice versa. The cortex is organised somatotopically (homunculus), and different vascular territories supply different functional regions – so patterns of weakness, language disturbance and visual loss all “map” back to this arterial anatomy.
Global View: Brain Surface & Functional Areas
Circle of Willis
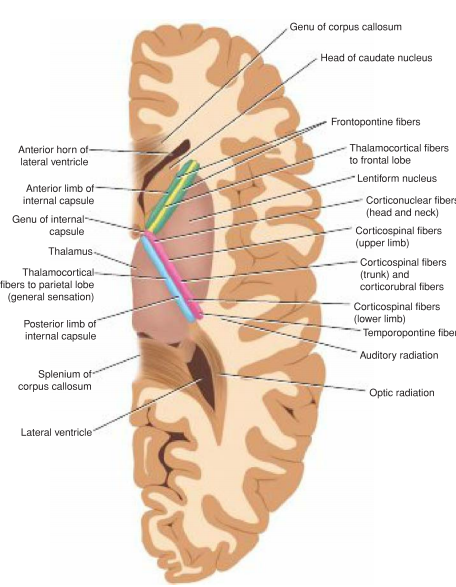
Internal Capsule
The lateral brain surface shows the motor and sensory cortices arranged from face (laterally) to leg (medially). Frontal lobe lesions typically affect motor control, behaviour, planning and speech output (dominant hemisphere). Parietal lesions cause sensory disturbance and visuospatial neglect (usually non-dominant). Temporal lobe lesions affect language comprehension (dominant), memory and visual recognition.
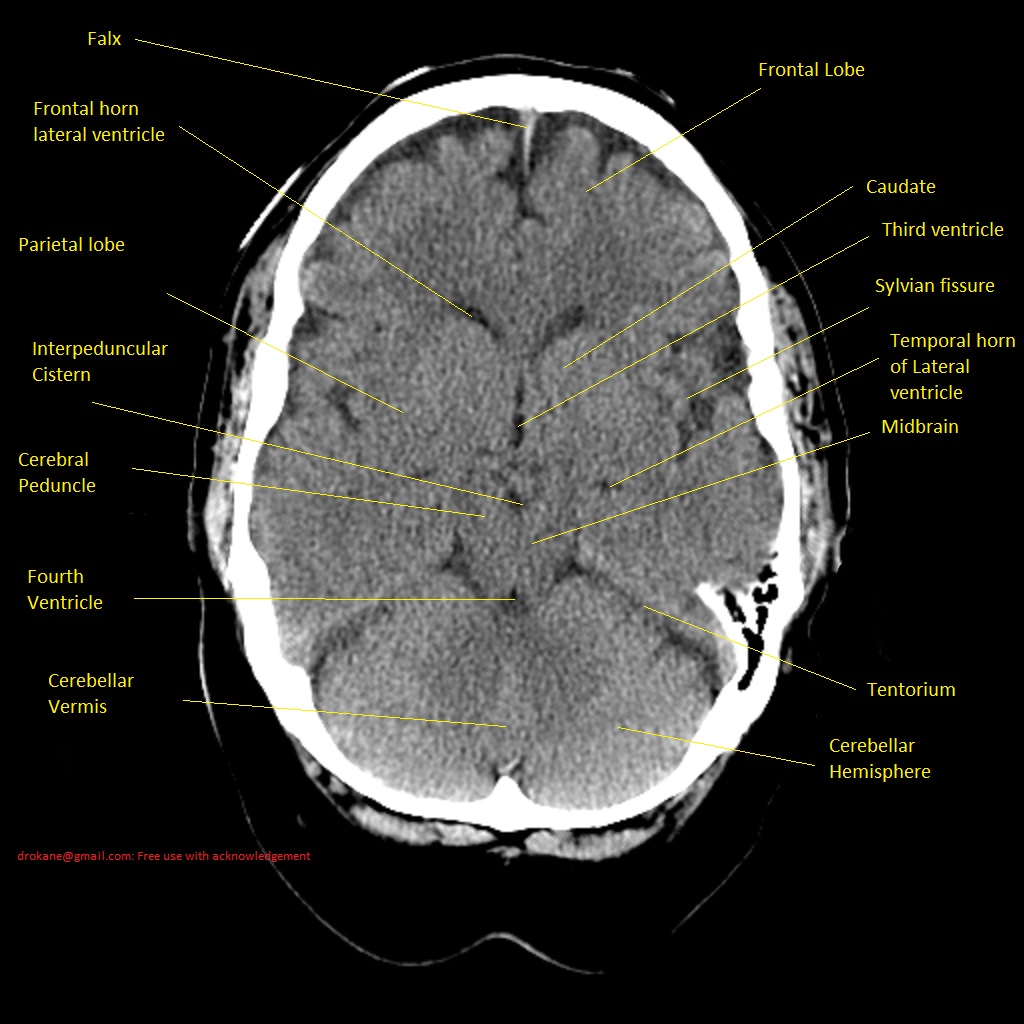
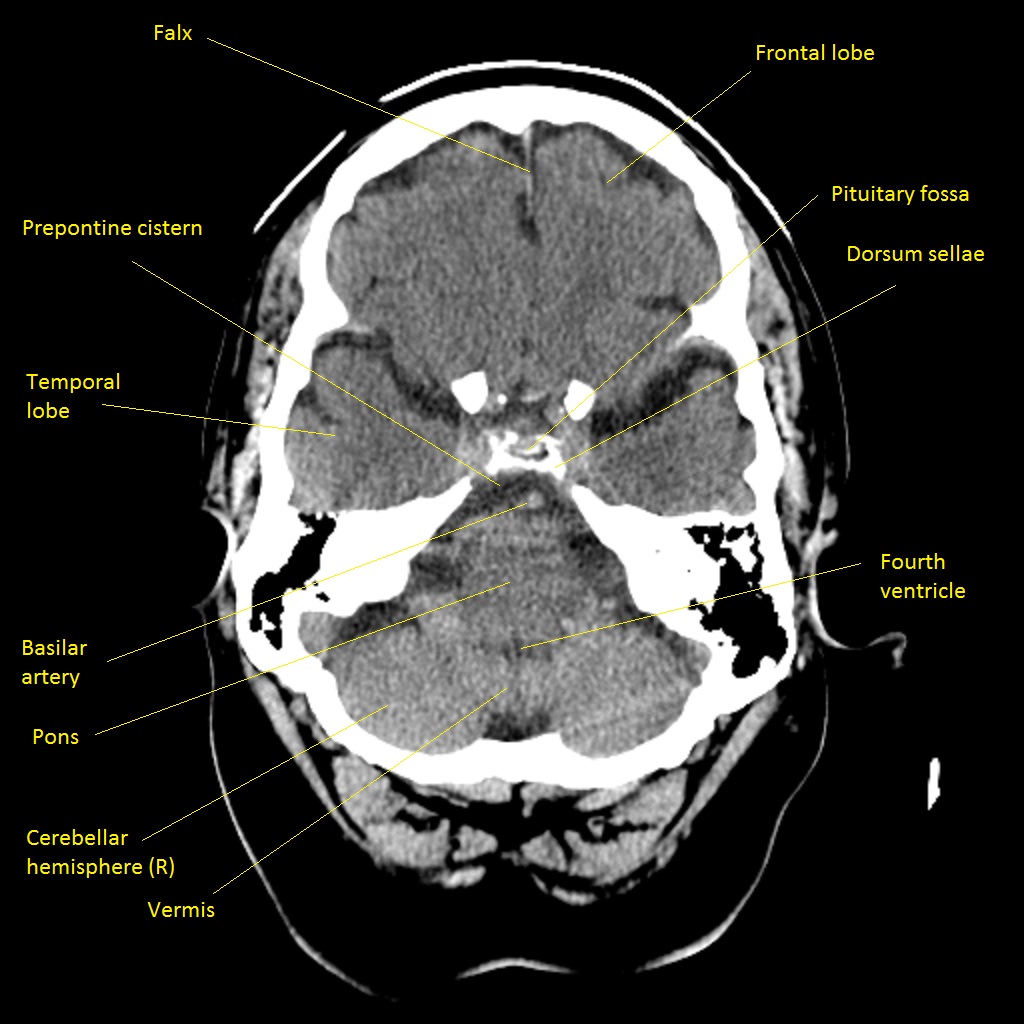
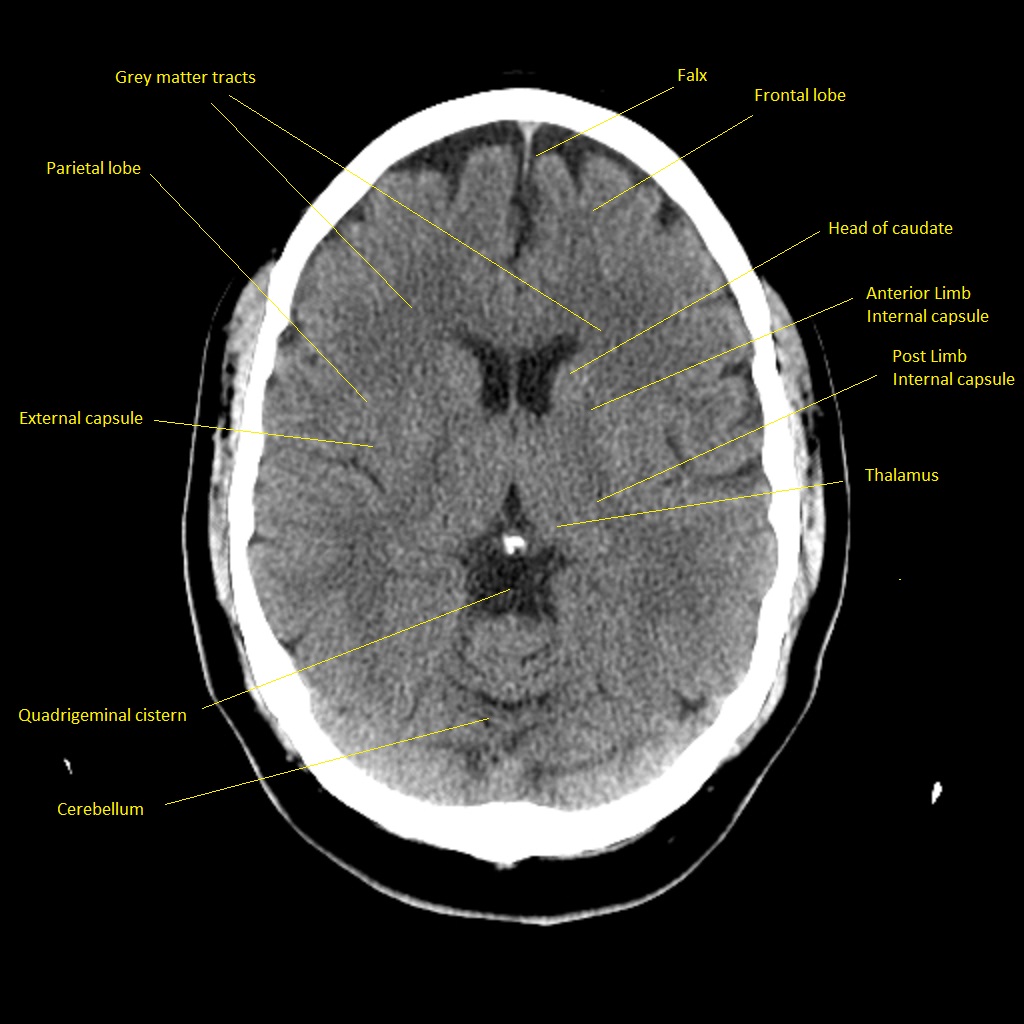
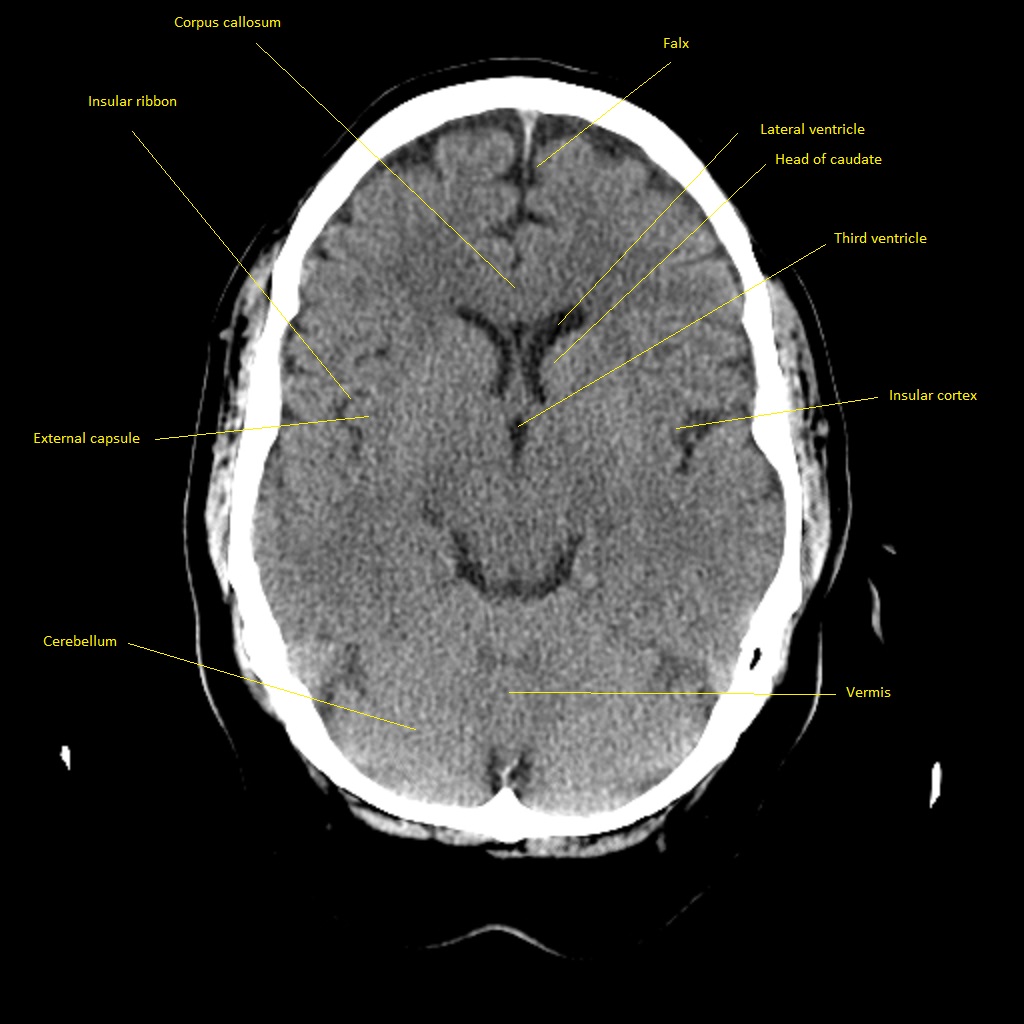
CT scan





Anterior Cerebral Artery (ACA) Territory

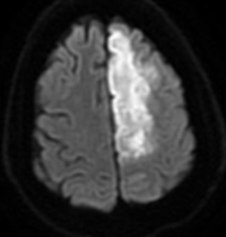
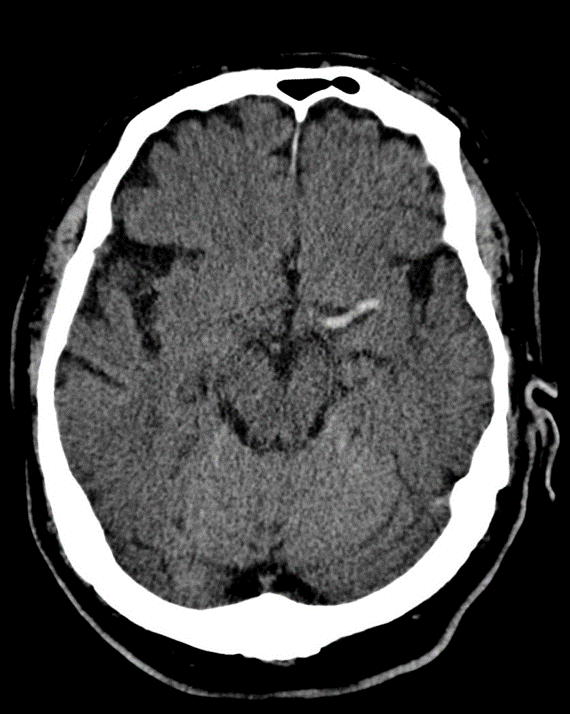
Dense MCA
The ACA supplies the medial frontal and parietal lobes, including the leg area of the primary motor and sensory cortex, supplementary motor area and parts of the cingulate gyrus. Clinically this gives leg ≫ arm weakness and sensory loss, often with abulia, impaired initiation and sometimes urinary incontinence. Because the face and arm are largely MCA territory, they may be relatively spared, which is a useful bedside clue. Bilateral ACA infarcts (e.g. in ACom pathology) can cause profound akinetic mutism and behavioural change.
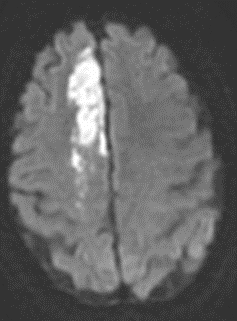
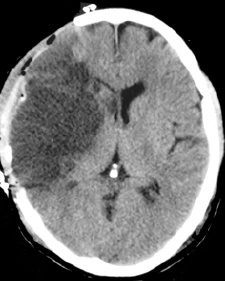
High Middle Cerebral Artery (MCA) Territory



The superior division of the MCA supplies lateral frontal cortex (including face/arm motor areas and Broca’s area in the dominant hemisphere). A “high MCA” cortical stroke typically causes contralateral face and arm weakness ≫ leg, with dysphasia if the dominant hemisphere is involved, or neglect and inattention if the non-dominant hemisphere is affected. Visual field defects (inferior quadrantanopia or homonymous hemianopia) reflect involvement of optic radiations in the temporal and parietal lobes.
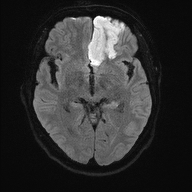
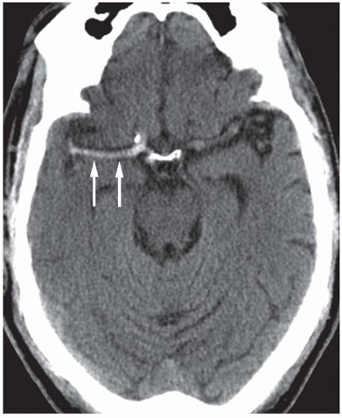
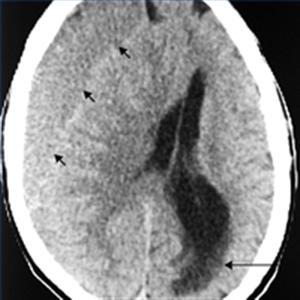
Striatocapsular - reperfused MCA preserses cortex
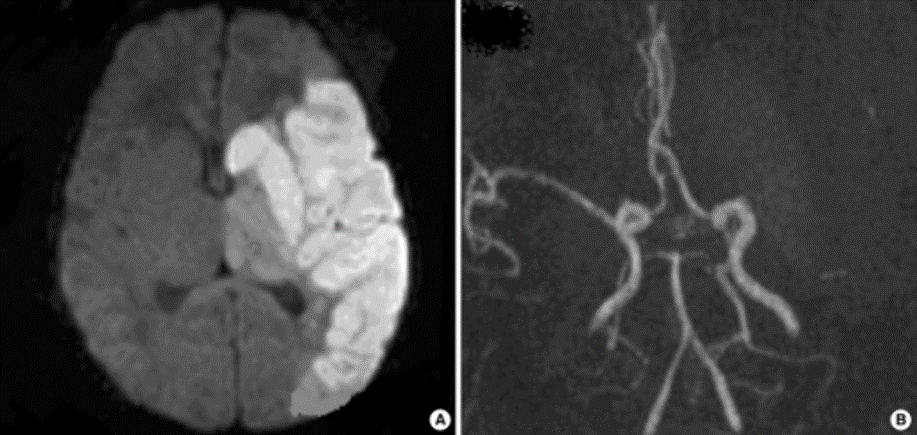
MCA and ACA infarction likely due to carotid occlusion

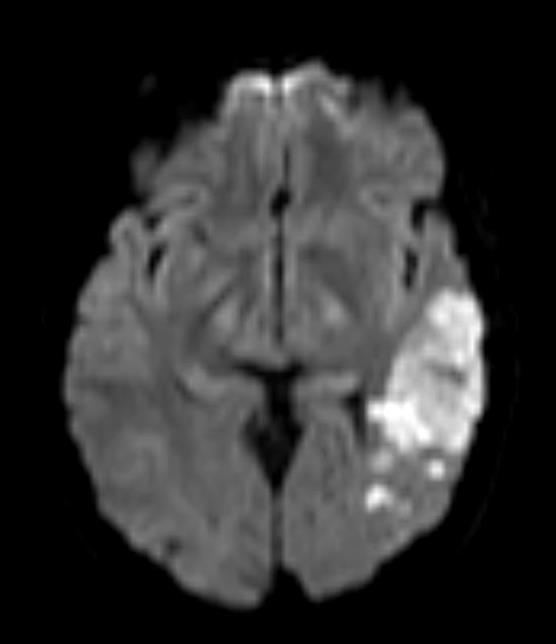
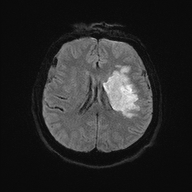
Posterior Cerebral Artery (PCA) Territory


The PCA supplies the occipital lobes, inferior temporal lobes and parts of the thalamus and midbrain. Classically, PCA stroke causes a contralateral homonymous hemianopia often with macular (foveal) sparing due to dual supply from MCA. Dominant PCA strokes can produce alexia without agraphia, visual agnosia and memory disturbance. Bilateral PCA infarction can lead to cortical blindness and Anton’s syndrome (denial of blindness).
Fetal PCA Infraction
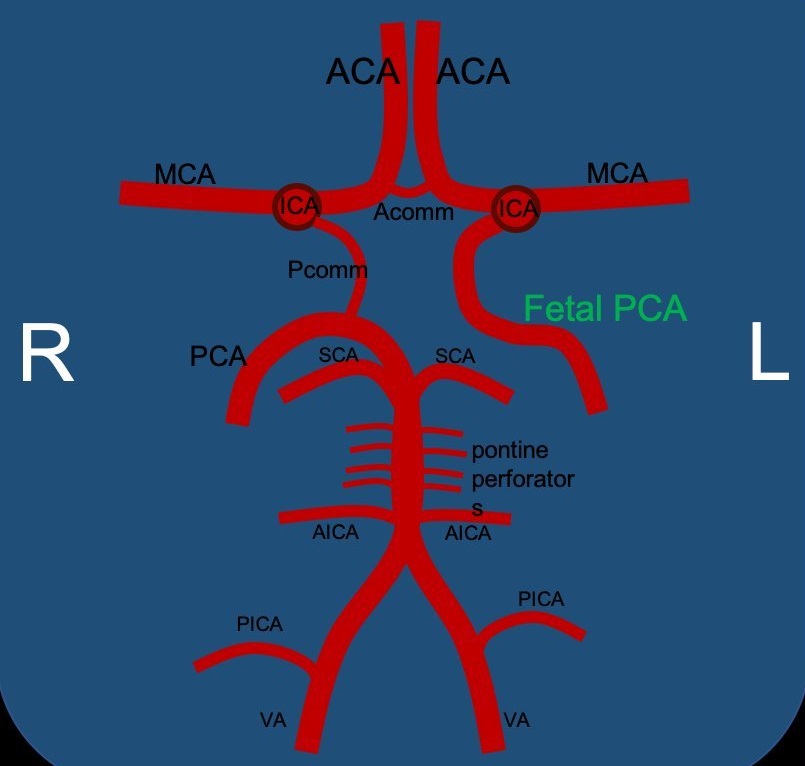
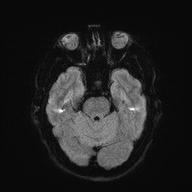
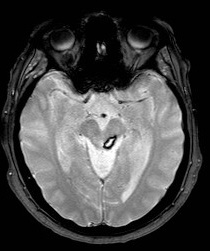
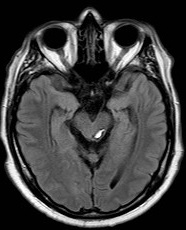
Artery of Percheron (AOP)
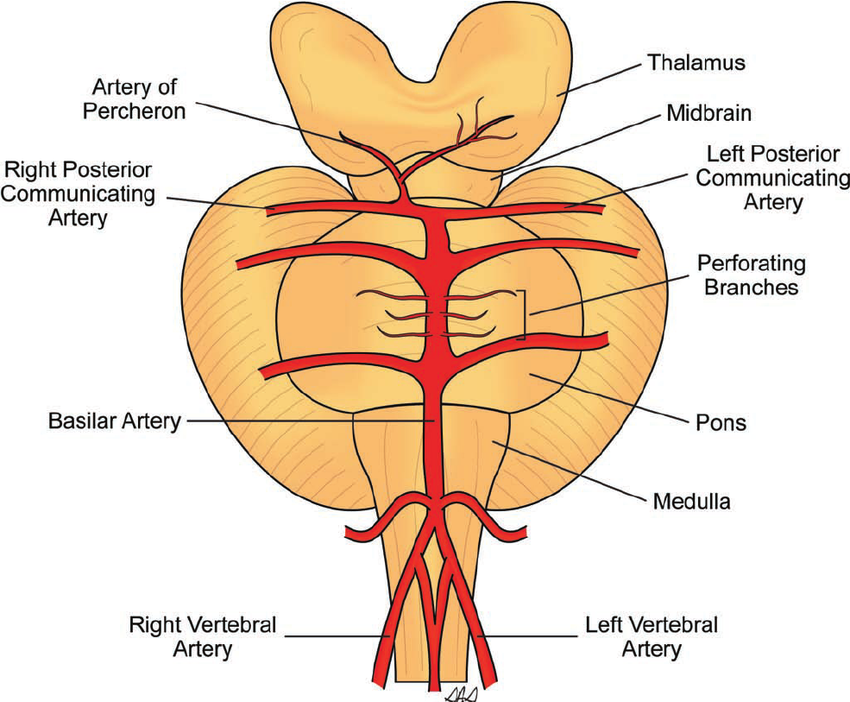
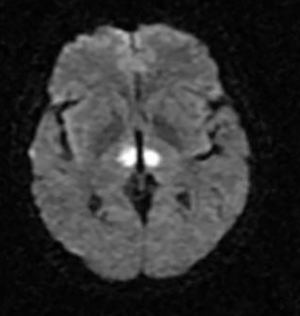

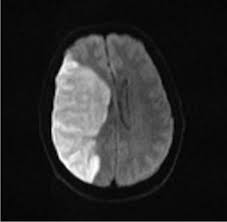
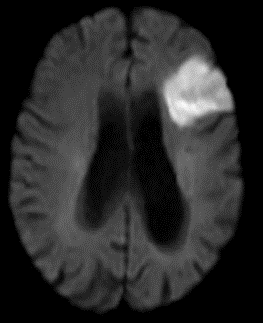
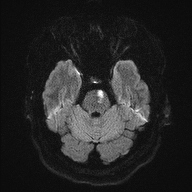
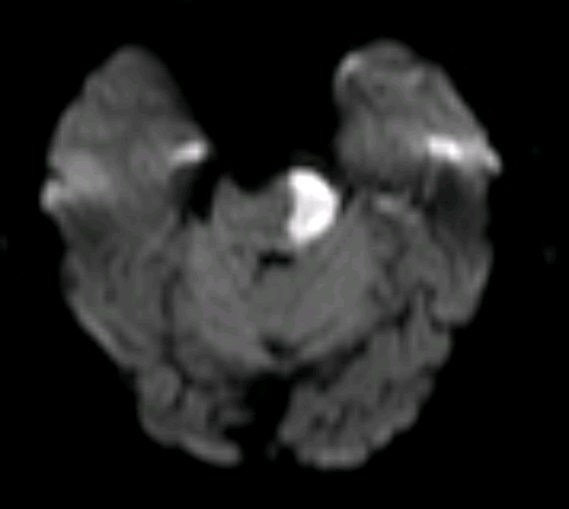
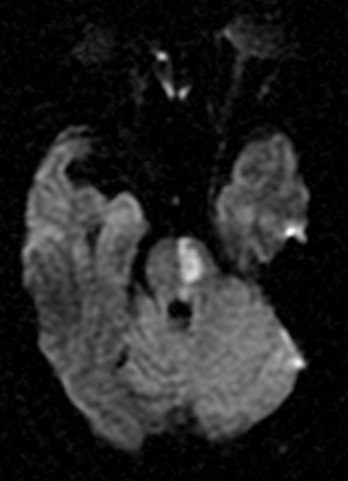
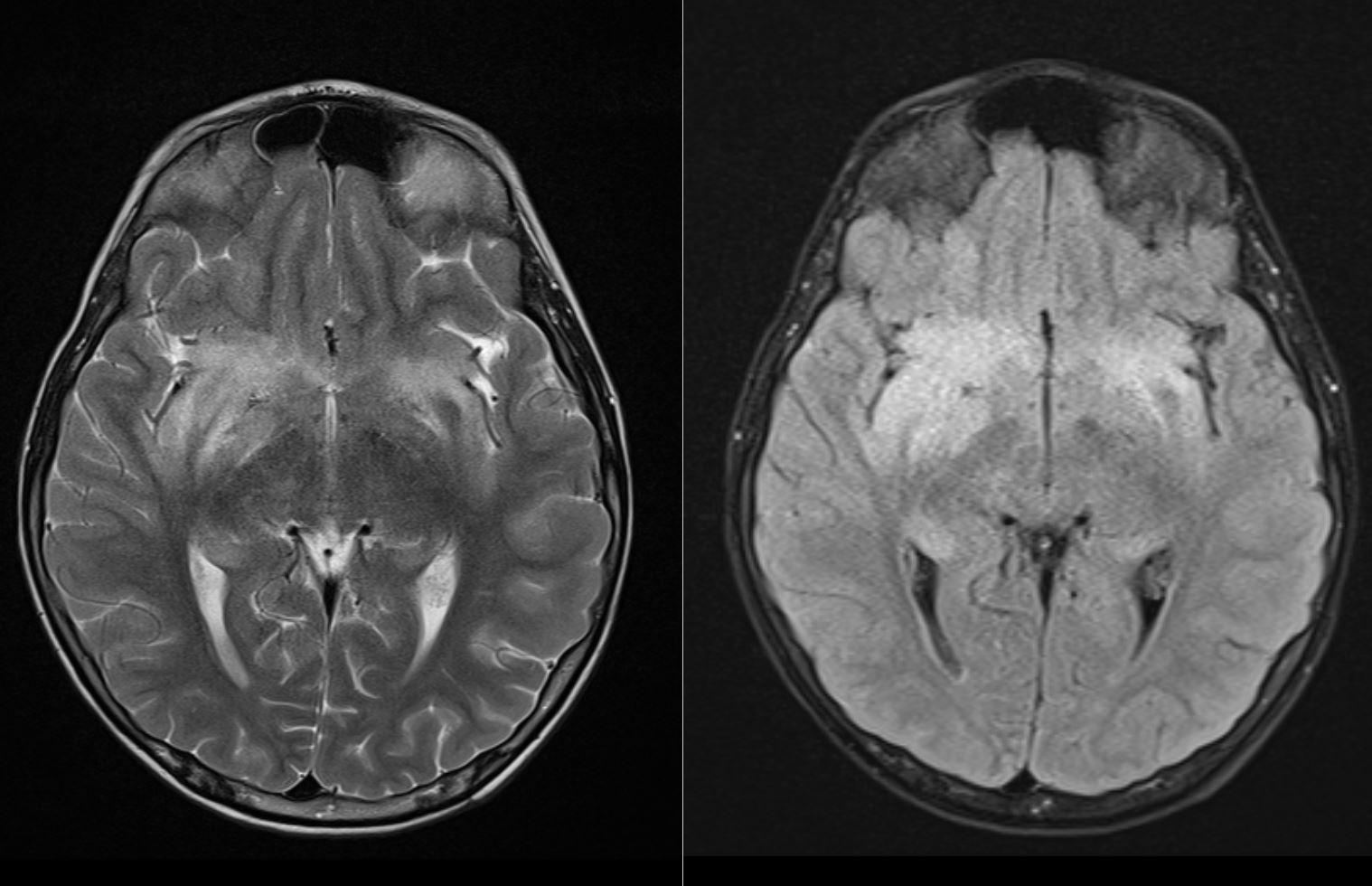
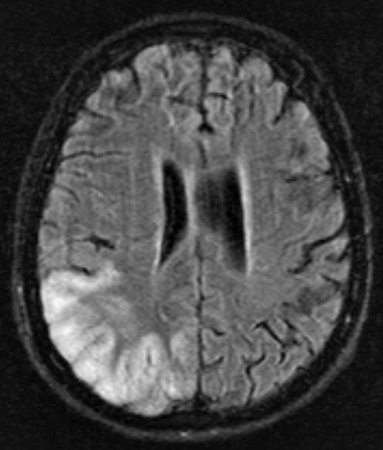
The Artery of Percheron is a single arterial trunk arising from one PCA, supplying both paramedian thalami ± the rostral midbrain. Occlusion gives a striking pattern of bilateral paramedian thalamic infarction, with sudden reduced consciousness, vertical gaze palsy, memory impairment and fluctuating confusion. Because the variant is anatomical rather than atherosclerotic, patients are often younger and standard CT head can initially be subtle. MRI DWI is particularly helpful in confirming the diagnosis.
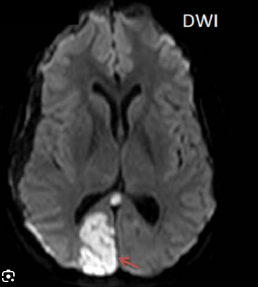
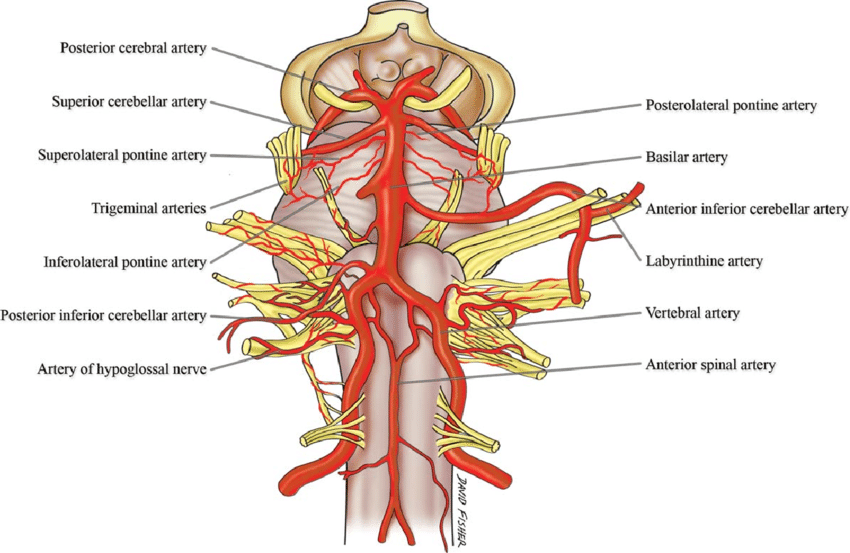
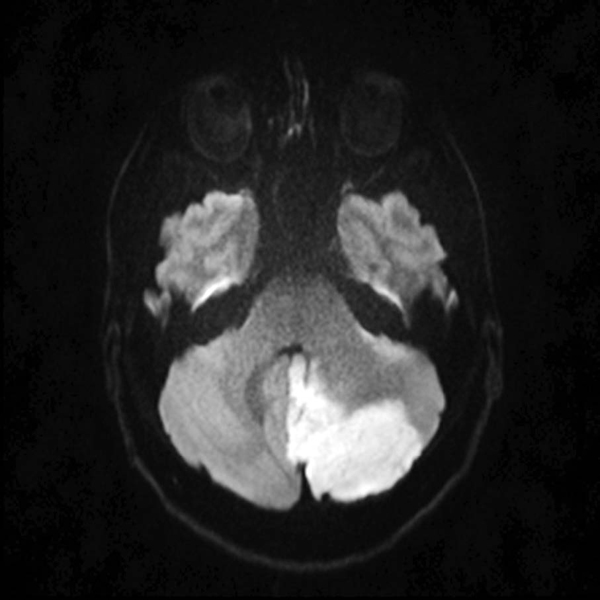
Posterior Inferior Cerebellar Artery (PICA)
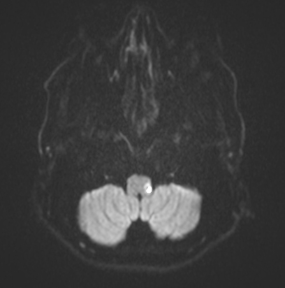

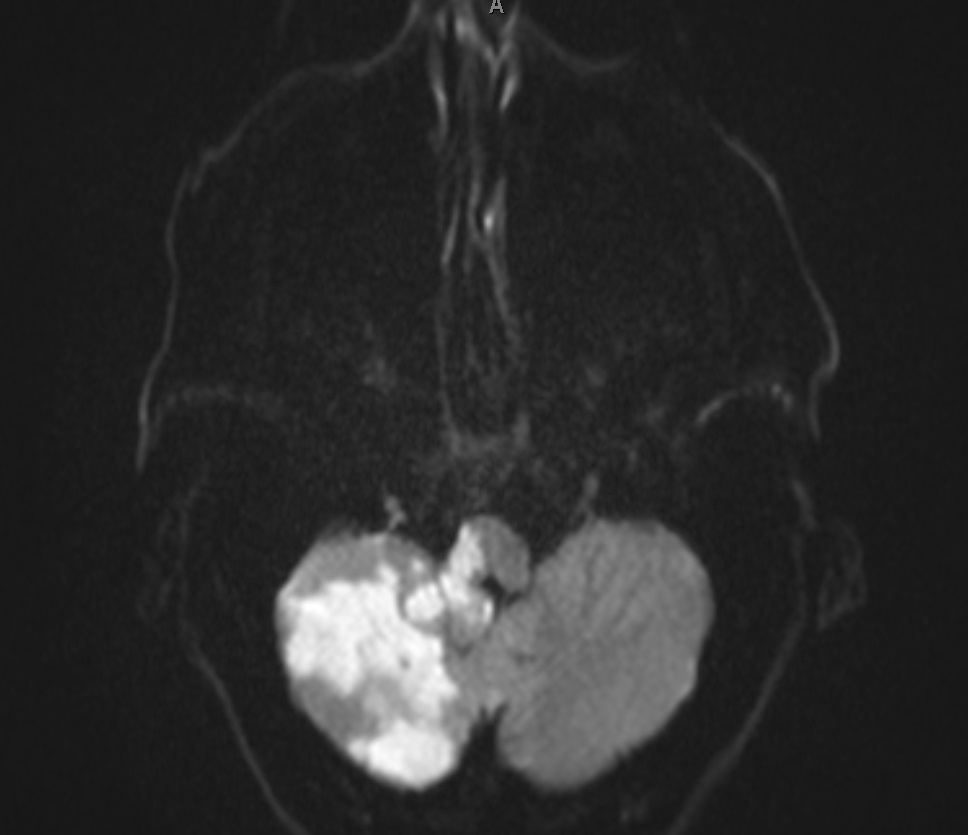
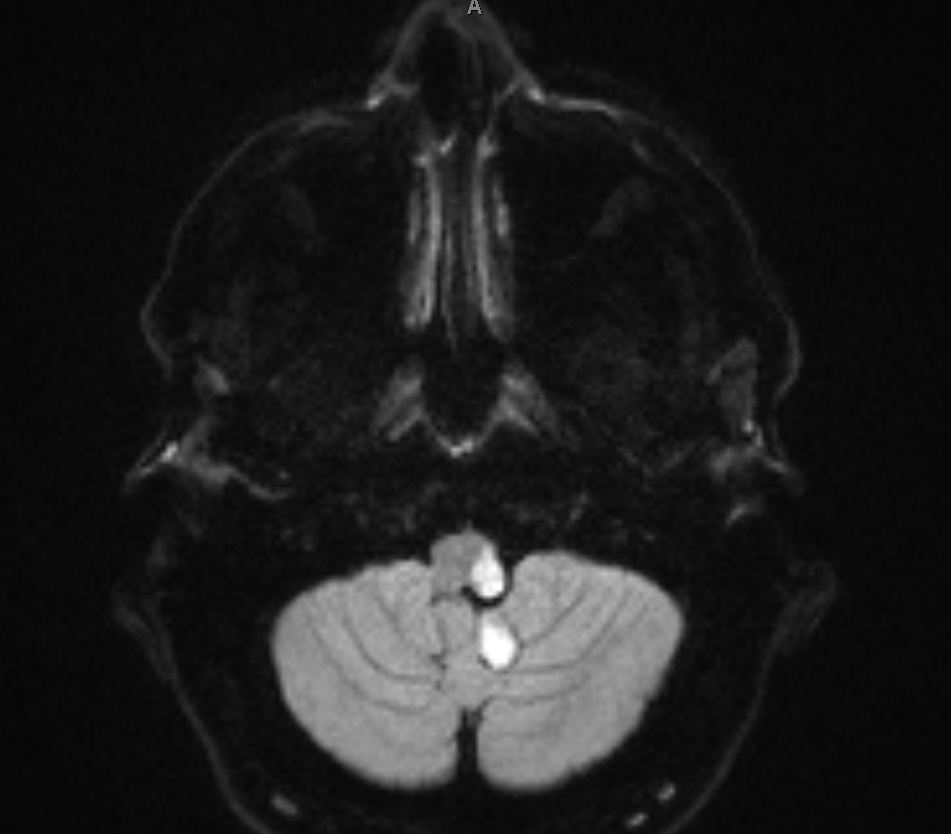
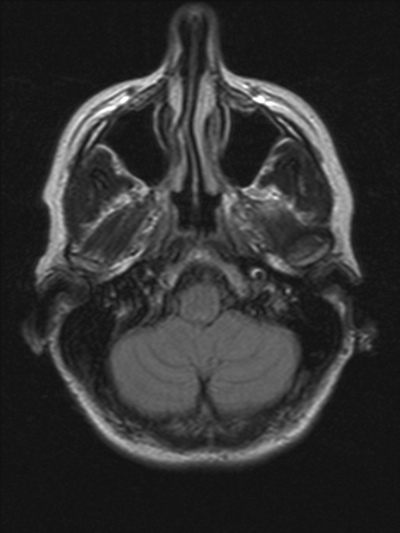
PICA supplies the inferior cerebellar hemisphere and the lateral medulla – giving the classic lateral medullary (Wallenberg) syndrome. Clinical features include ipsilateral ataxia, vertigo, nystagmus, ipsilateral facial loss of pain/temperature with contralateral body pain/temperature loss, dysphagia and dysarthria, and a tendency to fall towards the lesion side. Horner’s syndrome may be present from disruption of descending sympathetic fibres. Importantly, PICA strokes can be scan negative early on CT, so careful clinical localisation is crucial.
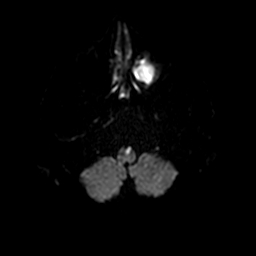
Anterior Inferior Cerebellar Artery (AICA)

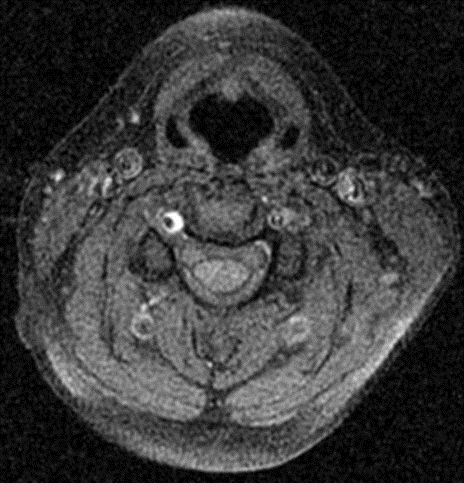
AICA supplies the lateral caudal pons and anterior inferior cerebellum, as well as the internal auditory (labyrinthine) artery in many people. AICA stroke can cause ipsilateral facial weakness (lower motor neuron), loss of facial sensation, gaze palsies and ataxia. Because of labyrinthine involvement, acute unilateral deafness and severe vertigo are important bedside clues favouring AICA over PICA. Differentiating these posterior circulation syndromes matters because the prognosis and risk of haemorrhagic transformation can differ.
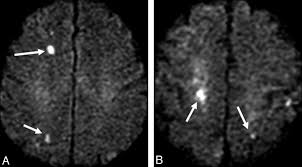
Penetrating Artery Occlusion – Lacunar Stroke

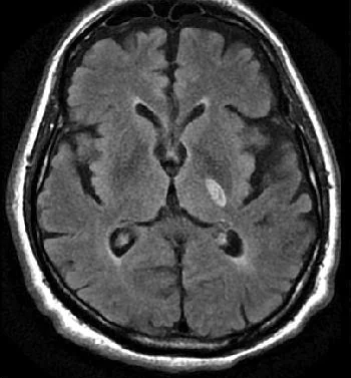
Lacunar strokes are small (<15 mm) infarcts due to occlusion of deep perforating arteries (e.g. lenticulostriate, thalamoperforating branches), typically in the internal capsule, basal ganglia, thalamus or pons. They produce “pure” clinical syndromes such as pure motor hemiparesis, pure sensory stroke, ataxic hemiparesis or dysarthria–clumsy hand syndrome, without cortical signs (no aphasia, neglect or visual field cut). The underlying pathology is lipohyalinosis related to hypertension and diabetes, so secondary prevention focusing on blood pressure and vascular risk factor control is key.
Anterior Medullary (Medial Medullary) Infarct
Medial medullary infarction is less common than lateral medullary stroke, and classically presents with the “Dejerine triad”: contralateral weakness (pyramidal tract), contralateral loss of vibration/proprioception (medial lemniscus) and ipsilateral tongue weakness (hypoglossal nerve) – the tongue deviates towards the lesion. The vascular supply comes from branches of the anterior spinal artery and vertebral artery. Clinically there is often dense hemiparesis but with preserved facial sensation and without the prominent vertigo and sensory dissociation seen in lateral medullary (PICA) syndromes.
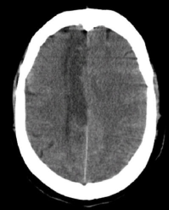
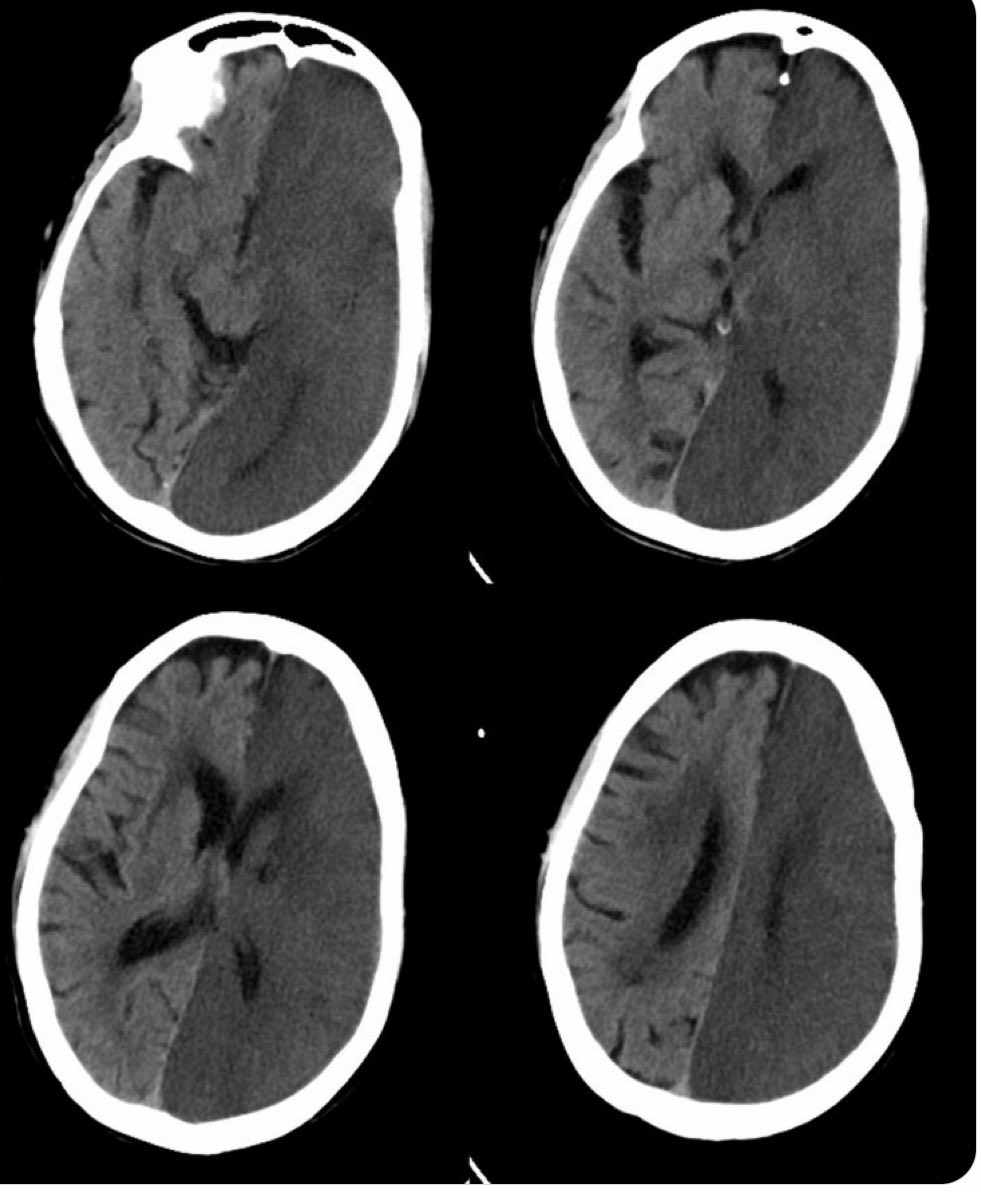
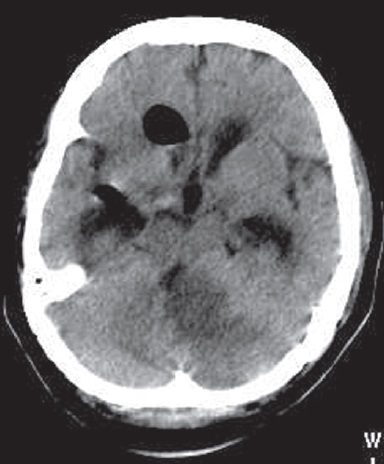
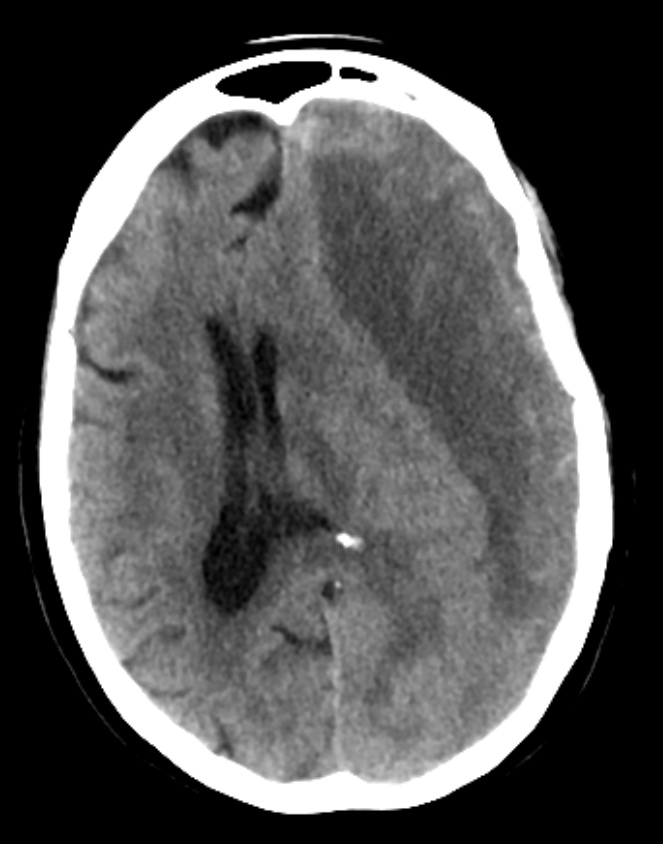
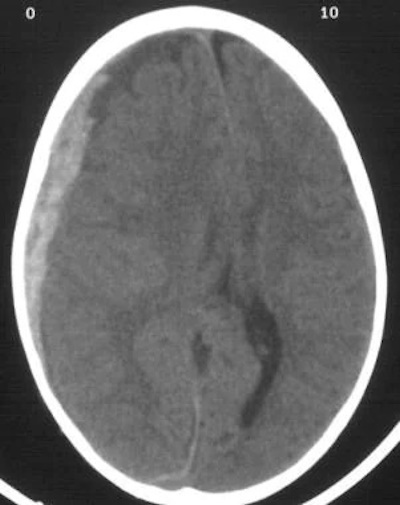
Post Hemicraniectomy – Malignant MCA Infarction
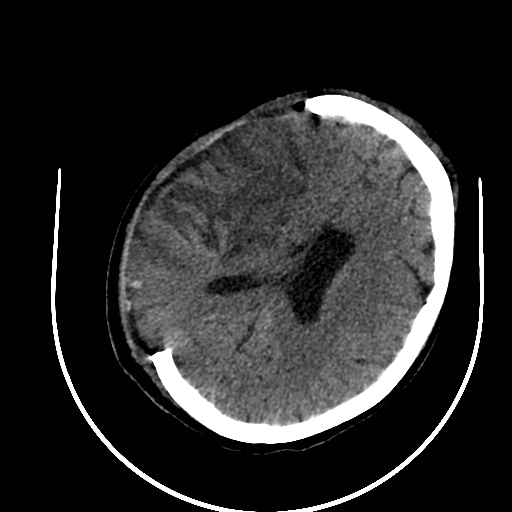
Large MCA infarcts can cause massive cytotoxic oedema with raised intracranial pressure – so-called malignant MCA infarction. Decompressive hemicraniectomy allows the swollen brain to herniate outwards rather than downwards, reducing secondary damage to the brainstem. Post-operative imaging shows bone flap removal with outward bulging of brain tissue. Clinically, surgery improves survival in selected younger patients but many survivors have significant residual disability, so careful shared decision-making is vital.
Artefact
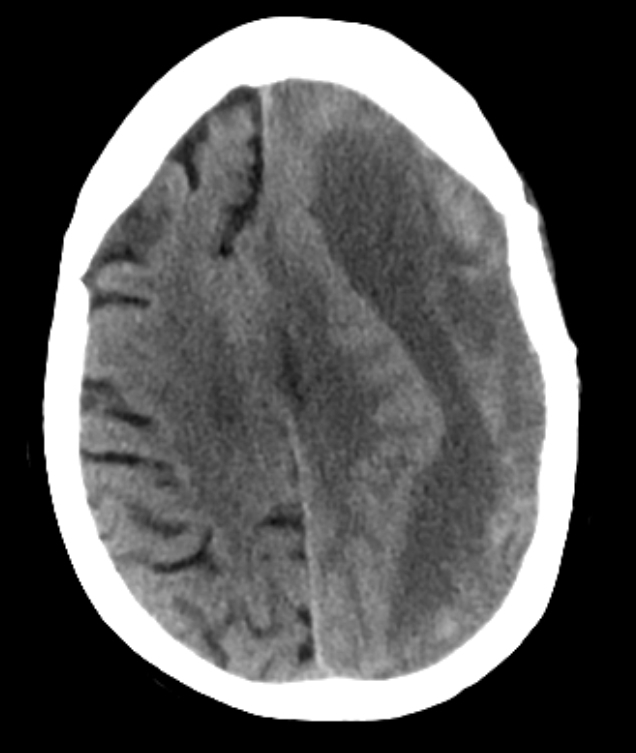
Malignant MCA


Moyamoya
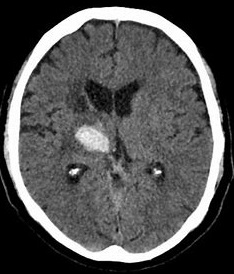
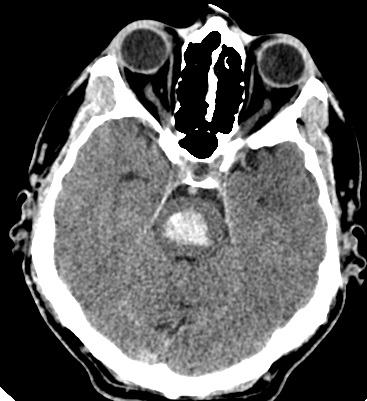
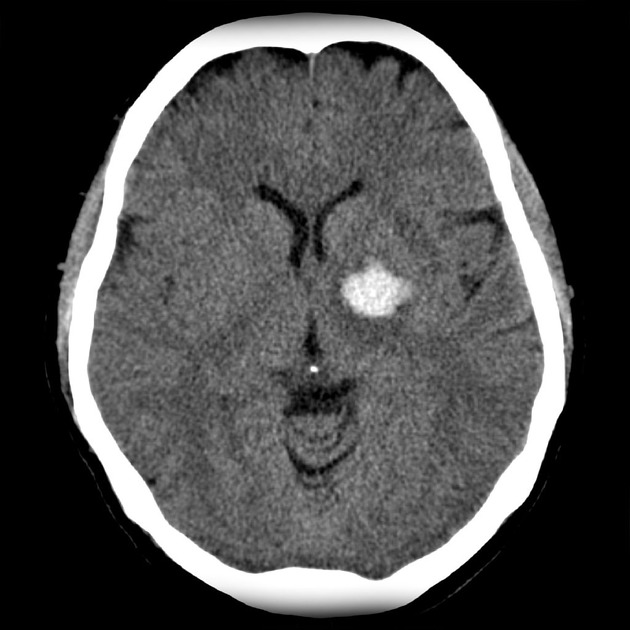
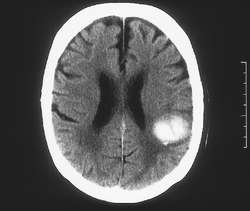
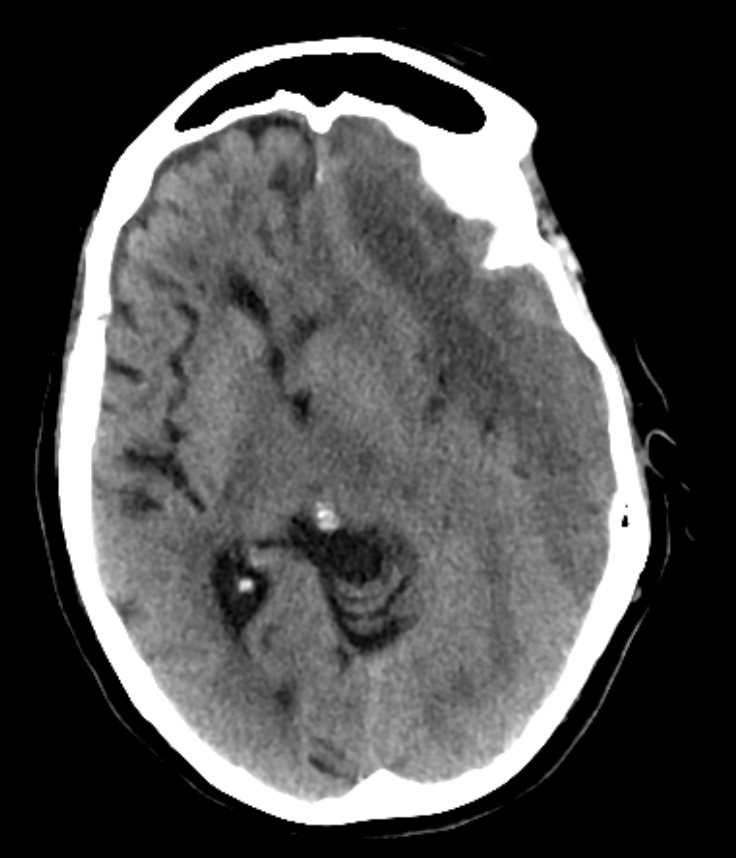
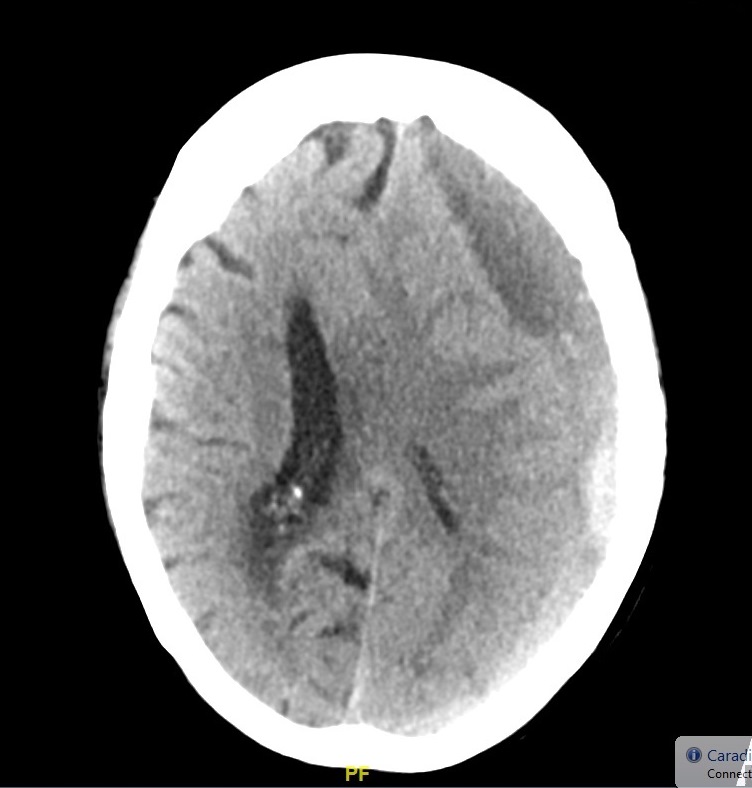
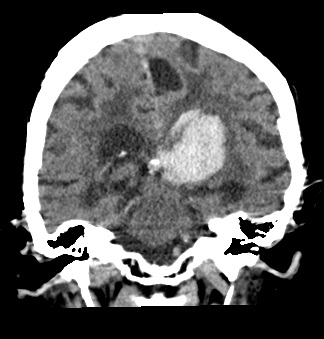
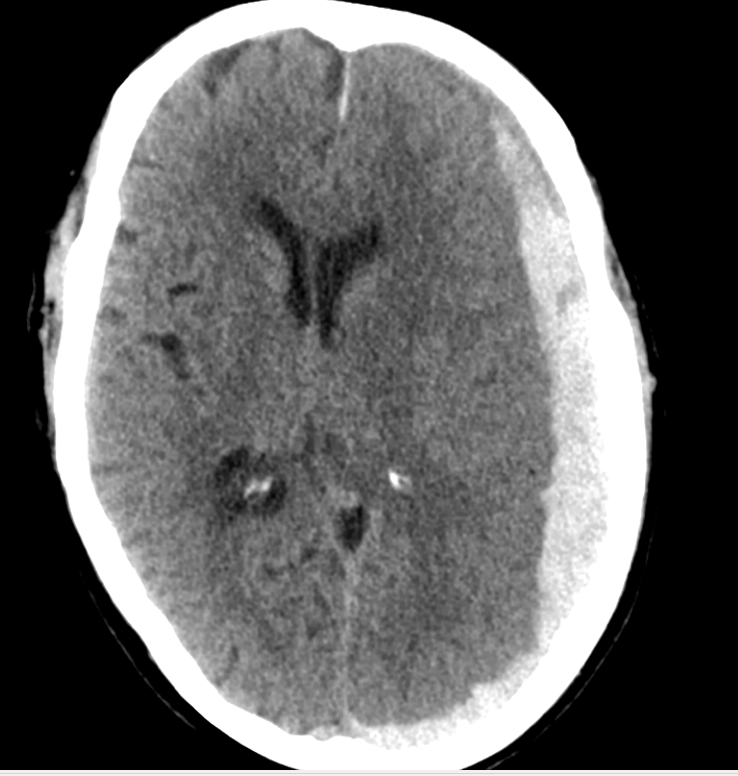
Thalamic Bleed

Basilar Artery



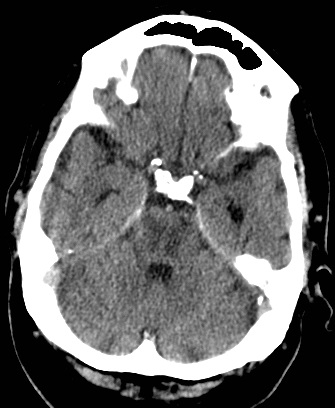
Bilateral Pontine Infarction
ASPECTS

Pontine Bleed
Air Embolism to the Brain

Cerebral air embolism is a rare but devastating cause of acute neurological deficit, usually iatrogenic (line insertion/removal, cardiac or neurosurgery) or due to trauma or diving accidents. CT may show air within cortical sulci or vessels, especially in the arterial circulation. Clinically it can mimic multifocal cortical stroke with seizures and reduced consciousness. Management is supportive with high-flow oxygen and, where available, hyperbaric oxygen; prevention through meticulous line technique is crucial.
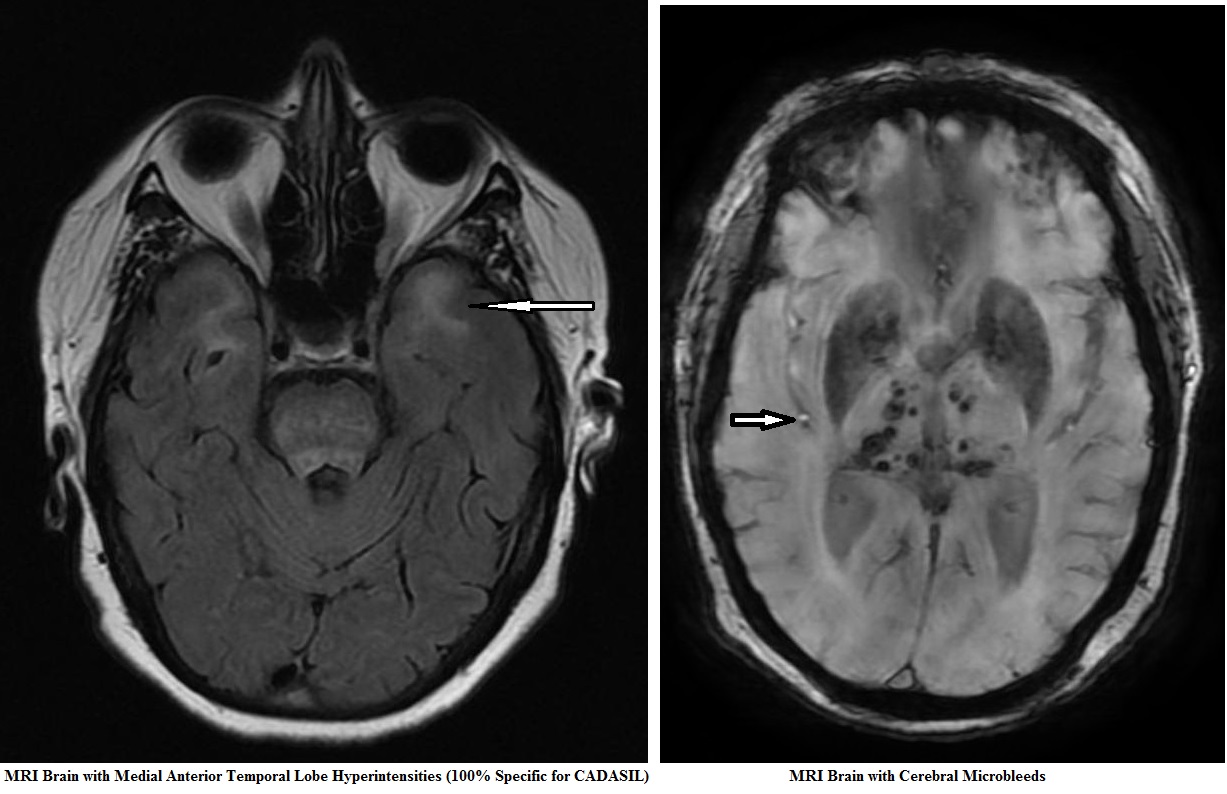
Amyloid Angiopathy
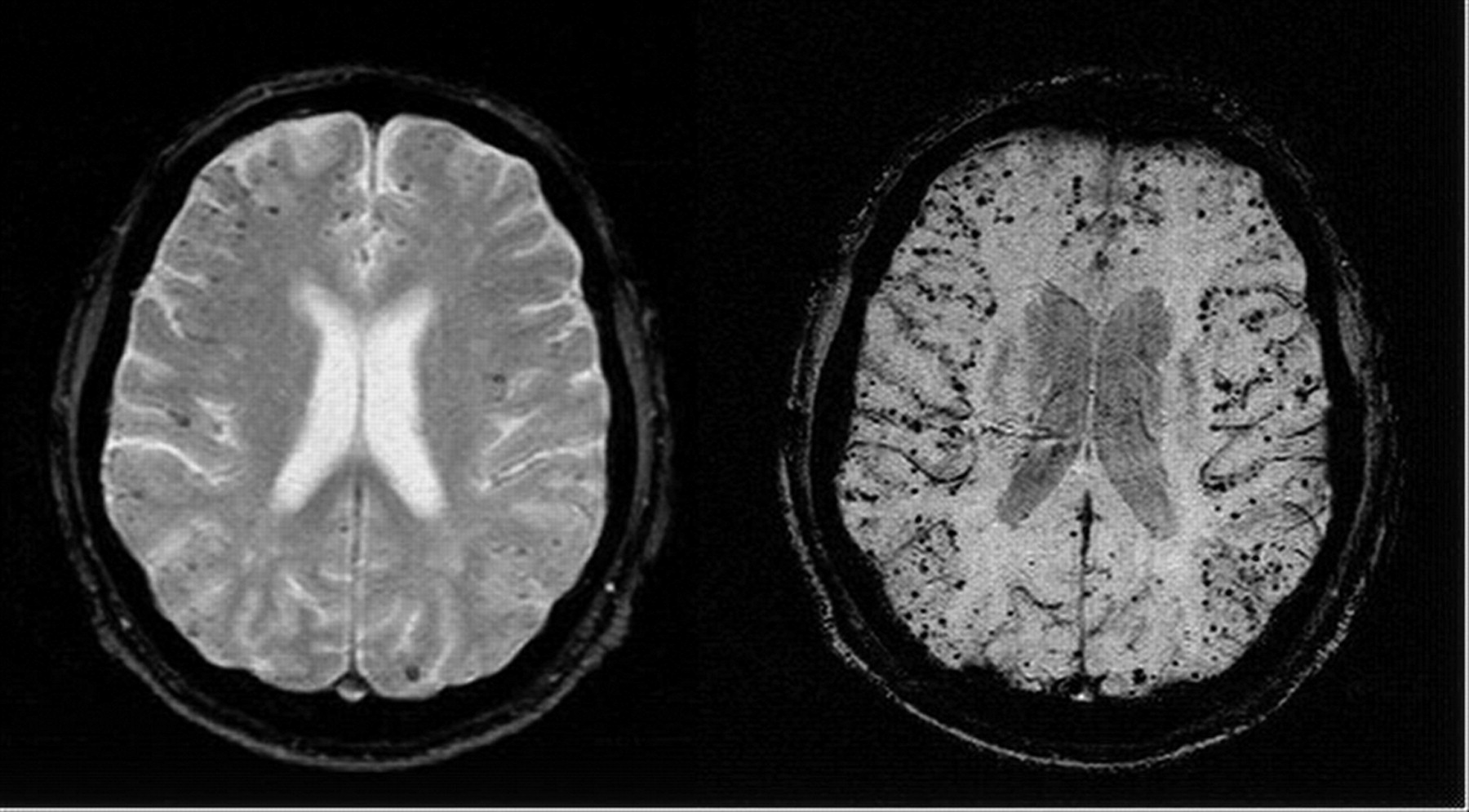
CADASIL
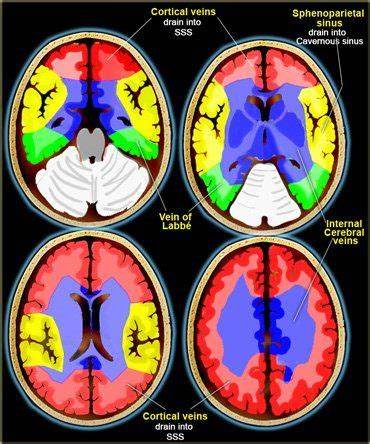
Venous system

Basal Ganglia Bleed
Basal Ganglia Calcification

Primary Brain Tumour as a Stroke Mimic

Primary brain tumours can present with subacute focal deficits that superficially resemble stroke, but the time course is longer (days–weeks), and there may be seizures, headache or cognitive change. Imaging typically shows a space-occupying lesion with mass effect, vasogenic oedema and variable contrast enhancement, rather than a wedge-shaped arterial territory infarct. Recognising tumour as a stroke mimic is important to avoid inappropriate thrombolysis and to ensure urgent neurosurgical/oncology referral.
Angioneurotic Oedema with Alteplase


Orolingual angioedema is an important acute complication of alteplase, seen particularly in patients on ACE inhibitors and in those with large MCA strokes (likely due to impaired bradykinin breakdown and loss of cortical inhibition of autonomic pathways). It often occurs asymmetrically, with tongue swelling on the side contralateral to the infarct. Immediate airway assessment is critical; management includes stopping alteplase, steroids, antihistamines, adrenaline if indicated and early anaesthetic involvement. Education of stroke teams about this complication is essential because early recognition can be life-saving.
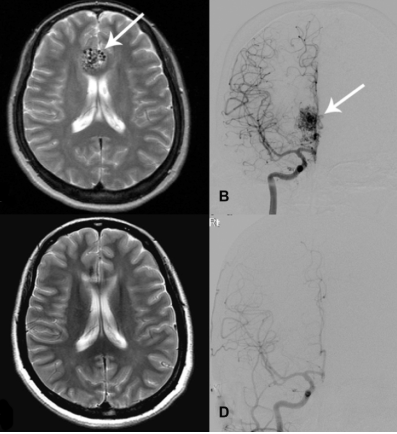
Arteriovenous Malformation
Carotid Dissection>/h1>
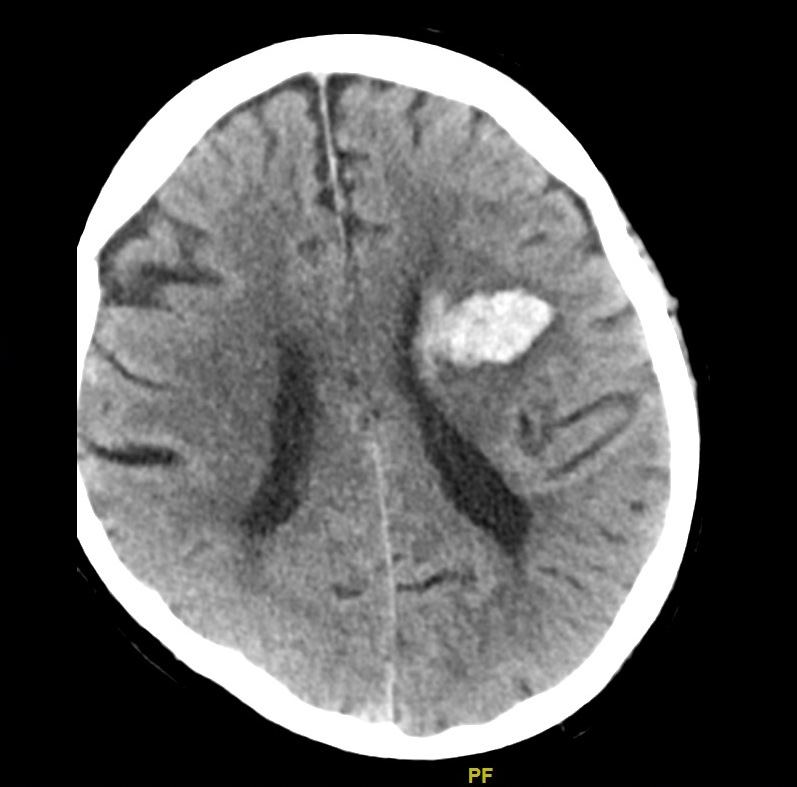
Lobar Bleeds
Cavernoma

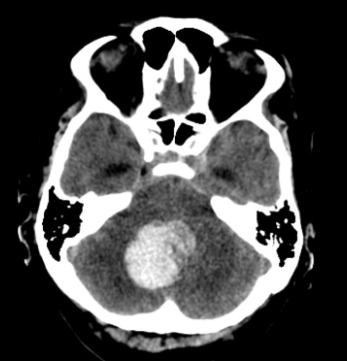
Cerebellar Bleed

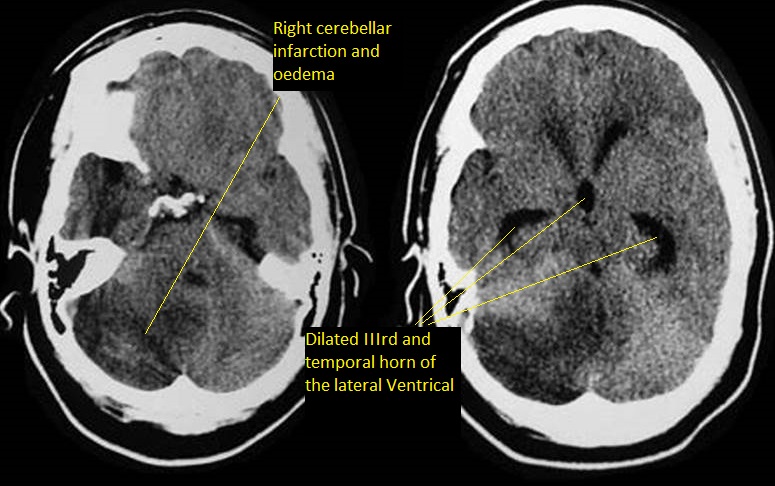
Cerebellar Infarction
Subdural
Cerebral Venous Thrombosis


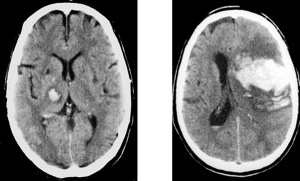
Basal ganglia Bleeds




Subdural
Horner's syndrome


HSV Encephalitis
Hydrocephalus

MELAS
Sturge Weber

Swiss Cheese
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
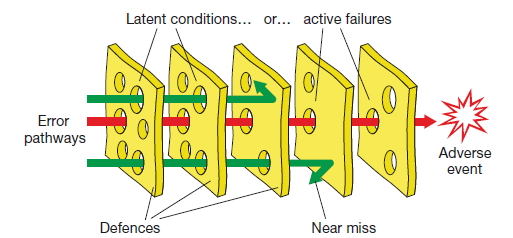
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
