Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Pyloric Stenosis Children
🍼🤮 Hypertrophic pyloric stenosis (HPS) – Infants typically develop hypochloraemic, hypokalaemic metabolic alkalosis. Diagnosis is confirmed with ultrasound (USS) 🖥️.
📖 About
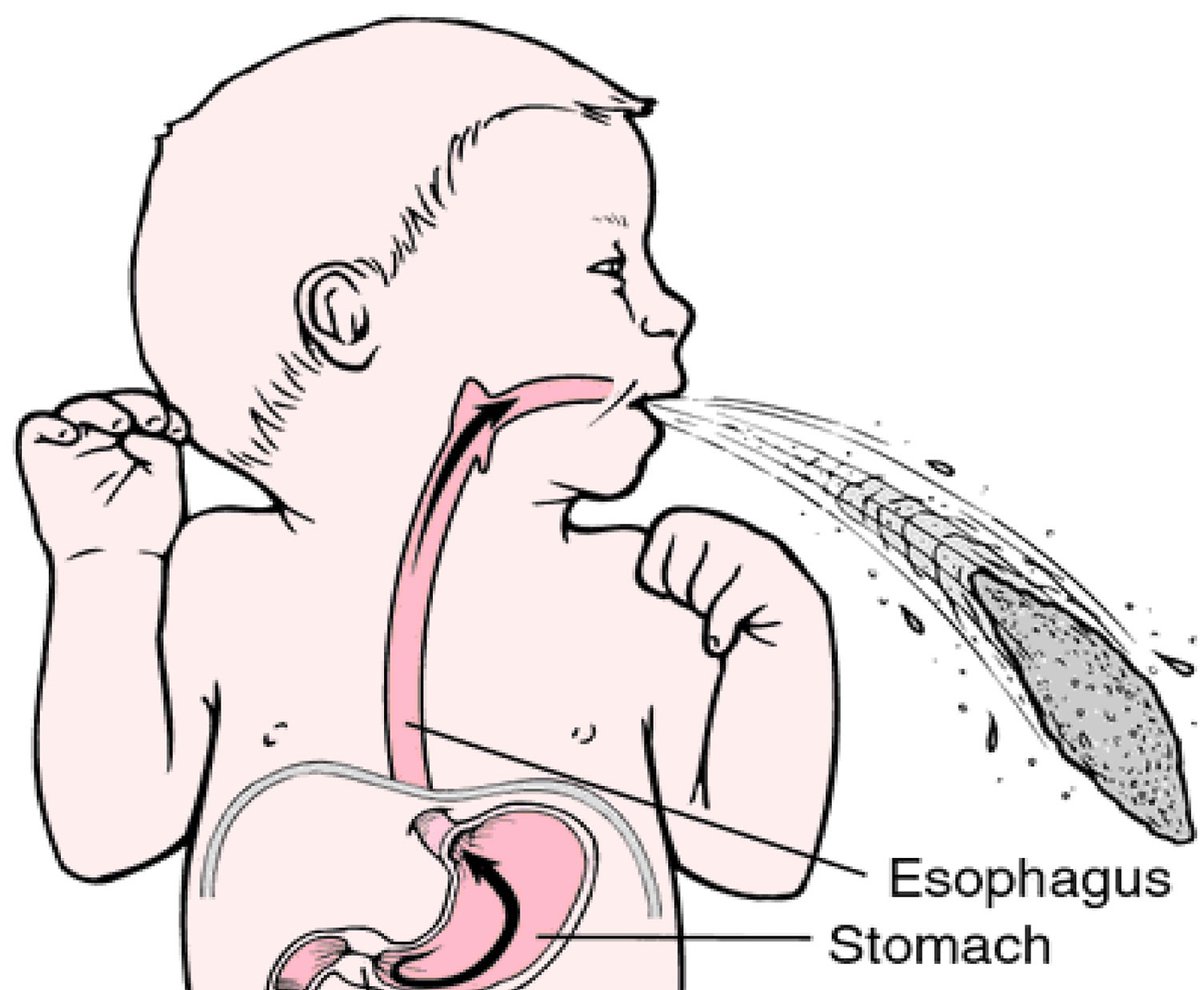
- A common cause of projectile, non-bilious vomiting in infants 🚼.
- Caused by hypertrophy of the pyloric muscle → gastric outflow obstruction.
- Often presents as a surgical emergency but prognosis is excellent once treated.
🧬 Aetiology
- 👦 More common in first-born male infants.
- 📈 Incidence: ~2–4 per 1000 live births.
- 👩👦 Family history (especially maternal side) suggests genetic predisposition.
- Mechanism: pyloric muscle hypertrophy + hyperplasia → narrowing of pyloric channel.
🩺 Clinical Features
👉 To palpate the “olive”: stand on the baby’s left side, palpate with the left hand along the lateral border of the right rectus in the RUQ, ideally during a feed.
- ⏰ Usually presents between 2–7 weeks of age.
- 🤮 Non-bilious, projectile vomiting shortly after feeds.
- 🍽️ Infant remains hungry after vomiting ("hungry vomiter").
- 🚫 No diarrhoea – constipation is common; may pass “starvation stools”.
- ⚠️ Large-volume vomiting within minutes of feeding → weight loss, dehydration.
- 👶 Infant often alert, anxious, and malnourished if untreated.
- ✋ Palpable olive-shaped mass in RUQ = classic sign.
- 👀 Visible peristalsis may be seen across the abdomen after a feed.
🖼️ Image
🔎 Investigations
- Bloods: Classic finding = hypochloraemic, hypokalaemic metabolic alkalosis 🧪. Hypokalaemia usually develops after 2–3 weeks of persistent vomiting.
- Ultrasound (USS): 📏 Diagnostic test of choice – pyloric thickness >3mm and length >15mm = HPS.
- Barium meal: Rarely used; may show “string sign” but generally unnecessary.
💊 Management
- Initial Stabilisation:
- 💧 IV fluid resuscitation + electrolyte correction (replace K⁺ and Cl⁻ until Cl⁻ >90 mmol/L).
- 🛑 Delay surgery until metabolic derangements are corrected (to avoid anaesthetic risk).
- 🧴 NG tube decompression if severe gastric distension.
- Definitive Treatment:
- ✂️ Ramstedt’s pyloromyotomy = standard surgical cure. Muscle split along pylorus, mucosa left intact.
- 🚼 Usually performed laparoscopically in modern practice.
- 📈 Excellent prognosis – most feed normally within 24–48h post-op.
⚠️ Complications if Untreated
- 💧 Severe dehydration & electrolyte imbalance
- 📉 Failure to thrive
- 🫀 Shock & metabolic alkalosis complications (e.g., hypoventilation, seizures)
🧑🏫 Exam Tip
The triad of hypertrophic pyloric stenosis = 1️⃣ Non-bilious projectile vomiting, 2️⃣ Palpable olive-shaped mass, 3️⃣ Visible gastric peristalsis. Always link the metabolic alkalosis (low Cl⁻, low K⁺, raised HCO₃⁻) to the underlying repeated vomiting of gastric contents. This is a classic finals OSCE favourite 🎯.
Cases — Infantile Hypertrophic Pyloric Stenosis
- Case 1 — Classic presentation 🍼: A 6-week-old first-born boy presents with 2 weeks of progressively worsening non-bilious, projectile vomiting after feeds. Exam: visible gastric peristalsis and an olive-shaped mass in the right upper quadrant. Bloods: hypochloraemic, hypokalaemic metabolic alkalosis. Diagnosis: classic hypertrophic pyloric stenosis. Managed with IV fluid and electrolyte correction followed by Ramstedt pyloromyotomy.
- Case 2 — Failure to thrive 📉: A 7-week-old girl presents with poor weight gain, constipation, and frequent vomiting. She is dehydrated with sunken eyes and dry mucous membranes. Blood gas: metabolic alkalosis. Ultrasound: elongated, thickened pylorus. Diagnosis: pyloric stenosis with dehydration and failure to thrive. Managed with urgent fluid/electrolyte replacement and planned surgical pyloromyotomy.
- Case 3 — Atypical late presentation ⚠️: A 12-week-old boy presents with persistent vomiting and irritability. Exam: abdominal distension and metabolic alkalosis. History of delayed diagnosis due to atypical age. Ultrasound confirms pyloric stenosis. Diagnosis: delayed diagnosis of pyloric stenosis. Managed with fluid resuscitation, correction of electrolytes, and surgery.
Teaching Point 🩺: Infantile hypertrophic pyloric stenosis usually presents at 2–8 weeks of life, more common in first-born males. Key features: projectile non-bilious vomiting, palpable olive-shaped mass, visible peristalsis. Biochemical hallmark: hypochloraemic, hypokalaemic metabolic alkalosis. Management = correct fluids/electrolytes first, then Ramstedt pyloromyotomy.
Categories
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology