| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Cryptogenic stroke
Related Subjects: |Anaromy and Physiology of the Brain |Cryptogenic stroke
Cryptogenic stroke describes an ischaemic stroke with no clear cause despite a structured diagnostic work-up. It is common in stroke practice, particularly in younger adults, and is best thought of as a working label rather than a final diagnosis. Many of these strokes are ultimately due to occult embolic sources such as paroxysmal atrial fibrillation (AF), patent foramen ovale (PFO), or non-stenotic atherosclerotic plaque.
📚 Definitions
| Term | Short Definition | Key Points |
|---|---|---|
| Cryptogenic stroke | Brain infarction not clearly attributable to large artery atherosclerosis, small vessel disease, or definite cardioembolism after adequate investigation. | A TOAST “stroke of undetermined aetiology”. Includes: negative evaluation, multiple possible causes, or incomplete work-up. A heterogeneous group. |
| ESUS (Embolic Stroke of Undetermined Source) | Subset of cryptogenic stroke that is non-lacunar on imaging and appears embolic, but no major cardioembolic source or significant proximal stenosis is found. | Requires a minimum standard work-up (brain imaging, vascular imaging, echocardiography, rhythm monitoring, basic labs). Used mainly in research; trials have not shown benefit of routine anticoagulation over antiplatelet therapy. |
📊 Epidemiology
- Cryptogenic strokes make up roughly one quarter to one third of ischaemic strokes, and a higher proportion in younger patients.
- ESUS accounts for around 15–30% of ischaemic strokes in many series.
- Recurrent stroke risk is clinically important (annual recurrence ≈ 4–5% for ESUS), so optimising secondary prevention is critical.
🧬 Pathophysiology & Mechanisms
“Cryptogenic” does not mean “no cause”; it means “no cause identified yet with standard tests”. In many patients, the underlying mechanism is embolic. Commonly suspected mechanisms include:
- Occult atrial fibrillation or atrial cardiomyopathy (paroxysmal AF not seen on initial ECG/24-hour trace).
- PFO and other interatrial shunts → paradoxical embolism from venous thrombus.
- Non-stenotic atherosclerotic plaque (e.g. ulcerated or high-risk carotid or aortic arch plaques <50% stenosis).
- Cardiomyopathies or structural cardiac lesions (LV thrombus, atrial myxoma, valvular disease).
- Systemic / haematological causes – cancer-associated thrombosis, antiphospholipid syndrome, inherited thrombophilia (especially in younger patients), other prothrombotic states.
🩺 Diagnostic Work-Up
Baseline evaluation (for all ischaemic strokes):
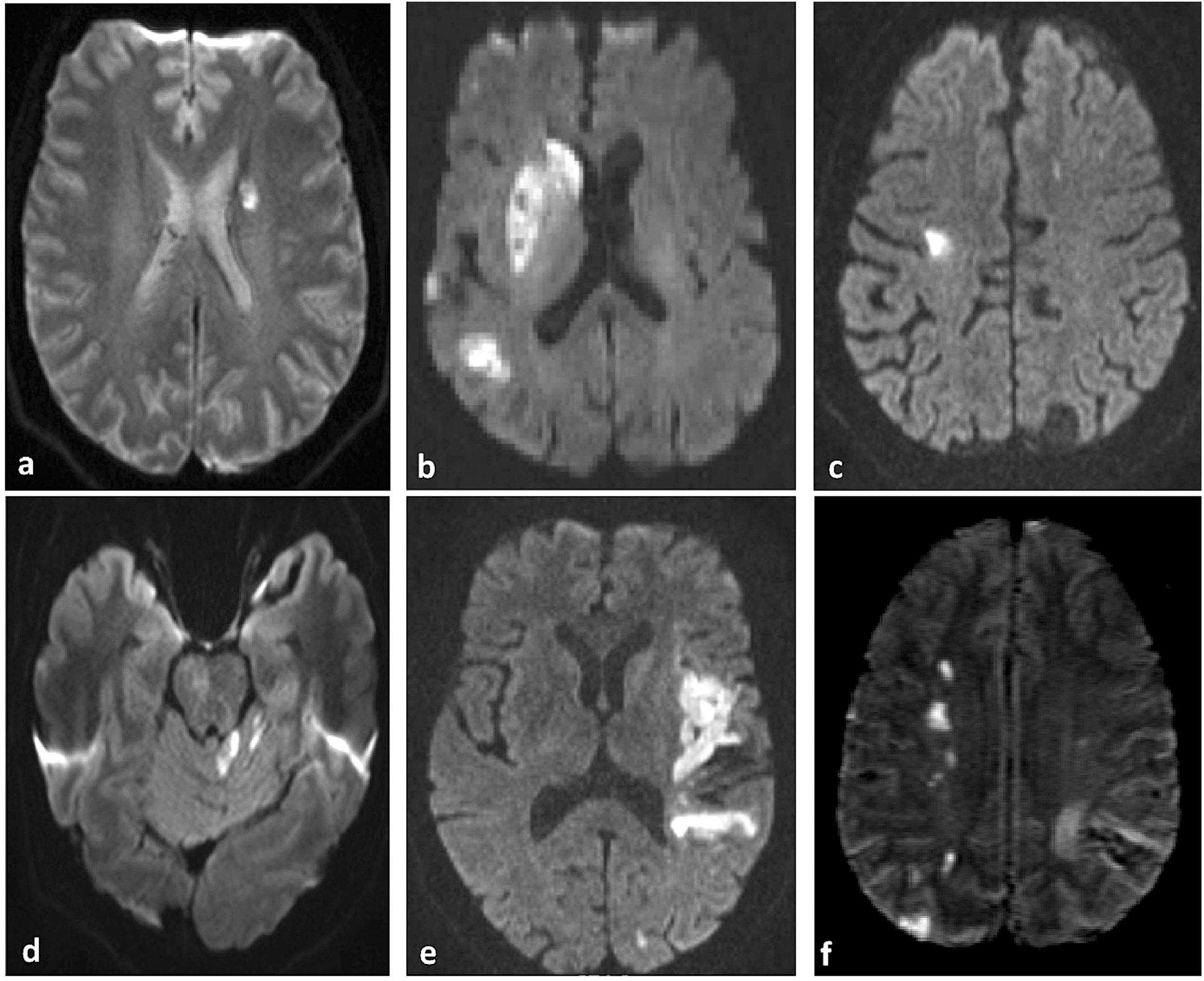
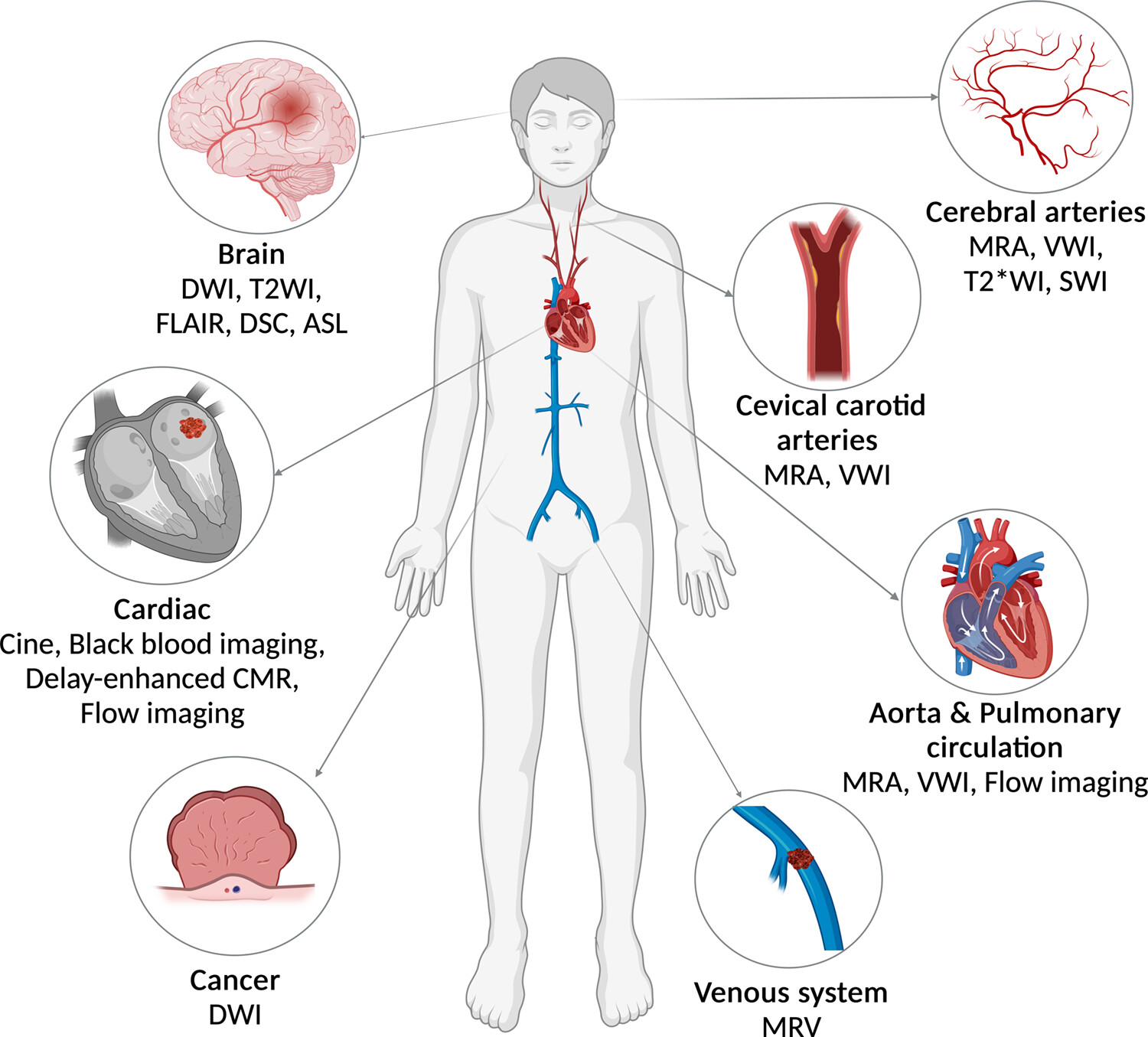
- Urgent brain imaging – non-contrast CT ± MRI to confirm infarction pattern (cortical vs lacunar, single vs multiple territories).
- Vascular imaging of intra- and extracranial arteries – CT angiography, MR angiography, or carotid ultrasound as appropriate.
- Cardiac rhythm assessment – 12-lead ECG and at least 24-hour ECG monitoring (Holter or in-hospital telemetry).
- Transthoracic echocardiogram (TTE) to look for LV dysfunction, thrombus, cardiomyopathy, valvular disease.
- Routine bloods – FBC, U&Es, LFTs, lipids, HbA1c, coagulation screen; consider inflammatory markers.
Extended work-up (to justify the “cryptogenic” label):
- Prolonged rhythm monitoring (e.g. 7–14 day Holter, external loop recorder, or implantable loop recorder) to uncover paroxysmal AF.
- Transoesophageal echo (TEE) where available – more sensitive for:
- Left atrial/appendage thrombus.
- Aortic arch atheroma.
- PFO, atrial septal aneurysm, and other shunts (often with bubble study).
- Screen for PFO and venous thrombosis (e.g. leg Doppler) in younger patients with cortical infarcts and minimal risk factors.
- Targeted tests in selected cases:
- Thrombophilia and antiphospholipid testing in younger patients or those with history of VTE, miscarriage, or autoimmune disease.
- CT chest/abdomen/pelvis, tumour markers, or PET if cancer is suspected.
- Vasculitis / connective tissue disease screen if systemic features are present.
A stroke should only be labelled “cryptogenic” after a reasonable, age-appropriate work-up. In practice, the depth of investigation will be influenced by age, vascular risk profile, and local pathways.
💊 Secondary Prevention & Management
1️⃣ Antithrombotic therapy
- For most patients with cryptogenic stroke (including ESUS) and no AF or other indication for anticoagulation, use:
- Single antiplatelet therapy – e.g. aspirin, clopidogrel, or aspirin–dipyridamole (follow local / national guidelines).
- Large ESUS trials (e.g. rivaroxaban vs aspirin, dabigatran vs aspirin, apixaban vs aspirin) have not shown routine DOAC therapy to be superior to antiplatelet therapy, and bleeding risk is higher. So empiric anticoagulation for ESUS alone is not recommended.
- If AF or another definite cardioembolic source is subsequently detected, switch to long-term oral anticoagulation (usually a DOAC, unless contra-indicated).
2️⃣ Risk factor modification
- Blood pressure – treat hypertension with a target consistent with secondary prevention guidelines.
- Lipids – high-intensity statin therapy for most patients; add ezetimibe or PCSK9 inhibitor in very high-risk cases if targets not met.
- Diabetes & metabolic risk – optimise glycaemic control; address obesity and metabolic syndrome.
- Lifestyle – smoking cessation, safe alcohol limits, regular exercise, healthy diet (Mediterranean-style), weight management.
3️⃣ PFO and structural cardiac interventions
- In carefully selected patients (<60 years, non-lacunar infarct, no alternative cause, high-risk PFO features), PFO closure plus
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
