| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Myasthenia Gravis
🔗 Related Subjects: | 💪 Myasthenia Gravis | ⚡ Lambert-Eaton syndrome (LEMS)
😴 Fluctuating, fatigable muscle weakness of eye, bulbar, respiratory, and limb muscles.
| 🚨 Initial Management of Myasthenic Crisis |
|---|
|
📖 About
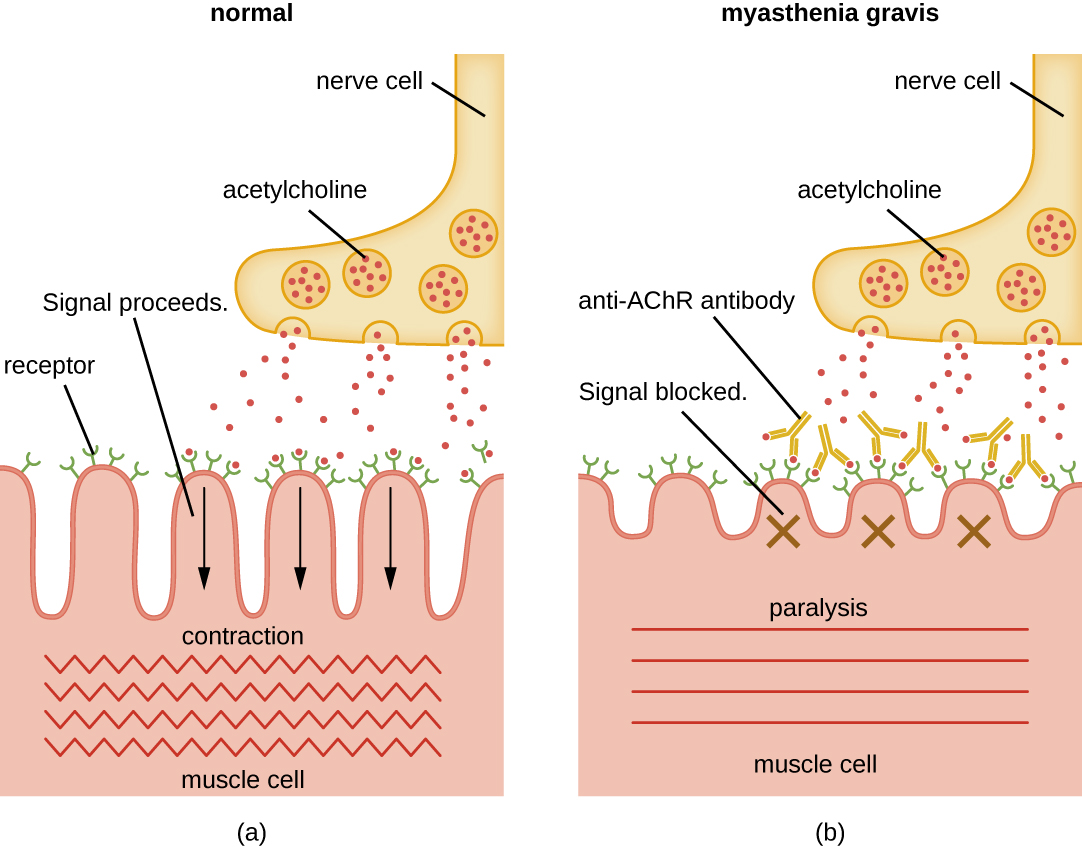
- 🧬 Myasthenia Gravis (MG) is an autoimmune disorder where antibodies target nicotinic acetylcholine receptors, causing fatigable weakness.
🧪 Aetiology
- 🔑 90% have anti-AChR antibodies.
- 🦠 Anti-MuSK antibodies in some AChR-negative patients.
- 🏹 Anti-Titin & anti-RyR often seen with thymomas.
- 🧨 Pathology: complement-mediated damage → ↓ ACh receptors → impaired neuromuscular transmission.
🔗 Clinical Associations
- 🦋 Autoimmune: RA, SLE, Sjögren’s, sarcoidosis.
- 🩸 Haematological: pernicious anaemia.
- 🧩 Others: polymyositis, ulcerative colitis, pemphigus.
🧩 Clinical Features
- ♻️ Fluctuating weakness worsens with activity (fatigability).
- 👀 Ocular: diplopia, ptosis (pupil spared).
- 👁️ Cogan’s lid twitch: classic eyelid sign.
- 🫁 Respiratory: may lead to crisis with failure.
- 🍽️ Bulbar: dysphagia, dysarthria, chewing difficulty, abnormal smile.
- ⚠️ Myasthenic crisis: severe respiratory muscle weakness → urgent PLEX/IVIg.
- 🤰 Pregnancy: symptoms often worsen in 1st trimester; neonatal MG possible.

🧾 Differential Diagnosis
- ⚡ Lambert-Eaton Myasthenic Syndrome (LEMS).
- ☠️ Botulism.
- 💊 Drug-induced (penicillamine, aminoglycosides).
- 🧿 Chronic Progressive External Ophthalmoplegia (CPEO).
🔎 Investigations
- 🧪 Anti-AChR antibodies (90%).
- 🧪 Anti-MuSK if AChR negative.
- ⚡ Neurophysiology: RNS or SFEMG → impaired transmission.
- 💉 Tensilon (edrophonium) test → transient improvement.
- 🧊 Ice pack test → improves ptosis.
- 🫀 Chest CT/MRI → thymoma screening.
- 🦋 TFTs → check for thyroid disease.
❓ Key Diagnostic Questions
- Is the patient AChR or MuSK seropositive/seronegative?
- Is a thymoma present?
- Ocular or generalised symptoms?
- Could this be congenital MG?
🚫 Drugs to Avoid in MG
| Drug | Mechanism |
|---|---|
| 💊 Aminoglycosides, Phenytoin, Lignocaine, Beta-blockers, Quinidine | ↓ ACh release at neuromuscular junction |
| 💊 Penicillamine | Induces AChR antibodies |
| 💊 Lithium | Causes MG-like weakness |
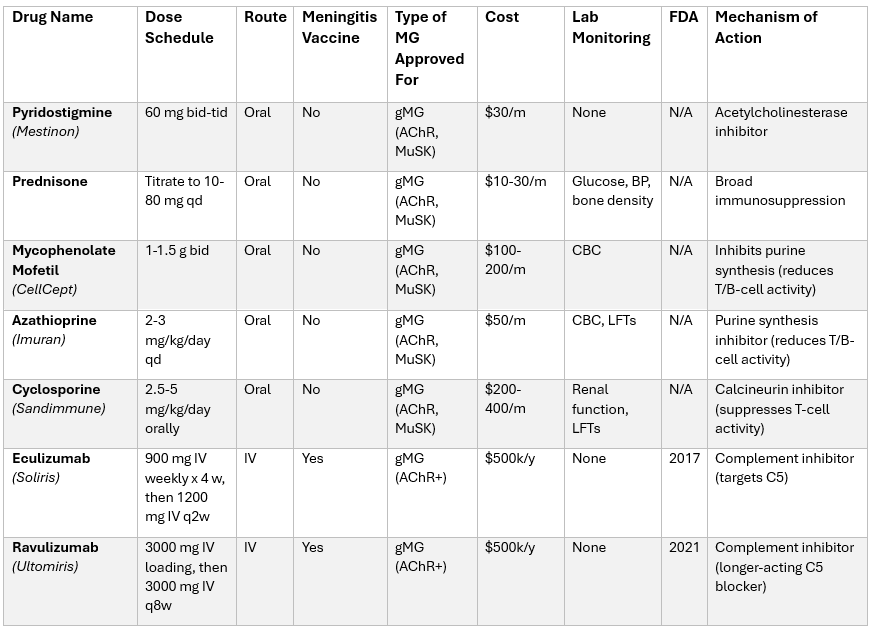
💊 Medications in MG
🛠️ Management
- 💊 Pyridostigmine: 30–60 mg PO q4h; adjust to symptoms.
- 🧴 Prednisolone: dose escalation; esp. effective in MuSK+ disease.
- 🧬 Immunosuppressants: azathioprine, mycophenolate, methotrexate, cyclosporine.
- 🧪 Refractory MG: IVIg, plasmapheresis, rituximab.
- 🔪 Thymectomy: for all MG with thymoma; improves long-term disease control.
- 🚑 Crisis: IVIg or plasmapheresis urgently.
- 🤰 Pregnancy: pyridostigmine safe; steroids if required; avoid teratogenic immunosuppressants.
- 🚫 Avoid MG-worsening drugs (aminoglycosides, tetracyclines, phenytoin, penicillamine).
📚 References
Cases — Myasthenia Gravis (MG)
- Case 1 — Ocular Myasthenia 👁️: A 28-year-old woman reports drooping of her right eyelid that worsens by evening and double vision after prolonged reading. Exam: fatigable ptosis and ophthalmoparesis. No limb weakness. Diagnosis: Ocular myasthenia gravis. Management: Pyridostigmine (acetylcholinesterase inhibitor); monitor for progression to generalised MG; immunosuppressants if refractory.
- Case 2 — Generalised MG with Bulbar Symptoms 🗣️: A 45-year-old man presents with fluctuating limb weakness, nasal speech, and difficulty swallowing, especially late in the day. Exam: fatigable proximal weakness, weak neck flexion, and reduced palatal movement. Diagnosis: Generalised MG with bulbar involvement. Management: Pyridostigmine; immunosuppression (prednisolone, azathioprine); screen for thymoma with CT chest; MDT support (speech and physio).
- Case 3 — Myasthenic Crisis in ICU ⚠️: A 52-year-old woman with known MG develops pneumonia and acute worsening weakness, now with difficulty speaking and shallow breathing. Exam: weak cough, reduced vital capacity. Diagnosis: Myasthenic crisis precipitated by infection. Management: Admit to ICU; ventilatory support if needed; IV immunoglobulin or plasma exchange; optimise infection treatment; adjust long-term immunotherapy.
Teaching Commentary 🧠
Myasthenia gravis is an autoimmune disorder of the neuromuscular junction, usually due to antibodies against the ACh receptor (AChR) or MuSK. Hallmarks: fluctuating, fatigable weakness, classically ocular (ptosis, diplopia), bulbar (dysarthria, dysphagia), and proximal limb/neck. Reflexes and sensation remain intact. Red flags: myasthenic crisis with respiratory weakness — life-threatening. Dx: AChR/MuSK antibodies, EMG (decrement on repetitive stimulation), CT chest (thymoma). Rx: Pyridostigmine, steroids/immunosuppressants, IVIG/plasma exchange for crisis, thymectomy if thymoma. Avoid drugs that worsen MG (aminoglycosides, beta-blockers, magnesium).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
