| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Malnutrition universal screening tool (MUST)
Related Subjects: |Malnutrition universal screening tool (MUST) |Body Mass Index |Peripherally inserted central catheters (PICC) |Refeeding syndrome
🥗 Introduction
- The Malnutrition Universal Screening Tool (MUST) is the most widely used, validated screening tool for identifying adults at risk of malnutrition in hospitals, GP practices, care homes, and community settings in the UK.
- Developed by the Malnutrition Advisory Group of BAPEN, it is recommended by NICE and incorporated into NHS nutrition policies.
- MUST provides a structured, rapid, evidence-based way to detect malnutrition and trigger appropriate interventions.
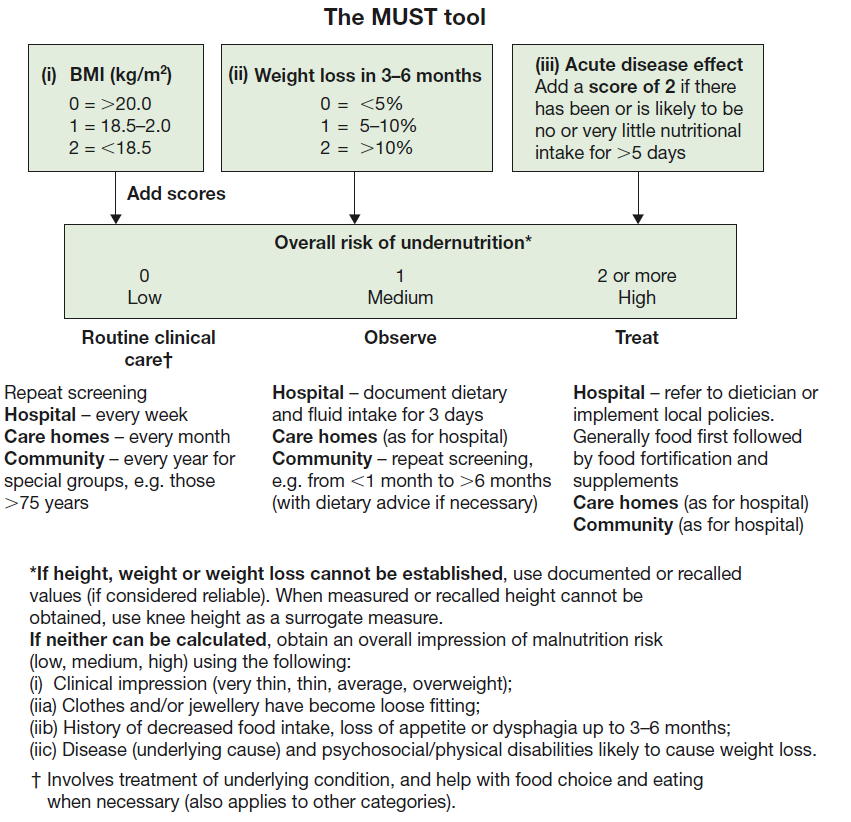
📊 Diagram
📌 Background and Rationale
Malnutrition is common but under-recognised: around 30% of hospital inpatients and 35% of care home residents are affected. It is associated with:
- ⚠️ Increased morbidity & complications (poor wound healing, infections, frailty).
- ⏳ Longer hospital stays and delayed recovery.
- 💷 Higher healthcare costs (£19.6 billion annually in the UK).
MUST was created as a simple, reproducible tool that could be applied across all healthcare environments and by different professionals.
🎯 Purpose of MUST
- 🔎 Early detection: Identify adults at risk before complications arise.
- 📈 Monitoring: Track changes in risk status over time.
- 🩺 Treatment planning: Stratify patients into low, medium, or high risk, guiding nutrition interventions.
- 📊 Audit & governance: Standardises malnutrition data collection for quality improvement.
🧮 Components and Scoring
MUST uses a simple 3-step process:
- BMI (kg/m²):
- >20 = 0 points
- 18.5–20 = 1 point
- <18.5 = 2 points
- Unplanned weight loss (3–6 months):
- <5% = 0 points
- 5–10% = 1 point
- >10% = 2 points
- Acute disease effect: If patient is acutely unwell and has had, or is likely to have, no nutritional intake for >5 days → +2 points.
Total score:
- 0 = Low risk → Routine care.
- 1 = Medium risk → Observe & repeat screening (weekly in hospital, monthly in care homes, yearly in GP/community).
- ≥2 = High risk → Refer to dietitian, initiate nutritional support, and monitor closely.
🏥 Clinical Applications
- 🧾 Hospital wards: Used on admission to trigger dietitian referral if needed.
- 🏡 Community & care homes: Enables carers and nurses to detect at-risk patients early.
- 🧑⚕️ Primary care: GPs can use MUST scores to support decisions about supplements (e.g. oral nutritional support like Fortisip).
- 📉 Palliative care: Helps balance nutritional intervention with patient comfort and goals of care.
⚠️ Limitations & Considerations
- 📏 BMI inaccuracies: May be misleading in oedema, ascites, or amputations → use surrogate measures (mid-upper arm circumference).
- 👵 Elderly patients: Sarcopenia can exist even with normal BMI (masked malnutrition).
- 🧮 Scoring errors: Staff training is essential to ensure accurate measurement and risk interpretation.
✅ Conclusion
The MUST Tool is a quick, evidence-based method to detect malnutrition risk in adults. By combining BMI, weight loss, and acute illness, it provides a robust framework for early intervention. Routine use of MUST improves patient outcomes, reduces complications, and lowers healthcare costs — making it a cornerstone of nutritional care in the NHS and beyond.
📚 References
- BAPEN: MUST Toolkit
- NICE CG32: Nutrition Support in Adults
- Elia M. MUST Report, BAPEN, 2003
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
