| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Blood Transfusion Reactions
📑 Crib Sheet: Transfusion Reactions
All patients receiving a blood component transfusion are at risk of an adverse transfusion reaction. ⚠️ Severe reactions (e.g. TRALI, TACO, acute haemolysis) must be reported to the hospital blood bank.
📊 UK SHOT Data (2017)
- 2 million transfusions → 372 acute reactions (≈1 in 5,376)
- 42 haemolytic reactions (≈1 in 48,000)
- 3 TRALI (≈1 in 666,000)
- 92 TACO (≈1 in 22,000)
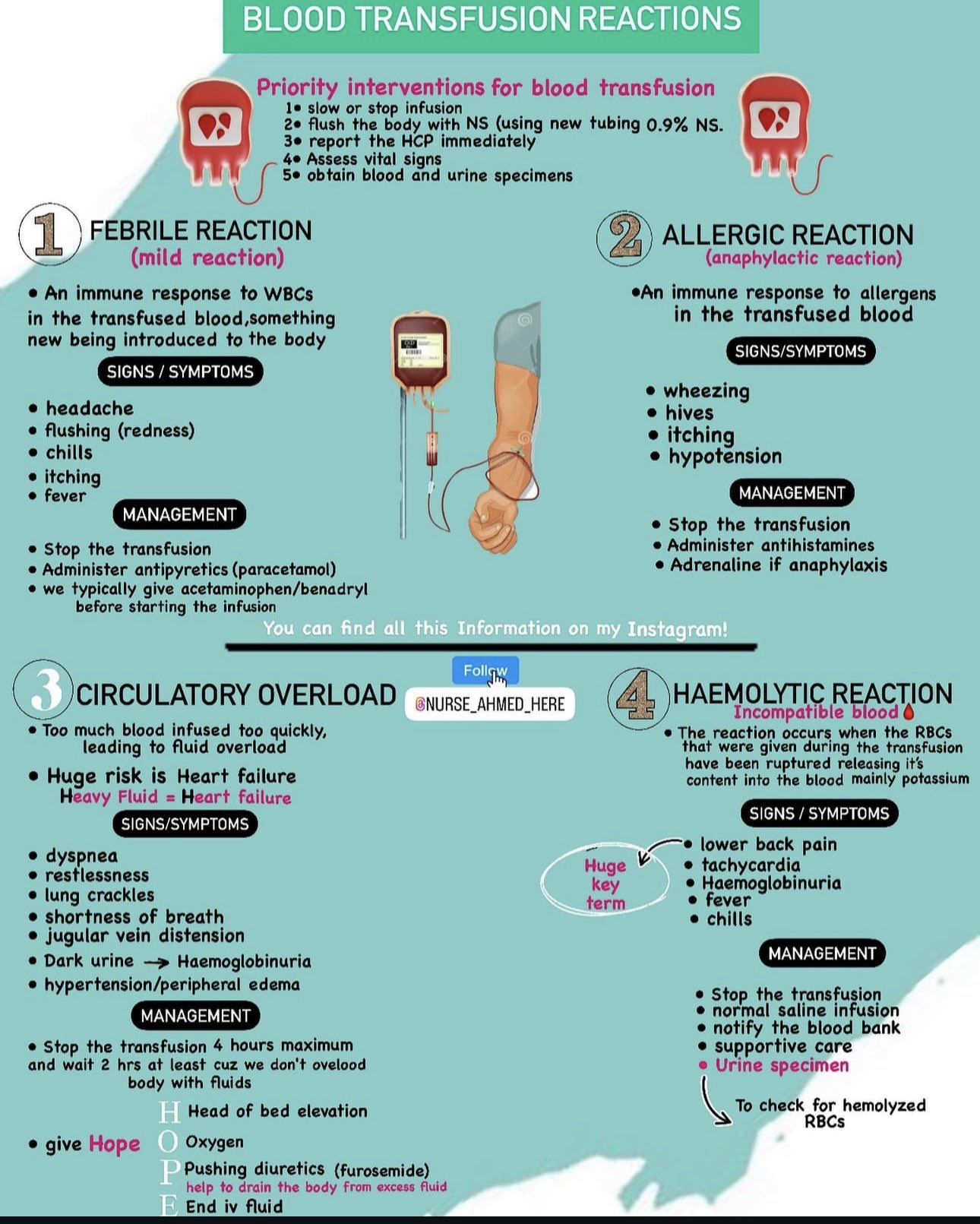
🚨 If Reaction Suspected
- 🛑 Stop the transfusion immediately.
- Assess with NEWS + ABCDE.
- Check correct patient and correct blood.
- Maintain IV line with normal saline if needed.
- Record observations every 15 min.
- Haemolysis or bacterial infection = most serious complications.
🌡️ Febrile Non-Haemolytic Reaction
- Occurs in ≈1% of transfusions (RBCs, platelets, FFP).
- Cause: Plasma pyrogens or leucocyte antibodies.
- Clinical: 30 min after start → fever (↑1–2°C to 38–39°C), chills, malaise, urticaria, pruritus.
- Management: Stop/slow transfusion, give paracetamol 1 g PO/IV, ± chlorphenamine. Restart if symptoms settle.
- Close monitoring q15min.
💥 Acute Haemolytic Reaction (ABO Incompatibility)
- Usually due to clerical/crossmatch error → 10% mortality.
- Clinical: Within minutes → fever, chills, hypotension, tachycardia, dyspnoea, chest/back pain, vomiting, haemoglobinuria.
- Tests: FBC, U&E, LFT, coagulation, DAT, lactate, blood cultures, urine Hb.
- Management:
- Stop transfusion, check IDs, change tubing.
- IV saline → diuresis (insert catheter, monitor urine output).
- IV furosemide if volume status allows.
- High-flow oxygen, monitor for AKI/DIC.
- Discuss with haematology/ICU, return blood units to lab.
- Consider antibiotics if sepsis in differential.
🤧 Anaphylaxis
- Symptoms: Wheeze, swelling, pain, hypotension, collapse.
- May occur in IgA deficiency exposed to donor IgA.
- Treatment: Stop transfusion, oxygen, IM adrenaline 0.5 mg, IV fluids. Consider IV hydrocortisone + chlorphenamine.
🦠 Bacterial Contamination
- Fever, hypotension, septic shock, DIC.
- Usually immediate, often lethal.
- Treatment: Stop transfusion, send blood cultures, follow sepsis 6, start IV antibiotics.
🧬 Viral Transmission
- Screened for: HBV, HCV, HIV, HTLV.
- CMV-negative blood: required for bone marrow & organ transplant patients.
- Other rare risks: syphilis, malaria, toxoplasmosis.
💧 TACO (Transfusion-Associated Circulatory Overload)
- Acute dyspnoea, tachycardia, raised JVP, pulmonary oedema on CXR.
- Prevention: Give slowly (over 3–4 hrs) + diuretics.
- Treatment: Oxygen, IV diuretics, manage as cardiogenic pulmonary oedema.
🌫️ TRALI (Transfusion-Related Acute Lung Injury)
- Due to donor anti-leucocyte antibodies.
- Acute breathlessness, pulmonary oedema, cough.
- CXR: Bilateral infiltrates (non-cardiogenic oedema).
- Treatment: Supportive → oxygen, treat like ARDS. Prognosis usually good.
🧾 Other Rare Reactions
- Transfusion-Related GvHD: Immunocompromised host → fever, rash, liver dysfunction 1 wk later. Prevent with irradiated blood.
- Post-Transfusion Purpura: 10–14 days later → severe thrombocytopenia due to anti-HPA-1a. Treat with IVIg ± plasma exchange.
📚 References
Clinical Pearl: Always suspect ABO mismatch if severe symptoms occur within minutes of starting a transfusion. If breathless, distinguish TACO (fluid overload) vs TRALI (immune-mediated lung injury) — both need stopping transfusion immediately, but management differs.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
