| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Hypothyroidism
💡 Always start with a lower dose of levothyroxine in the elderly and in those with angina or heart failure, to avoid precipitating arrhythmia or ischaemia.
📖 Introduction
- Hypothyroidism = inadequate thyroxine production for normal metabolism.
- Thyroid produces both T4 and T3, but T3 is the active form at tissue level.
- TSH is the best single test: ↑TSH is a highly sensitive marker of primary hypothyroidism.
- A normal TSH in a treated patient usually indicates adequate replacement and euthyroidism.
⚙️ Aetiology
- Primary hypothyroidism (95%): intrinsic thyroid failure (iodine deficiency, autoimmune thyroiditis, post-surgical, post-radioiodine).
- Secondary hypothyroidism: pituitary or hypothalamic disease → insufficient TSH secretion (TSH low/normal despite low T4).
🧬 Causes of Primary Hypothyroidism
- Iodine deficiency: still the most common cause worldwide.
- Autoimmune: Hashimoto’s thyroiditis (± goitre) or atrophic thyroiditis (no goitre). Often associated with other autoimmune disease.
- Post-ablative: surgery, radioiodine, external radiotherapy.
- Drugs: carbimazole, propylthiouracil, lithium, amiodarone, interferons, thalidomide, rifampicin, excess iodine (e.g. kelp supplements).
- Transient thyroiditis: subacute (de Quervain’s), often post-viral, painful goitre.
- Postpartum thyroiditis: transient hyper → hypo → recovery within 1 year.
- Infiltrative disease: amyloidosis, sarcoidosis, haemochromatosis, TB, scleroderma.
- Congenital: agenesis, hypoplasia, ectopic gland, or enzyme defects (causes cretinism if untreated).
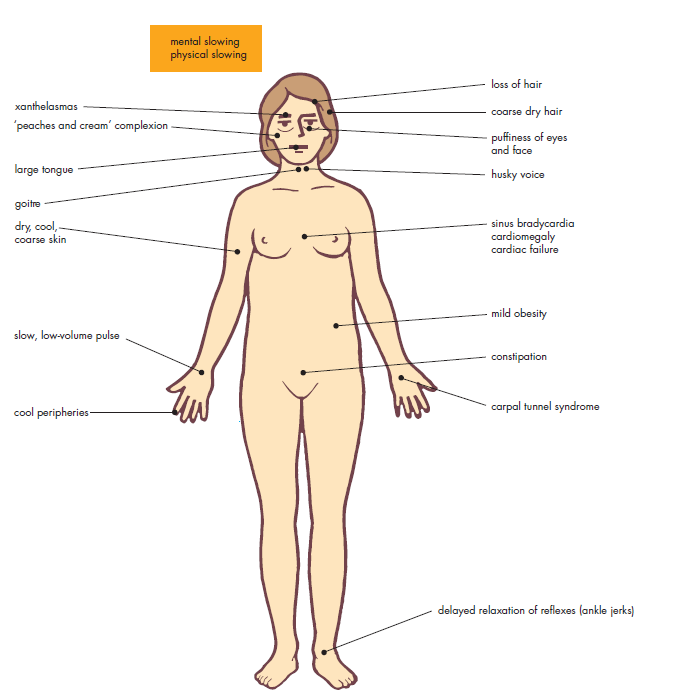
🧑⚕️ Clinical Features
- General: tiredness, lethargy, weight gain, cold intolerance.
- Neuropsychiatric: poor memory, depression, psychosis, ataxia, slow movements.
- GI: constipation.
- Reproductive: menorrhagia or oligomenorrhoea, infertility.
- Skin/hair: dry skin, thin brittle hair, hair loss, periorbital puffiness.
- Cardio: bradycardia, heart failure, pericardial effusion.
- Neuro exam: “hung-up” slow-relaxing reflexes, proximal myopathy.
- Severe: myxoedema coma (rare, emergency).
- Children: congenital hypothyroidism → growth retardation & cretinism if untreated.
🆚 Differential Diagnosis
- Hypopituitarism (low/normal TSH with low T4).
- Chronic fatigue syndrome.
- Depression (can mimic fatigue/low mood).
- Obstructive sleep apnoea.
- Other causes of weight gain and lethargy (e.g. Cushing’s, anaemia).
🔬 Investigations
- TFTs: high TSH, low T4 (primary); low/normal TSH with low T4 (secondary).
- FBC: normocytic or macrocytic anaemia (pernicious anaemia association).
- CXR: may show pleural/pericardial effusion.
- ECG: bradycardia, low QRS voltage.
- Thyroid antibodies: TPO antibodies positive in autoimmune thyroiditis.
- Ultrasound: if nodules/goitre present.
📊 Classification
- Overt hypothyroidism: TSH ↑ (>10 mU/L), T4 ↓ → treat.
- Subclinical hypothyroidism: TSH ↑, T4 normal. Treat if TSH >10, symptomatic, or TPO-Ab positive.
- Secondary hypothyroidism: T4 ↓ with inappropriately low/normal TSH → pituitary cause.
- Euthyroid: normal TSH & T4.
📉 ECG in Hypothyroidism
🧪 Treatment Algorithm
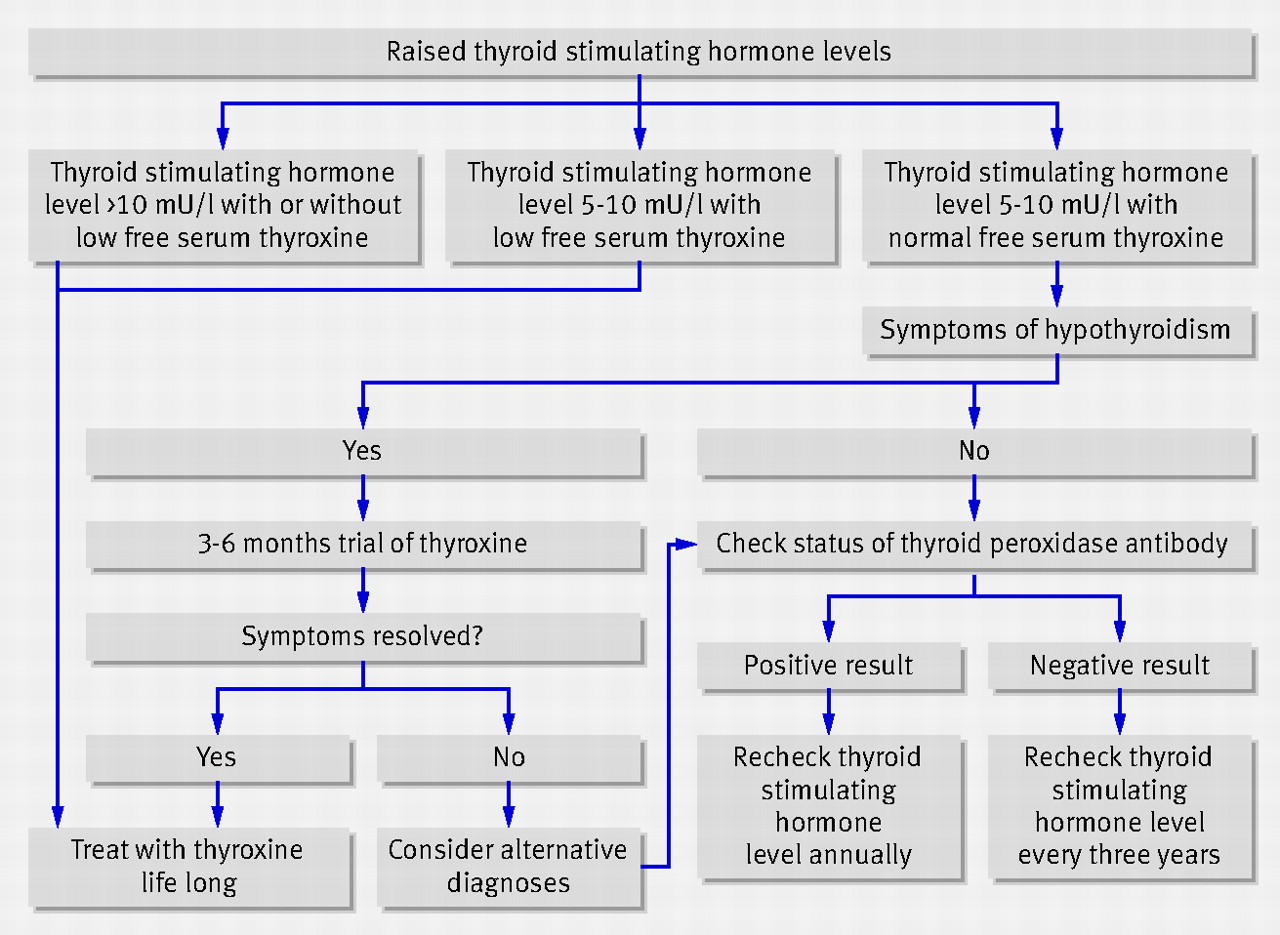
💊 Management
- Levothyroxine (T4): first-line, lifelong replacement in most patients.
- Dosing: Typical adult dose 100–150 mcg OD. Start lower (25–50 mcg) in elderly or those with ischaemic heart disease, then titrate every 6–8 weeks.
- T3 (liothyronine): only indicated in selected cases (e.g. myxoedema coma, rare poor responders to T4).
- Monitor: TSH (and T4 in secondary hypothyroidism). Target TSH in normal range.
- Pregnancy: higher levothyroxine requirements; check TFTs early each trimester.
- Myxoedema coma: ICU emergency - IV levothyroxine ± liothyronine, IV hydrocortisone, supportive care.
📌 OSCE / Exam Tips
- Classic vignette: young woman with fatigue, cold intolerance, dry skin, TSH ↑, T4 ↓.
- Differentiate subclinical vs overt hypothyroidism.
- In elderly/IHD → start levothyroxine low & slow.
- Myxoedema coma: hypothermia, bradycardia, drowsiness → emergency.
- Don’t forget associations: autoimmune thyroiditis + pernicious anaemia / T1DM.
📚 References
- Hypothyroidism: An Update – AAFP
- Kumar & Clark’s Clinical Medicine, 10th ed.
- NICE CKS: Hypothyroidism (2023).
🧾 Clinical Case Examples – Hypothyroidism
Case 1 – Classic Overt Hypothyroidism 👩🦰 A 32-year-old woman presents with 6 months of fatigue, weight gain, constipation, and feeling cold all the time. Exam: dry skin, periorbital puffiness, slow reflexes. Bloods: TSH 18 mU/L, T4 low, TPO antibodies positive. 👉 Diagnosis: Autoimmune hypothyroidism (Hashimoto’s). 👉 Management: Start levothyroxine 100 mcg daily, monitor TSH every 6–8 weeks. Lifelong therapy likely.
Case 2 – Elderly with IHD & Hypothyroidism ❤️ A 75-year-old man with ischaemic heart disease presents with lethargy and ankle swelling. Exam: bradycardia (HR 52), pitting oedema, cool peripheries. Bloods: TSH 12 mU/L, T4 low. 👉 Key point: Elderly patient with cardiac disease - risk of precipitating angina/arrhythmia if started on high-dose thyroxine. 👉 Management: Start low-dose levothyroxine (25 mcg OD), titrate slowly, close cardiac monitoring.
Case 3 – Myxoedema Coma 🚨 A 68-year-old woman with known untreated hypothyroidism is brought in drowsy, hypothermic (34°C), and bradycardic (HR 40). Exam: periorbital puffiness, hypotension, delayed reflexes. Bloods: very low T4, very high TSH, hyponatraemia. 👉 Diagnosis: Myxoedema coma - rare, life-threatening hypothyroidism. 👉 Management: ICU admission, IV levothyroxine ± liothyronine, IV hydrocortisone (until adrenal insufficiency excluded), active warming, fluid/electrolyte correction, treat precipitant (e.g. infection, MI).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
