| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Cushing syndrome
⚠️ Important: Hypokalaemia is more likely when the source of ACTH is malignant. 🧠 A normal pituitary MRI does not exclude Cushing’s disease – up to 50% (especially children) may have normal imaging. 👉 In such cases, inferior petrosal sinus sampling is crucial.
📖 About
- Cushing's Syndrome = chronic exposure to excessive cortisol.
- Disrupts hypothalamic–pituitary–adrenal (HPA) axis feedback 🔄.
- Loss of normal circadian cortisol rhythm 🌙☀️.
- Cushing’s Disease = pituitary adenoma secreting ACTH.
🧬 Aetiology
- 🌟 ACTH-dependent:
- 🧠 Pituitary adenoma (Cushing’s disease).
- 🫁 Ectopic ACTH from tumours (e.g. lung, pancreas).
- 🌟 ACTH-independent:
- 🟤 Adrenal adenomas/carcinomas.
- 💊 Exogenous glucocorticoids (most common overall cause).
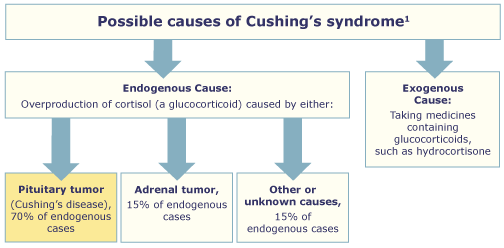
⚡ Causes
- 🧠 Pituitary Adenoma (Cushing’s Disease) (~70% endogenous)
- Microadenomas → ↑ACTH → bilateral adrenal hyperplasia.
- Key: not suppressed by low-dose dex, partially suppressed by high-dose; ↑ACTH & cortisol; responds to CRH.
- 🟤 Adrenal Tumours
- Autonomous cortisol secretion → suppressed ACTH.
- No suppression on low or high-dose dex.
- 🫁 Ectopic ACTH Production
- Sources: small cell lung carcinoma, bronchial carcinoid, pancreatic NET.
- ACTH high, no suppression on high-dose dex.
- Often severe hypokalaemia ⚠️ due to mineralocorticoid activity.
- 💊 Iatrogenic – long-term glucocorticoid therapy (asthma, RA, PMR, UC, post-transplant).
- 🎭 Pseudo-Cushing’s – alcohol excess, severe obesity, depression (reversible).
- 🤰 Pregnancy – ↑ cortisol-binding globulin → raised total cortisol (rarely true Cushing’s).
👀 Clinical Features
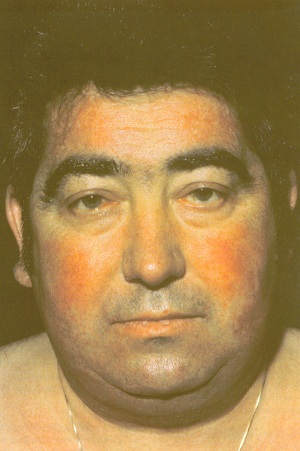
- Appearance 🌙:
- Centripetal obesity.
- Moon face, facial plethora, acne.
- Dorsocervical fat pad (“buffalo hump”).
- Muscle wasting → thin extremities.
- Purple striae (abdomen, thighs, breasts).
- Skin 🩹:
- Thin fragile skin, easy bruising.
- Slow wound healing.
- Hirsutism in women.
- Hyperpigmentation (if ACTH-driven).
- MSK 💪:
- Proximal myopathy (difficulty standing/climbing stairs).
- Osteoporosis → fractures.
- Avascular necrosis of femoral head.
- Metabolic 🧪:
- Glucose intolerance / diabetes.
- Hyperlipidaemia.
- Hypertension.
- Hypokalaemia & metabolic alkalosis.
- Neuropsychiatric 🧠:
- Mood swings, depression, psychosis.
- Cognitive impairment.
- Reproductive ❤️:
- Women: amenorrhoea, infertility.
- Men: ↓ libido, impotence.
- Growth 📏:
- Stunted growth in children.
- Immune 🛡️:
- Infections, reactivation of TB.
- Poor wound healing.


🧪 Diagnostic Tests
🌙 Overnight Dexamethasone Suppression (screen)
- 1 mg dex at midnight → cortisol at 08:00.
- Normal < 50 nmol/L;> 50 → suspect Cushing’s.
- ⚠️ False positives: depression, obesity, alcohol, phenytoin.
🧪 24h Urinary Free Cortisol (screen)
- Normal < 280 nmol/24h; elevated = abnormal.
💉 Low-Dose 48h Dex Test (confirm)
- 0.5 mg dex 6-hourly × 48h (total 4 mg).
- Cortisol undetectable = excludes; detectable = Cushing’s confirmed.
📊 High-Dose 48h Dex Test (localise)
- 2 mg dex 6-hourly × 48h (total 16 mg).
- Pituitary: >50% suppression.
- Ectopic/adrenal: no suppression.
🧬 Plasma ACTH
- ⬇️ Undetectable → adrenal tumour.
- ⬆️ High → pituitary vs ectopic.
- CRH test: rise = pituitary; no rise = ectopic.
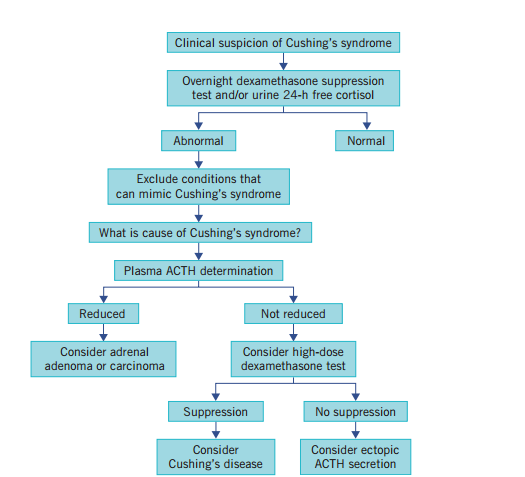
📚 Exam Tip: Think stepwise → Overnight (screen) → Low-dose (confirm) → High-dose/ACTH (localise). Pituitary = suppressible, ectopic/adrenal = resistant.
🖼️ Imaging
- 🧠 Pituitary MRI (but 50% normal!) → may need inferior petrosal sinus sampling.
- 🟤 Adrenal CT/MRI → adenoma or carcinoma.
- 🫁 Chest/abdomen CT → ectopic ACTH tumours.
- 📡 Octreotide scans for ectopic localisation.
💊 Management
- 🧠 Pituitary adenoma: transsphenoidal resection; radiotherapy if unsuccessful; pasireotide or ketoconazole if refractory.
- 🟤 Adrenal tumours: adrenalectomy ± mitotane if carcinoma.
- 🫁 Ectopic ACTH: treat primary tumour if resectable; otherwise medical control of cortisol.
- 💊 Iatrogenic: gradual steroid taper, switch to steroid-sparing alternatives.
🧪 Medical Therapy (for inoperable / pre-surgery)
- Metyrapone (11β-hydroxylase inhibitor).
- Ketoconazole (blocks steroidogenesis).
- Aminoglutethimide (cholesterol → pregnenolone block).
- Mitotane (adrenolytic, carcinomas).
- Etomidate (IV emergency use).
📌 Key Points
- Early recognition prevents morbidity & mortality.
- Diagnosis = stepwise biochemical + imaging + sometimes petrosal sampling.
- Management is cause-directed (surgery first-line where possible).
- 🏥 Long-term follow-up essential: recurrence, metabolic complications, bone health, psychological support.
Cases - Cushing’s Syndrome
- Case 1 - Iatrogenic steroid use 💊: A 55-year-old woman with rheumatoid arthritis on long-term prednisolone presents with weight gain, easy bruising, proximal muscle weakness, and thin skin. Exam: moon facies, buffalo hump, purple abdominal striae. Diagnosis: exogenous Cushing’s syndrome due to chronic glucocorticoid therapy. Managed by gradual tapering of steroids and use of steroid-sparing agents.
- Case 2 - Pituitary-dependent (Cushing’s disease) 🧠: A 36-year-old woman presents with irregular menses, hirsutism, and worsening acne. Exam: central obesity, hypertension, and skin thinning. Bloods: elevated cortisol not suppressed by low-dose dexamethasone, but suppressed with high-dose dexamethasone. MRI: pituitary microadenoma. Diagnosis: Cushing’s disease (ACTH-secreting pituitary adenoma). Managed with trans-sphenoidal pituitary surgery.
- Case 3 - Adrenal tumour ⚠️: A 42-year-old man presents with new-onset diabetes, hypertension, and muscle wasting. No exogenous steroid use. Bloods: raised cortisol with suppressed ACTH. CT abdomen: adrenal mass. Diagnosis: ACTH-independent Cushing’s syndrome due to adrenal adenoma. Managed with adrenalectomy.
Teaching Point 🩺: Cushing’s syndrome = chronic glucocorticoid excess. Common causes: exogenous steroids, pituitary adenoma (Cushing’s disease), adrenal adenoma/carcinoma, ectopic ACTH (e.g. small-cell lung cancer). Clinical clues: central obesity, moon facies, striae, proximal weakness, hypertension, diabetes, mood changes. Diagnosis: screen with 24h urinary cortisol, overnight dexamethasone suppression, late-night salivary cortisol. Management: treat underlying cause (taper steroids, pituitary surgery, adrenalectomy).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
