| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
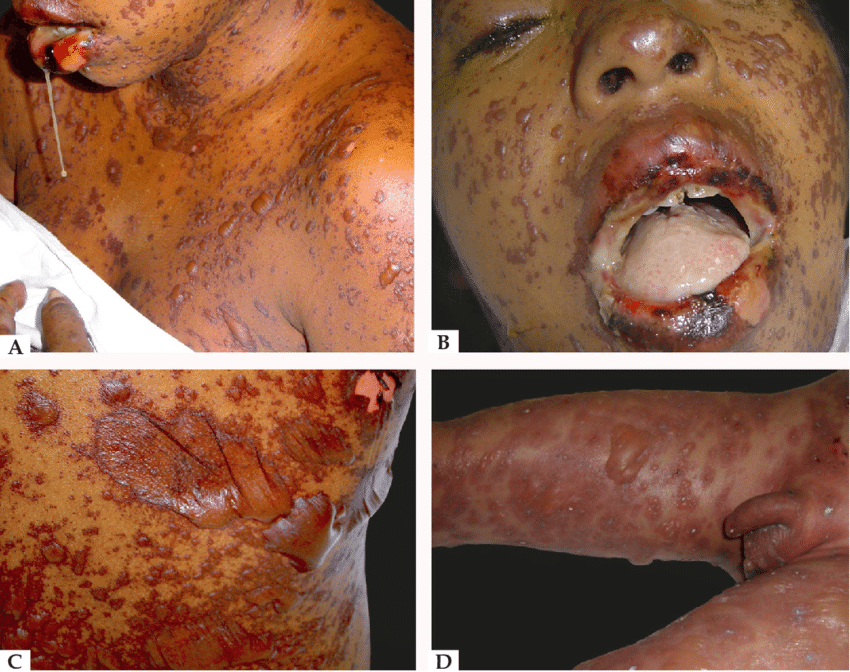
Toxic Epidermal Necrolysis (TEN) and Stevens-Johnson syndrome
Related Subjects: |Cellulitis |Pyoderma gangrenosum |Pemphigus Vulgaris |Toxic Epidermal Necrolysis |Stevens-Johnson Syndrome |Necrotising fasciitis |Gas Gangrene (Clostridium perfringens) |Purpura Fulminans |Severe burns |Anatomy of Skin |Skin Pathology and Lesions |Skin, Soft Tissue & Bone Infections
⚠️ Toxic Epidermal Necrolysis (TEN) is a rare, life-threatening dermatological emergency. It lies at the most severe end of the SJS–TEN spectrum, caused by an immune-mediated reaction against keratinocyte adhesion molecules. This leads to widespread skin necrosis, epidermal detachment, and mucosal involvement.
📌 About
- Part of the SJS–TEN spectrum (SJS: <10% BSA, TEN: >30% BSA, overlap: 10–30%).
- Marked by extensive epidermal sloughing, like a severe burn injury.
- High risk of sepsis, fluid loss, multi-organ failure, and death.
🧾 Aetiology
- 💊 Drug-induced (most common) – sulphonamides, cephalosporins, anticonvulsants (carbamazepine, phenytoin, lamotrigine).
- 🧬 Idiopathic cases → worse prognosis, esp. in haematological malignancy (e.g. leukaemia, lymphoma).
- 🦠 Higher risk in viral infections (notably HIV).
- 🧪 Genetic risk: slow acetylator phenotype predisposes.
💊 Common Culprit Drugs (≈50% cases)
- Allopurinol
- Carbamazepine / Lamotrigine
- Nevirapine
- Oxicam NSAIDs
- Phenobarbital
- Phenytoin
- Sulphonamides (e.g. sulfamethoxazole)
- Sulfasalazine
🤒 Clinical Features
- Prodrome: fever, malaise, myalgia (flu-like).
- Painful, rapidly spreading erythema → confluent blistering.
- Mucous membrane involvement: oral, ocular, genital.
- Widespread epidermal detachment → erosions, fluid loss, risk of infection.
- Sepsis & multi-organ failure are leading causes of death.
🔍 Differential Diagnosis
- Staphylococcal scalded skin syndrome (SSSS) – mucosa spared.
- Toxic shock syndrome.
- DRESS (Drug Reaction with Eosinophilia & Systemic Symptoms).
- Severe phototoxic reactions.
📊 SCORTEN Severity Score
- Age >40 years → +1
- HR >120 bpm → +1
- Underlying malignancy → +1
- BSA detachment >10% → +1
- Urea >10 mmol/L → +1
- HCO₃⁻ <20 mmol/L → +1
- Glucose >14 mmol/L → +1
💀 Mortality by SCORTEN
- 0–1 → ~3%
- 2 → ~12%
- 3 → ~35%
- 4 → ~58%
- ≥5 → ~90%
🧪 Investigations
- Bloods: FBC, U&E, LFTs, CRP, coagulation profile.
- Skin biopsy → differentiates TEN from SSSS.
- Blood & urine cultures; CXR if febrile.
🏥 Management
- 🔺 Admit ICU / burns unit if SCORTEN ≥2 or BSA >10% involved.
- ⚡ Supportive care: fluid/electrolyte balance, nutrition, thermoregulation.
- 🔥 Fire risk: paraffin-based emollients are flammable → CO₂ extinguisher + fire blanket at bedside.
- 🫁 Airway: anticipate obstruction if mucosa involved; use non-adhesive fixation.
- 💨 Breathing: monitor for ARDS; use lung-protective ventilation if intubated.
- 💉 Circulation: invasive access via unaffected skin; fluids, albumin, vasopressors as required.
- 🩸 Transfusion: maintain Hb >70 g/L (or >90 in CVD); monitor coagulopathy.
- 💊 Analgesia: opioids ± sedation for dressing changes; early pain team input.
- 🌡️ Exposure: prevent hypothermia (room 25–28°C; warmed IV fluids).
- 🥗 Nutrition: NG feeding early; consider parenteral if needed; beware refeeding syndrome.
- 🦠 Infection: barrier nursing; treat only proven infection (early Staph → later Gram-negatives like Pseudomonas).
- 👁️ Ophthalmology: daily review; lubricants ± topical antibiotics.
📚 References
🖼️ Images


Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
