| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Synchronised DC Cardioversion
Related Subjects: | AF - General | AF and Anticoagulation | AF and Rate Control | AF and Rhythm Control and Cardioversion | AF ECG | DC cardioversion
⚠️ Caution: haemodynamic compromise purely from AF is uncommon. More often the driver is the underlying illness (e.g. sepsis/pneumonia, ACS, PE, decompensated HF, electrolyte/metabolic derangement). Treat the precipitant first; if uncertain that AF is the primary problem, get senior/cardiology input early.
ℹ️ About
- ⚡ Any unstable tachyarrhythmia is an indication for synchronised DC cardioversion (DCCV).
- 🚑 If AF + life-threatening features → DCCV now (don’t delay for anticoagulation).
- 🫀 Synchronisation times the shock to the R wave to avoid “R-on-T” (VF risk).
- 🧠 Think “cause first”: in sinus tachycardia, don’t try to normalise HR with shocks/antiarrhythmics — treat the driver.
Life-threatening features (treat as UNSTABLE)
- 🫨 Shock
- 😵 Syncope with severe/ongoing hypotension
- 🫀 Myocardial ischaemia (ongoing chest pain/ECG ischaemia)
- 🌊 Severe heart failure with pulmonary oedema or shock
- 🧯 Immediately post-ROSC with recurrent/ongoing tachyarrhythmia
Emergency DCCV – Indications
- ⚡ Any tachyarrhythmia with life-threatening features.
- 💥 Fast AF with hypotension/ischaemia/pulmonary oedema (often HR >150/min) despite immediate supportive measures.
- 🧬 AF with pre-excitation (WPW physiology) and rapid ventricular response → DCCV or procainamide (avoid AV node blockers).
- 📈 VT with a pulse causing compromise → synchronised cardioversion.
Elective DCCV – Indications
- 🎯 AF as part of a rhythm-control strategy (symptoms, HF, first episode/early AF, patient preference).
- 🪽 Atrial flutter (often highly responsive to lower-energy DCCV).
- 🩸 Ensure an anticoagulation strategy (see below) or TOE-guided early cardioversion.
When Elective DCCV is Unlikely to Succeed / Consider Deferring
- 🕰️ Long-standing persistent AF (>12 months) or markedly enlarged LA (e.g. >5.0 cm / high LA volume).
- 🧯 Reversible trigger not corrected (infection, thyrotoxicosis, alcohol binge, pericarditis, severe valve disease).
- 🔁 Prior failed cardioversion despite optimisation/antiarrhythmics.
- 🩸 Not adequately anticoagulated (unless TOE strategy planned and no thrombus).
Anticoagulation Around Cardioversion (UK + practical)
- Scheduled/elective: if AF duration is >48 h or unknown (common UK threshold), give therapeutic OAC for ≥3 weeks before and ≥4 weeks after DCCV (DOAC or warfarin INR 2–3). Alternative: TOE-guided early cardioversion if no LA/LAA thrombus.
- Emergency/unstable: proceed with DCCV for instability, then start therapeutic OAC as soon as feasible and continue for ≥4 weeks (and long-term based on stroke risk).
- After 4 weeks: continue long-term OAC according to CHA2DS2-VASc / local policy, not “because they’re in sinus rhythm”.
- Pragmatic safety note: some contemporary guidance uses a more cautious >24 h threshold for “needs TOE or 3 weeks OAC before cardioversion” (especially if onset uncertain). If your history is shaky, treat it as unknown duration.
Procedure – Key Steps (DCCV)
- 👥 Senior review; call cardiology/anaesthetics if time allows; obtain consent where possible.
- 🫁 Sedation/anaesthesia with full monitoring (ECG, BP, SpO2), IV access, airway kit ready.
- 🩹 Pad position: antero-posterior (or antero-lateral). Shave hair if needed; ensure firm pressure and good gel contact.
- 🔁 Select SYNCHRONISED mode for AF/SVT/VT with pulse; confirm sync markers before each shock.
- 🔥 Oxygen safety: keep O2 source away from pad “spark zone”.
Energy (biphasic) – Practical starting points
- Narrow regular (SVT / typical flutter): 70–120 J (escalate if needed)
- Narrow irregular (AF): 120–150 J (then escalate to 200 J or per device)
- Wide regular (VT with pulse): start ~120–150 J (escalate)
- Wide irregular (polymorphic VT): DEFIBRILLATE (unsynchronised)
If DCCV fails (typical escalation)
- 🔁 Up to 3 shocks with escalation and optimised pad contact/position.
- 💊 Consider amiodarone 300 mg IV (then infusion e.g. 900 mg over 24 h) and repeat DCCV.
- 🧪 Re-check and correct K/Mg, acidosis, hypoxia, ongoing ischaemia, sepsis, PE etc.
Complications (risk–benefit)
- 🧠 Stroke/systemic embolism (risk minimised by correct peri-DCCV anticoagulation).
- 🐢 Post-shock bradycardia/pauses (usually transient; have atropine/pacing capability available).
- 🔥 Skin burns / myalgia at pad sites.
- 😴 Sedation-related events (hypoventilation, aspiration) — hence airway readiness.
Investigations (don’t delay emergency DCCV)
- 📈 12-lead ECG + continuous monitoring.
- 🧪 FBC, U&E, Mg2+, LFTs, glucose; TFTs if new AF or unexplained.
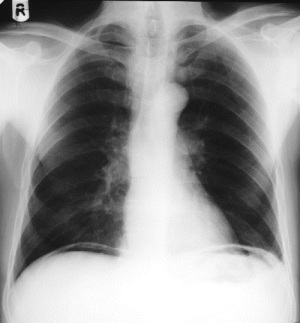
- 🫀 Troponin if ACS suspected; CRP/cultures/CXR if infection suspected.
- 🫁 Consider D-dimer/CTPA if PE suspected and clinically appropriate.
- 🧠 TOE if early cardioversion planned and not pre-anticoagulated (esp. duration >24–48 h or uncertain).
Images

References
- Resuscitation Council UK. Adult tachyarrhythmia algorithm (latest version).
- NICE NG196: Atrial fibrillation: diagnosis and management.
- ESC/EACTS AF guideline (latest).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
