| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Haemoptysis
Related Subjects: | Lung Cancer
🫁 Introduction
Haemoptysis = coughing up blood originating from the lower respiratory tract. ⚠️ Massive haemoptysis is a medical emergency → mortality is usually due to asphyxiation rather than blood loss. 💡 As little as 250 mL can fill the bronchial tree and obstruct the airway. 🎯 Always confirm the source (lung vs nasopharynx vs GI tract).
📊 About
- Common causes: TB, bronchiectasis, aspergilloma, lung cancer.
- Lungs have dual blood supply: pulmonary + bronchial arteries.
- 👉 Most haemoptysis originates from the bronchial arterial system (systemic pressure → brisk bleeding).
- Pulmonary circulation can shunt blood away from hypoxic zones.
🦠 Causes
- 🎗️ Malignancy: Bronchogenic carcinoma, metastases (esp. in smokers >40).
- 🦠 Infective: Pneumonia, lung abscess, TB (upper lobe lesions in young).
- 🍄 Aspergilloma: Cavitary disease → classically recurrent haemoptysis.
- 🌪️ Bronchiectasis: Purulent sputum, recurrent infection, CF common.
- 🚨 Trauma: Biopsy, bronchoscopy, penetrating injury.
- 🧬 Vasculitis: GPA (c-ANCA), Goodpasture’s (anti-GBM).
- 🫀 Vascular: PE with infarction, AVMs.
- 💉 Bleeding disorders: Thrombocytopenia, anticoagulation (warfarin, DOACs).
- ❤️ Cardiac: Mitral stenosis → pulmonary venous hypertension.
- 🌀 Other: Autoimmune disease, factitious haemoptysis.
🧑⚕️ Clinical Features
- History: smoking 🚬, TB exposure, weight loss ⚖️, bleeding disorders.
- Massive haemoptysis = >600 mL/24h or rapid bleeding with airway threat.
- Exam: clubbing, cachexia, chest crepitations, signs of chronic lung disease.
- Always distinguish from: – Epistaxis (nasopharyngeal blood trickling) 👃 – Haematemesis (vomiting blood from GI tract) 🍷
🧪 Investigations
- 🩸 Bloods: FBC, U&E, clotting, ABG.
- 🩻 CXR: May show cavitation, mass, consolidation, bronchiectasis.
- 🖥️ CT Angiography: Gold standard for source localisation if stable.
- 👁️ Bronchoscopy: Rigid/flexible to visualise + tamponade bleeding site.
- 🧬 Autoimmune tests: c-ANCA, anti-GBM.
🚨 Management of Massive Haemoptysis
- ABC first! Senior help immediately (respiratory, IR, cardiothoracics).
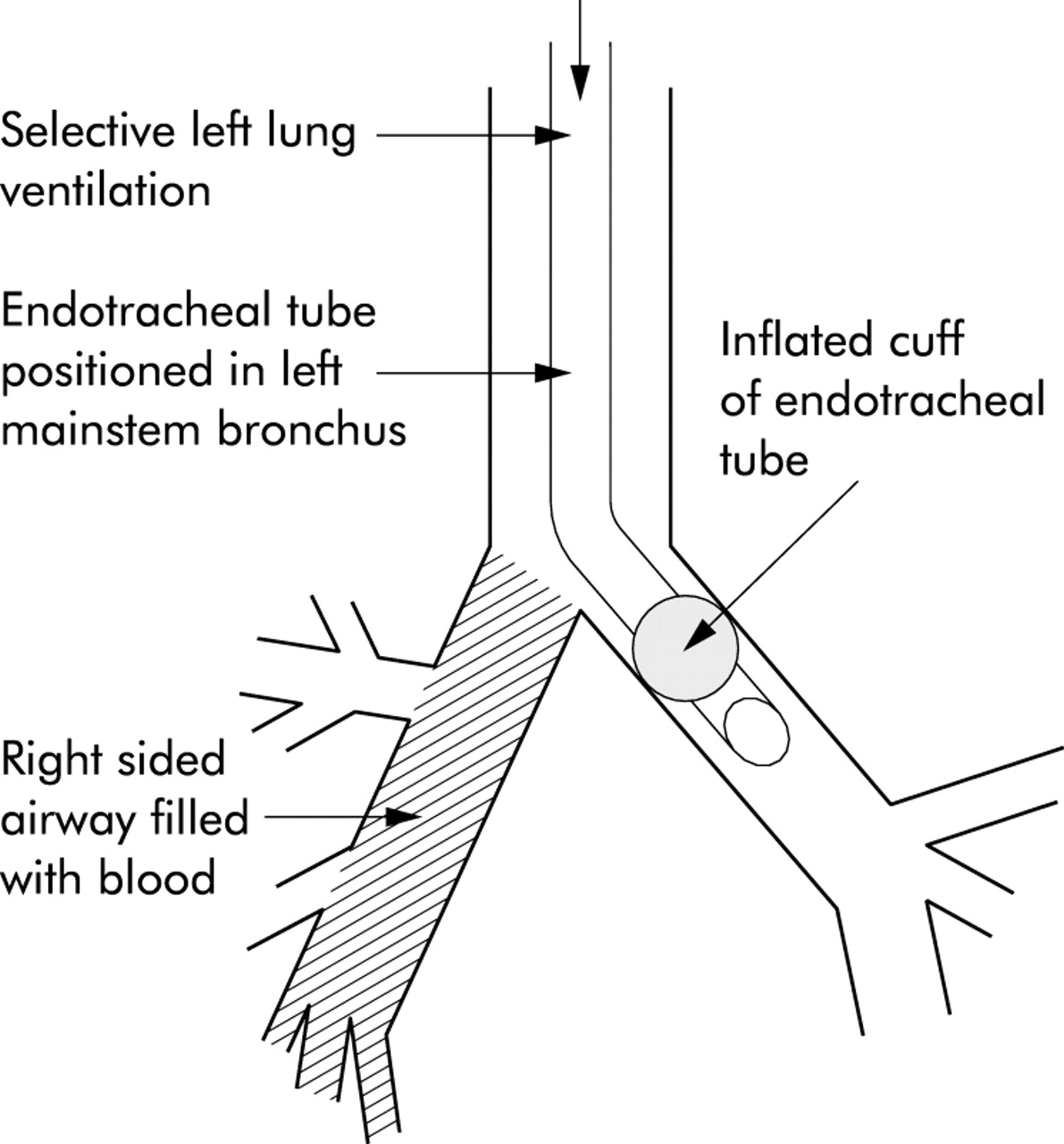
- 🫁 Position: Lie on side of bleeding lung → protect good lung.
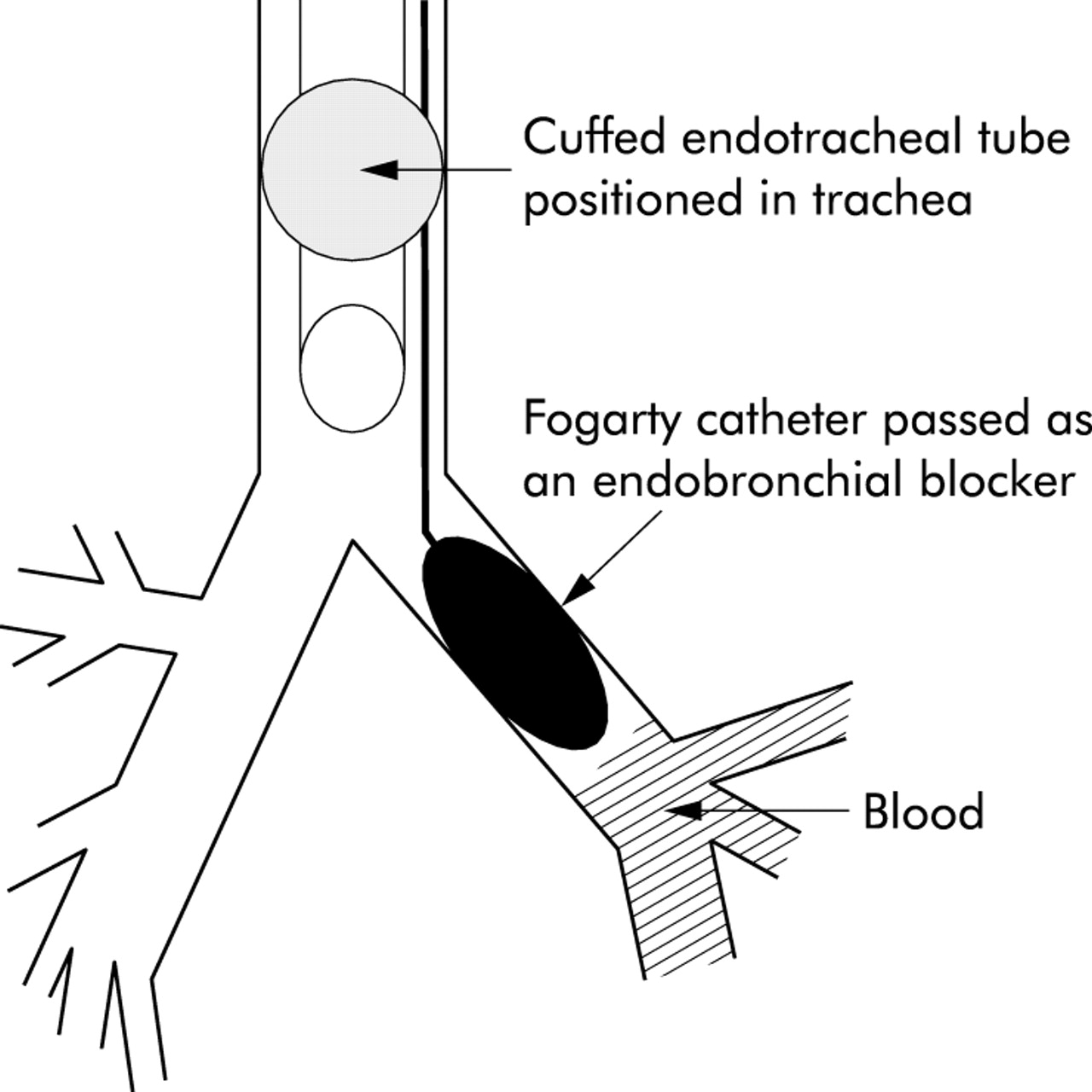
- 💨 Oxygen: High-flow. Intubation if decompensating (selective main bronchus intubation or double-lumen tube).
- 💉 IV Access: Wide-bore cannulae; crossmatch.
- 💊 Drugs: – Nebulised adrenaline (epinephrine) 5–10 mL of 1:10,000. – Nebulised tranexamic acid (e.g. 500 mg in 5 mL). – IV tranexamic acid (1 g IV over 10 min, then infusion if needed).
- 🖥️ Imaging: Urgent portable CXR; CT angiography if stable.
- 🔧 Bronchoscopy: Endobronchial blocker, suction, topical haemostatics.
- 🩻 Interventional Radiology: Bronchial artery embolisation (BAE) = first-line definitive therapy.
- 🔪 Surgery: Lobectomy/pneumonectomy if localised + fit for surgery.
- 🤲 Palliation: In terminal cancer → symptom control (morphine, midazolam, palliative sedation).
📌 Clinical Pearls
- Death in massive haemoptysis = airway obstruction, not blood loss.
- First priority = protect unaffected lung and maintain oxygenation.
- Tranexamic acid is increasingly used (nebulised or IV).
- BAE is highly effective but recurrence is common → monitor long term.
- Always rule out lung cancer in smokers >40 with unexplained haemoptysis.
📚 References
- British Thoracic Society (BTS) Guidelines – Management of Haemoptysis
- BMJ Best Practice: Haemoptysis
- Oxford Handbook of Clinical Medicine
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
