Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Infective Endocarditis
🩺 The presence of an Endocarditis Team is crucial in IE. This multidisciplinary approach has been shown to significantly reduce 1-year mortality. ⚠️ Do not start antibiotics before taking at least 3 blood cultures over 12+ hrs, using strict aseptic technique.
📖 About
- Infective Endocarditis (IE) = infection of the endocardium and heart valves, usually bacterial.
- Vegetations consist of organisms + fibrin + platelets, may embolise.
- Causes valve destruction, regurgitation, abscesses, and embolic/immune complications.
🧬 Aetiology & Pathophysiology
- Infection of native or prosthetic valves, congenital defects (VSD, bicuspid aortic valve).
- Often seeded by bacteraemia in patients with prior endothelial damage.
- Immune complex deposition → vasculitis, glomerulonephritis, skin signs.
- Emboli may affect brain 🧠, spleen, kidneys, or lungs.
📊 Epidemiology
- Commoner in men
- Increasingly older patients
- IV drug use → right-sided IE (tricuspid valve)
- Underlying rheumatic or congenital heart disease
🦠 Common Organisms
| Organism | Description | Common Situations |
|---|---|---|
| Staphylococcus aureus | Aggressive, acute IE | IVDU, healthcare-associated |
| Streptococcus viridans | Subacute, oral flora | Post-dental procedures |
| Enterococcus spp. | Older adults, subacute | GU or GI procedures |
| Staphylococcus epidermidis | Low-grade, prosthetic valves | PVE esp. <1 yr post-surgery |
| HACEK group | Fastidious GN bacteria | Culture-negative IE |
| Fungal IE | Large vegetations, high mortality | Immunocompromised, IVDU |
⚠️ High Risk Groups
- Prosthetic valve patients (including TAVI)
- Previous IE
- Uncorrected cyanotic congenital heart disease, or within 6 months post-repair
🩺 Clinical Features
- Constitutional: malaise, fever, sweats, weight loss
- Cardiac: new murmur, AF, HF, conduction block
- Embolic: stroke, splenic infarct, lung abscess
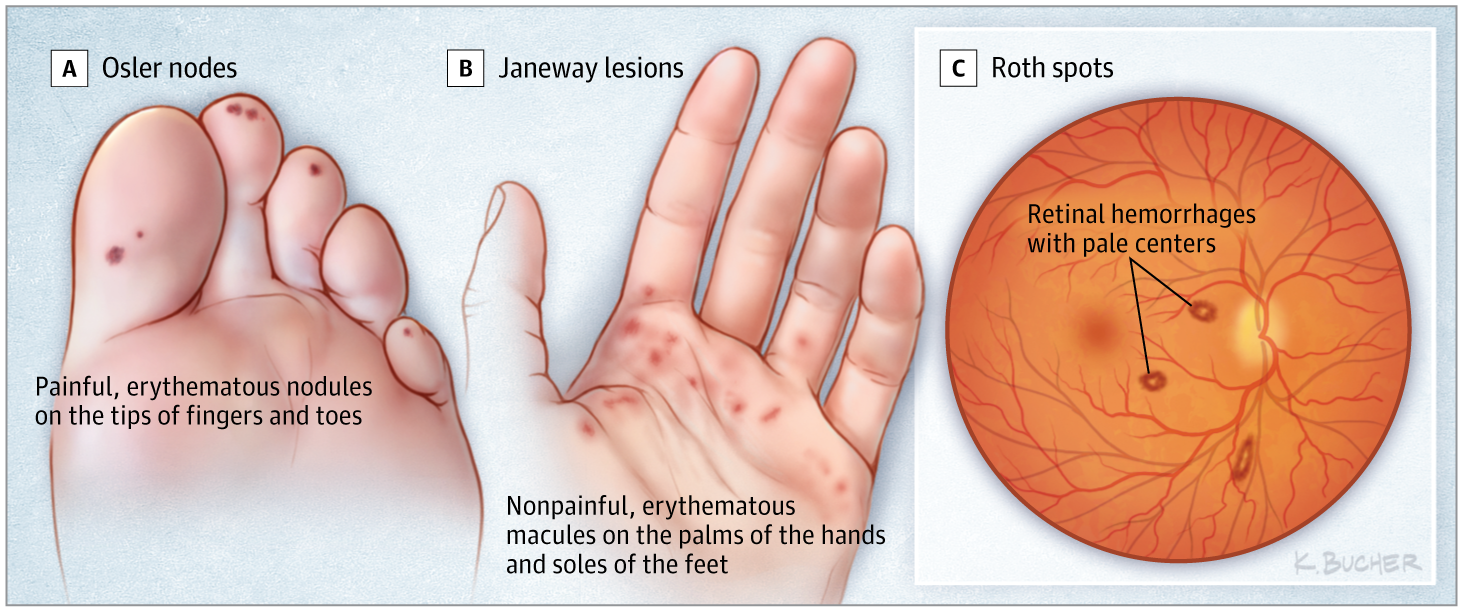
- Peripheral stigmata: Roth spots 👁, splinter haemorrhages, Osler nodes (tender), Janeway lesions (painless)
- Right-sided IE → septic lung emboli, cavitating pneumonia
Clinical signs or Stigmata of Endocarditis
Vegetations
Roth's spots
Vegetations
🔎 Diagnosis
- Blood cultures: 3 sets before antibiotics
- Echocardiography: TEE > TTE for vegetations, abscess, prosthetic dehiscence
- Duke criteria: Major + minor clinical/micro/echo findings
🫀 The Modified Duke Criteria help diagnose infective endocarditis (IE) by combining 🔬 microbiology, 🖥️ echo, and clinical features. They classify cases as definite, possible, or rejected, reducing both missed cases and overtreatment.
🧪 Pathological Criteria
- Positive histology/microbiology from valve, vegetation, abscess, or embolic material
🔑 Major Criteria
- Microbiology: Typical organisms in ≥2 cultures, persistent bacteremia, or positive serology/PCR (e.g. Coxiella).
- Echo: Vegetation, abscess, new prosthetic valve dehiscence, or new regurgitation.
⚖️ Minor Criteria
- Predisposing lesion or IVDU
- Fever >38°C 🌡️
- Vascular phenomena (emboli, Janeway lesions, mycotic aneurysm)
- Immunological phenomena (Osler’s nodes, Roth’s spots, GN, RF)
- Non-typical microbiology
- ↑ ESR/CRP
📊 Quick Reference Table
| Category | Criteria |
|---|---|
| Pathological | Histology/microbiology from valve/vegetation/abscess/embolus |
| Major | Typical organisms (≥2 cultures), persistent bacteremia, positive serology/PCR, echo evidence (vegetation, abscess, new regurgitation, prosthetic dehiscence) |
| Minor | Predisposition, fever >38°C, vascular signs, immunological signs, non-typical culture, ↑ ESR/CRP |
| Diagnosis |
|
📚 Exam Tips:
👉 Always take 3x blood cultures before antibiotics.
👉 TOE > TTE for vegetations & prosthetic valves.
👉 🔑 Janeway = painless, Osler’s = painful.
👉 Definite IE = 2 major or 1 major + 2 minor.
🧪 Investigations
- Bloods: normocytic anaemia, raised ESR/CRP
- Urine: microscopic haematuria (GN)
- ECG: arrhythmia, AV block (aortic root abscess)
- CXR: pulmonary oedema, septic emboli
- CT/MRI brain: embolic infarcts (often haemorrhagic if anticoagulated)
💊 Medical Management
- Source control: treat dental/skin sepsis
- Culture-guided IV antibiotics (see table below)
- Duration: 4–6 weeks (≥6 weeks if prosthetic valve)
- Prosthetic valve IE: triple therapy (vancomycin + gentamicin + rifampicin)
- Close liaison with Endocarditis MDT
📊 Endocarditis – Antibiotic Management Summary
| Causative Group | Recommended Treatment | Duration | Notes |
|---|---|---|---|
| Streptococcus (penicillin-sensitive) | Benzylpenicillin IV + Gentamicin (first 2 weeks) | 4 weeks | Native valve; good prognosis |
| Enterococcus | Amoxicillin IV + Gentamicin
(If penicillin allergy → Vancomycin + Gentamicin) |
4–6 weeks | High-level gentamicin resistance increasingly common |
| MSSA | Flucloxacillin IV | 4–6 weeks | ± Gentamicin first 2 weeks; avoid in renal impairment |
| MRSA / Penicillin Allergy | Vancomycin (level-adjusted) + Rifampicin ± Gentamicin | 6 weeks | Close drug-level monitoring essential |
| Prosthetic Valve Endocarditis | Vancomycin + Rifampicin + Gentamicin | ≥ 6 weeks | High mortality – always involve cardiothoracic surgery early |
| HACEK group | Ceftriaxone IV | 4 wks (native)
6 wks (prosthetic) |
Slow-growing Gram negatives |
| Fungal | Amphotericin B or Echinocandin | Prolonged | Surgery almost always required |
💡 Exam Tip: Always take 3 sets of blood cultures before starting antibiotics (unless the patient is critically unwell). Surgical referral is urgent if there is heart failure, peri-valvular abscess, uncontrolled sepsis, or large vegetations.
🪡 Surgical Management
- Indications: refractory infection, emboli despite therapy, HF from valve destruction, abscess
- Procedures: valve replacement (mechanical, bioprosthetic, homograft), repair where feasible, abscess drainage, device removal
- Timing: urgent if severe HF/emboli; elective if stabilised after antibiotics
📚 Reference
Categories
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology