| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
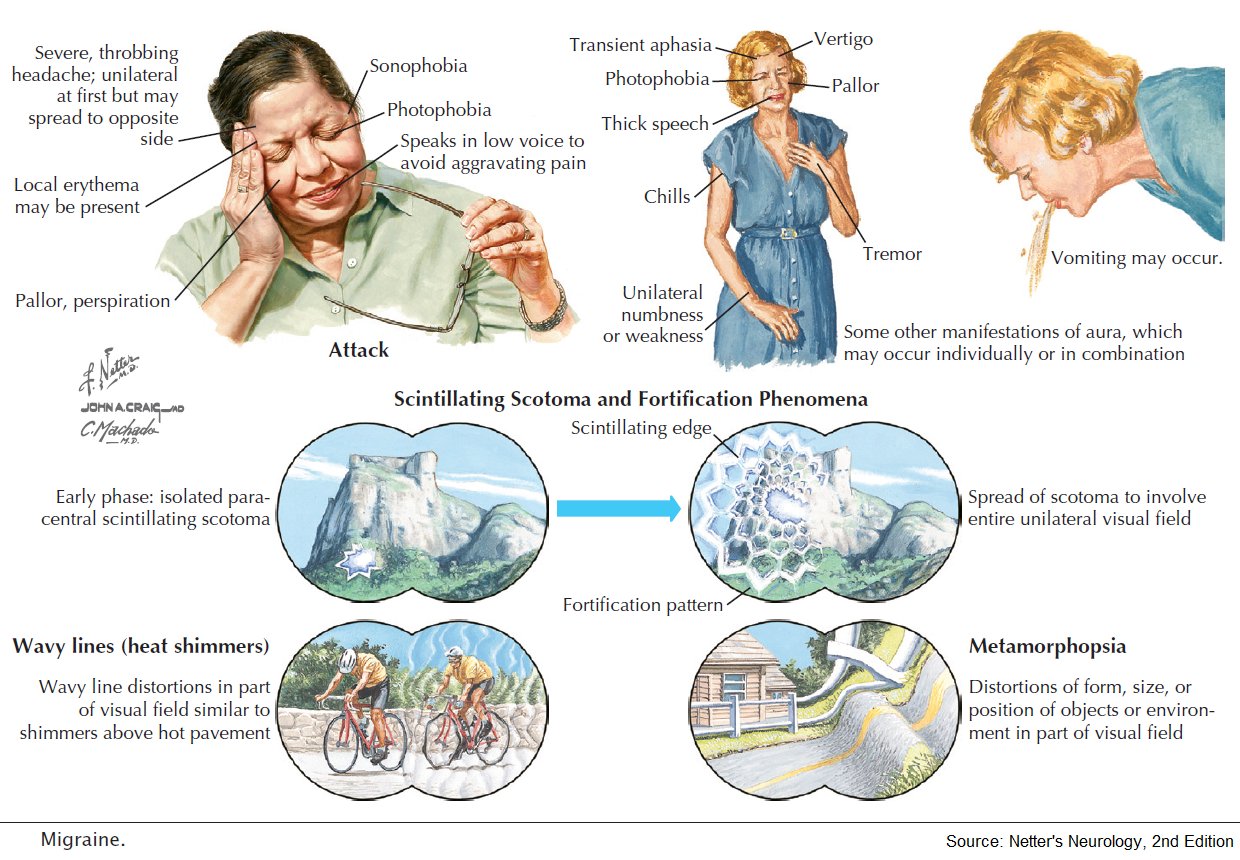
Migraine
Related Subjects:Migraine |Basilar Migraine |Cluster Headaches |Sumatriptan |Tension Headache |Analgesic Overuse Headache |Headaches in General |CADASIL
🧠 Migraine is a chronic, episodic neurological disorder causing recurrent headaches with associated features such as nausea 🤢, vomiting, photophobia 😎, and phonophobia 🔊. It affects ~1 in 10 people, more common in women (14%) than men (4%). Onset is often in childhood or young adulthood.
ℹ️ About
- ⏳ Two main types:
- Migraine without aura (common migraine)
- Migraine with aura (classical migraine)
- 🔬 Classification follows the International Classification of Headache Disorders (ICHD-2).
- 👩⚕️ Migraine is more disabling from its cognitive and sensory symptoms than from headache pain alone.
Diagnostic Criteria – Migraine without Aura
- 🔄 At least 5 attacks lasting 4–72 hours.
- ➡️ Headache has ≥2 of:
- Unilateral location 🎯
- Pulsating quality 💓
- Moderate/severe pain intensity
- Aggravated by routine activity 🏃
- During headache, ≥1 of:
- Nausea and/or vomiting 🤮
- Photophobia 😵💫 and phonophobia 📢
Diagnostic Criteria – Migraine with Aura
- ⚡ At least 2 attacks with reversible neurological symptoms:
- Visual (flickering lights ✨, scotoma 👁️)
- Sensory (pins and needles 🤲, numbness)
- Speech disturbance 🗣️
- Symptoms evolve over ≥5 minutes, last 5–60 min ⏱️, and are followed by headache within 1 hour.
🧬 Aetiology
- 🧬 Involves serotonin and CGRP dysregulation.
- 🌊 Cortical Spreading Depression (CSD): self-propagating depolarization wave → aura.
- 💓 Possible association with right-to-left shunts (e.g., PFO).
Associations
- 🧠 CADASIL (hereditary stroke disorder)
- 💔 PFO (patent foramen ovale) – controversial role in migraine with aura
- ⚡ Mitochondrial disease (MELAS)
- 🩸 Antiphospholipid antibodies & stroke syndromes
🩺 Clinical Features
- ⏱️ Duration: 4–72 hours
- 🧩 Aura in ~30% (visual, sensory, speech)
- 🤢 GI features: nausea, vomiting, diarrhoea, colic
- 🌓 Unilateral headache in ~60%, bilateral in the rest
- 🔥 Triggers: stress, let-down after stress (weekends), alcohol 🍷, cheese 🧀, lack of sleep, dehydration, exercise
🔎 Investigations
- 🧪 Usually clinical diagnosis – no tests needed in typical cases.
- ⚠️ Exclude SAH with CT ± LP if acute/atypical presentation.
- 📉 ESR for suspected temporal arteritis.
- 🫀 Bubble echo if aura + suspicion of PFO.
Migraine Variants
- 🌀 Vertebrobasilar: Diplopia, vertigo, dysarthria, stupor/coma.
- 👁️ Ophthalmoplegic: III nerve palsy, must exclude PCA aneurysm.
- 👓 Retinal: Transient monocular visual constriction.
- 🎡 Benign recurrent vertigo: Vertigo responsive to migraine therapy.
- 🩸 Menstrual migraine: Linked to hormonal changes.
These questions are used to determine your score, which then is matched to a level of disability.
- How many days in the last 3 months did you miss work or school because of your headaches?
- How many days in the last 3 months was your productivity at work or school reduced by half or more because of your headaches? (Do not include days you counted in question 1 where you missed work or school.)
- On how many days in the last 3 months did you not do household work because of your headaches?
- How many days in the last three months was your productivity in household work reduced by half or more because of your headaches? (Do not include days you counted in question 3 where you did not do household work.)
- How many days in the last 3 months did you miss family, social or leisure activities because of your headaches?
Once you have answered these questions, add up the total number of days to determine your level of disability.
| Score | Grade | Disability |
|---|---|---|
| 0 to 5 | MIDAS Grade I | Little or no disability |
| 6 to 10 | MIDAS Grade II | Mild disability |
| 11 to 20 | MIDAS Grade III | Moderate disability |
| 21+ | MIDAS Grade IV | Severe disability |
What your Physician will need to know about your headache:
- A. On how many days in the last 3 months did you have a headache? (If a headache lasted more than 1 day, count each day.)
- B. On a scale of 0 - 10, on average how painful were these headaches? (where 0 = no pain at all and 10 = pain as bad as it can be.)
Acute Management
- 🛏️ Rest in dark, quiet room; sleep can abort attack.
- 💊 NSAIDs: Ibuprofen 400–600 mg, naproxen 500 mg.
- 💊 Aspirin 900 mg (avoid <16 years, pregnancy 3rd trimester).
- 💊 Triptans: Sumatriptan 50–100 mg PO, 20 mg nasal, or 6 mg SC (avoid in IHD, PVD, hemiplegic migraine).
- 🤢 Antiemetics: Metoclopramide or domperidone help nausea & absorption.
Prevention
- 🫀 Beta-blockers: Propranolol, atenolol (avoid in asthma).
- 🧃 Candesartan: ARB, effective off-license.
- 🌙 Amitriptyline: Low-dose TCA, helpful for comorbid insomnia.
- 💊 Topiramate: Effective but may cause paraesthesia, weight loss.
- 💉 Botulinum toxin A: For chronic migraine (≥15 days/month).
- 🧬 Fremanezumab: CGRP monoclonal antibody, specialist use.
- 🩸 Menstrual migraine: Frovatriptan 2.5 mg BID from 2 days before menses × 5 days.
References
Cases — Migraine
- Case 1 — Migraine Without Aura (“Common Migraine”) 💥: A 28-year-old woman presents with unilateral, throbbing headaches lasting 12 hours, associated with photophobia, phonophobia, and nausea. Attacks occur around menstruation. Diagnosis: Migraine without aura. Management: Acute: NSAID + triptan; Preventive: consider propranolol if frequent; menstrual migraine may benefit from perimenstrual triptan or hormonal therapy.
- Case 2 — Migraine With Aura (“Classic Migraine”) 🌈: A 35-year-old man reports visual zig-zag lines (scintillating scotoma) followed by unilateral headache with nausea and photophobia. Aura lasts 20 minutes and resolves before headache onset. Diagnosis: Migraine with aura. Management: Avoid vasoconstrictors if vascular risk factors; triptans for acute therapy; topiramate for prevention if frequent.
- Case 3 — Hemiplegic Migraine 🧠: A 19-year-old woman develops transient right arm weakness and dysphasia for 30 minutes, followed by severe left-sided headache. Brain imaging normal. Family history of similar attacks. Diagnosis: Familial hemiplegic migraine. Management: Avoid triptans/ergots; preventive therapy with verapamil or acetazolamide; genetic counselling.
- Case 4 — Status Migrainosus ⏳: A 40-year-old woman presents with continuous severe unilateral headache lasting >72 hours, unresponsive to her usual triptan. She has vomiting and photophobia. Diagnosis: Status migrainosus. Management: Hospital admission; IV fluids, antiemetics, IV NSAID or dihydroergotamine; exclude secondary causes.
- Case 5 — Chronic Migraine (Medication Overuse Headache) 💊: A 45-year-old man with longstanding migraine now has daily headaches. He takes OTC analgesics most days. Headaches are less severe but constant. Diagnosis: Chronic migraine with medication overuse headache. Management: Withdraw overused analgesics; introduce preventive therapy (e.g., topiramate, propranolol, botulinum toxin A if refractory); lifestyle measures.
Teaching Commentary 🧠
Migraine is a neurovascular disorder characterised by recurrent disabling headaches, often with aura. Key subtypes: - Without aura (commonest, unilateral throbbing, N/V, photophobia). - With aura (transient neurological symptoms, often visual). - Hemiplegic migraine (motor aura, mimics stroke). - Status migrainosus (prolonged, severe, emergency). - Chronic migraine (≥15 headache days/month, often with medication overuse). Management is stepwise: trigger avoidance → acute therapy (NSAIDs, triptans, antiemetics) → preventive therapy if frequent/severe (beta-blockers, topiramate, valproate, CGRP mAbs). Always consider red flags (first or worst headache, neuro deficits, papilloedema).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
