Pelvic Anatomy
The pelvis forms the bony ring connecting the spine and lower limbs.
It supports the trunk, protects pelvic organs, and provides attachment for muscles of locomotion, posture, and pelvic floor.
Clinically, it’s central to obstetrics, urology, colorectal surgery, and trauma care.
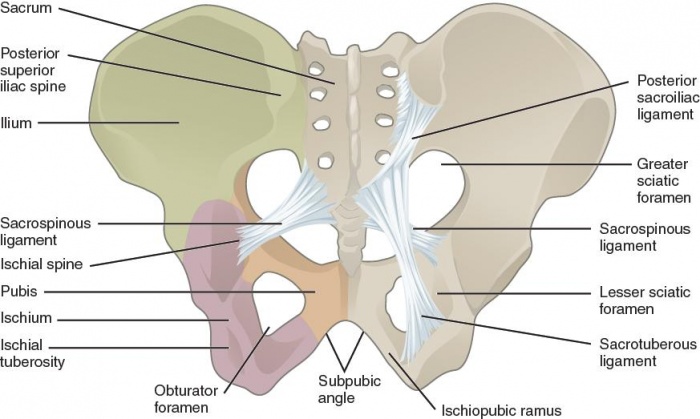
🏗️ Bony Pelvis Overview
- The pelvis is composed of two hip bones (ossa coxae), the sacrum, and the coccyx.
- Each hip bone develops from three fused bones:
- Ilium – broad, flared superior portion.
- Ischium – posteroinferior part with ischial tuberosity (“sitting bone”).
- Pubis – anterior portion meeting at the pubic symphysis.
- The two hip bones meet anteriorly at the pubic symphysis and posteriorly with the sacrum at the sacroiliac joints.
📏 Divisions of the Pelvis
- Pelvic brim (inlet) – line separating:
- False (greater) pelvis: above the brim, part of abdominal cavity.
- True (lesser) pelvis: below the brim, contains pelvic organs.
- Pelvic outlet – bounded by coccyx, ischial tuberosities, and pubic arch.
👩⚕️ Gender Differences
| Feature | Male | Female |
|---|
| Pelvic inlet | Heart-shaped | Oval, wider |
| Pelvic cavity | Narrow, deep | Shallow, roomy |
| Pubic arch | < 70° (acute) | > 80° (wide) |
| Sacrum | Long, curved | Short, less curved |
| Ischial spines | Project medially | Less prominent (wider outlet) |
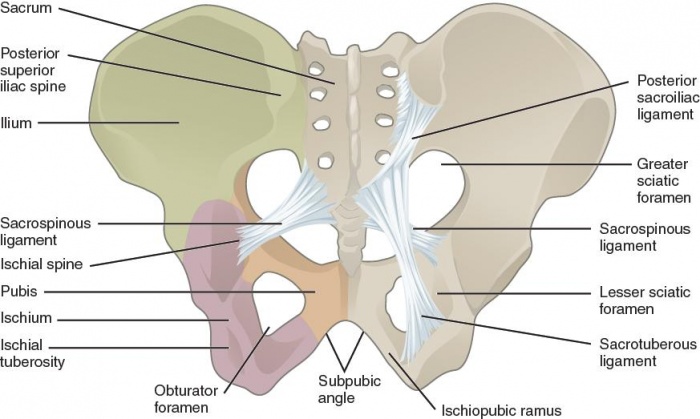
🔩 Joints & Ligaments
- Sacroiliac joints: between auricular surfaces of sacrum and ilium; strong synovial joints with limited movement.
- Pubic symphysis: fibrocartilaginous joint with small mobility (increased in pregnancy via relaxin).
- Sacrospinous ligament: sacrum → ischial spine; forms greater and lesser sciatic foramina.
- Sacrotuberous ligament: sacrum → ischial tuberosity; limits upward tilting of sacrum.
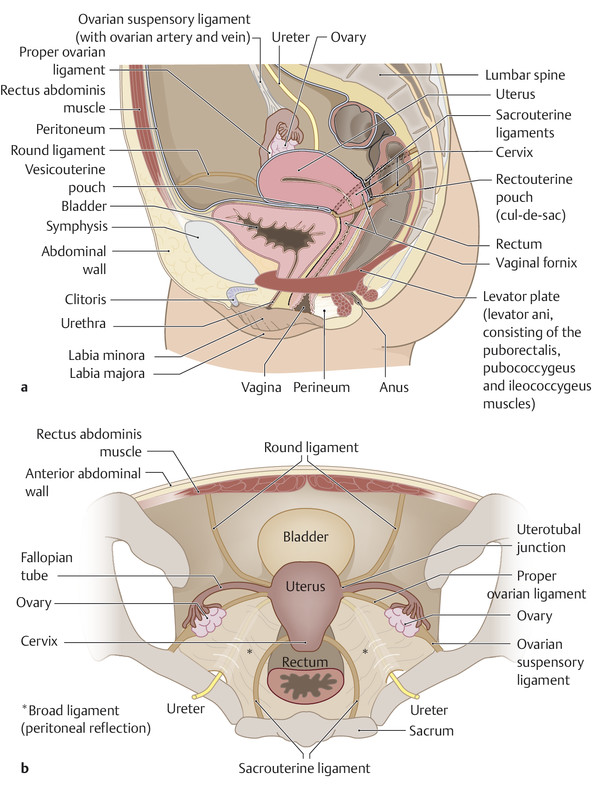
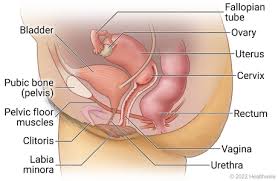
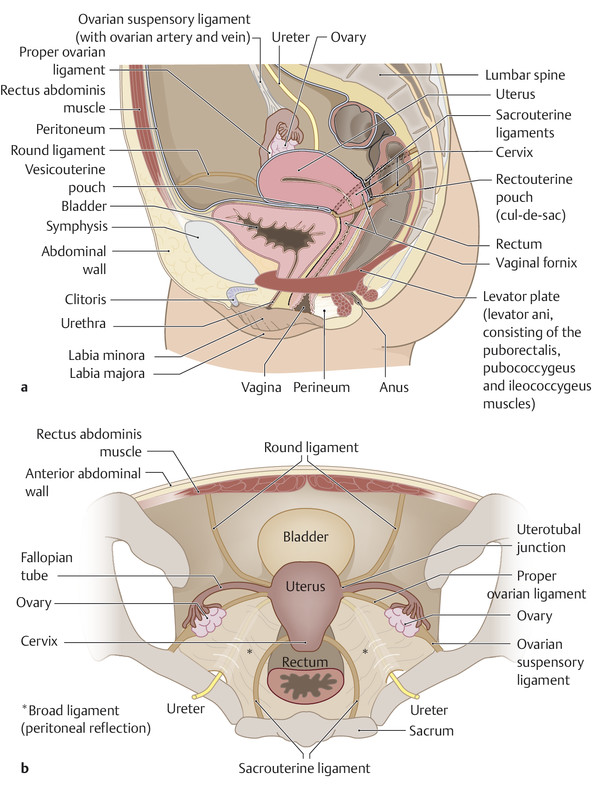
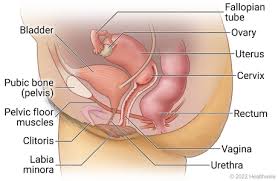
🧠 Pelvic Cavity & Peritoneal Relations
- Peritoneum drapes over pelvic viscera forming key pouches:
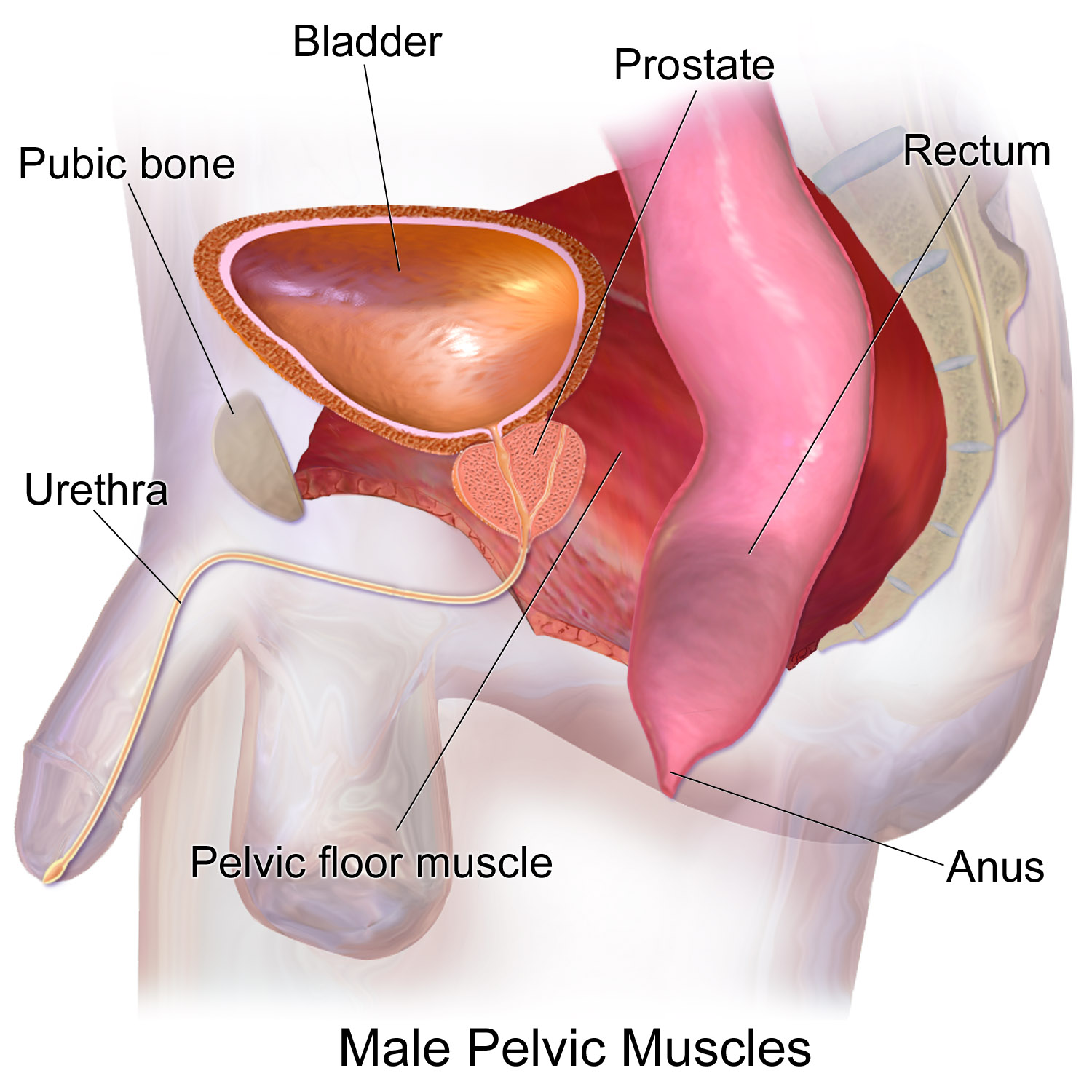
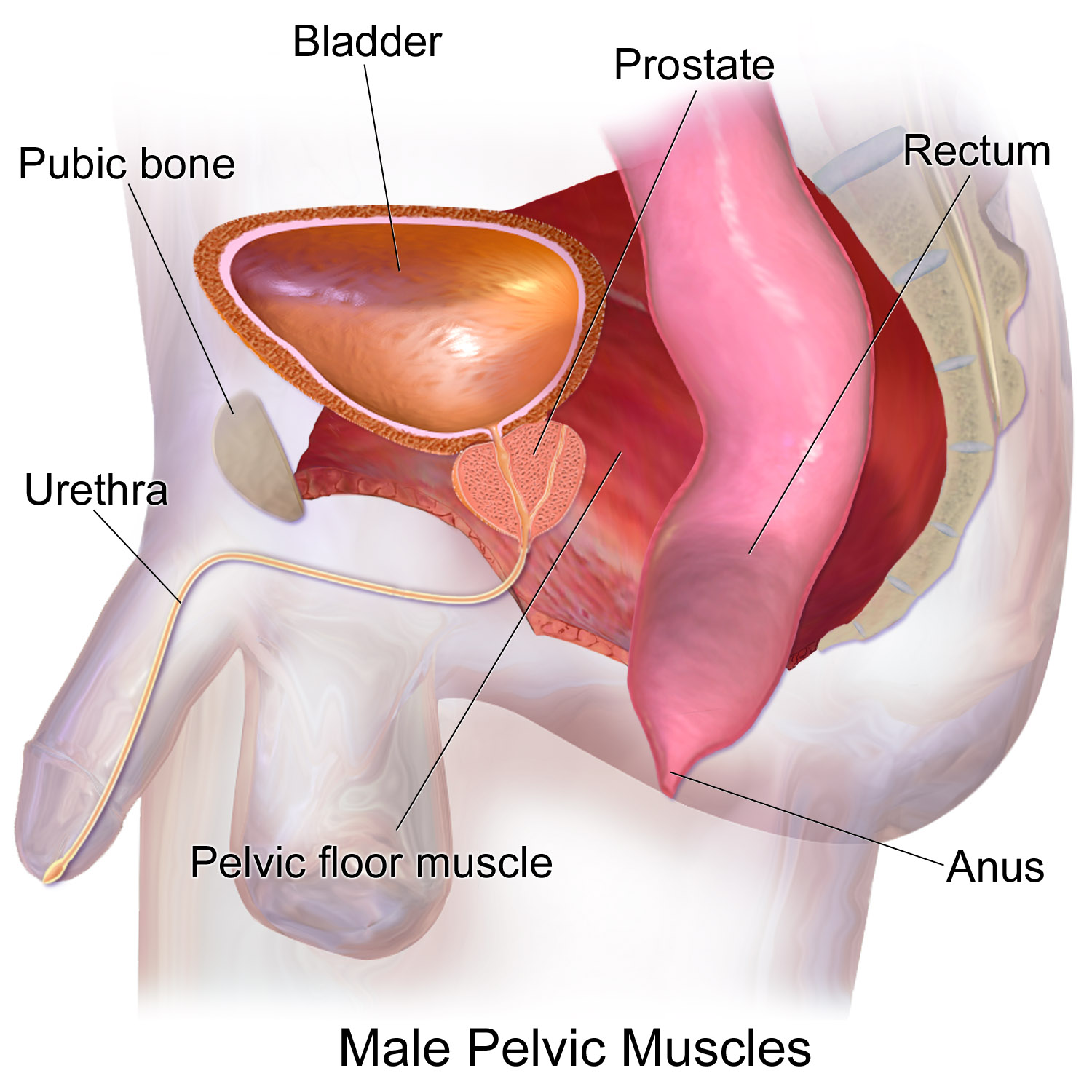
- Rectovesical pouch (males): between bladder and rectum.
- Vesicouterine and rectouterine (Douglas) pouches (females): important sites for free fluid or infection.
- In females, the broad ligament encloses the uterus, uterine tubes, and ovaries.
💧 Pelvic Organs Overview
| Organ | Key Features | Clinical Notes |
|---|
| Bladder | Muscular organ (detrusor) posterior to pubic symphysis; rises into abdomen when full. | Injury may occur in pelvic fractures; suprapubic catheterisation avoids peritoneal entry if distended. |
| Rectum | Continuation of sigmoid colon to anal canal; anterior surface related to prostate/vagina. | Digital rectal exam (DRE) assesses prostate, rectal masses, and tone. |
| Uterus | Pear-shaped organ between bladder and rectum; anteverted and anteflexed normally. | Retroversion common, may affect fertility or cause back pain. |
| Prostate | Fibromuscular gland surrounding proximal urethra. | Enlargement (BPH) causes obstructive voiding symptoms. |
🧍♀️ Pelvic Floor (Diaphragm)
- Supports pelvic viscera and maintains continence.
- Formed mainly by the levator ani group:
- Pubococcygeus – supports vagina, prostate, and rectum.
- Puborectalis – forms sling around anorectal junction; key in maintaining the anorectal angle.
- Iliococcygeus – posterior sheet of the diaphragm.
- Innervation: pudendal nerve (S2–S4) and direct branches of sacral plexus.
🩸 Blood Supply
- Arterial: Internal iliac artery (anterior division supplies pelvic viscera).
- Venous: Internal iliac veins form pelvic venous plexuses → risk of infection/thrombosis spread (e.g., prostatic plexus → vertebral veins).
- Lymphatic: Internal/external/common iliac and sacral nodes → para-aortic.
⚡ Nerve Supply
- Sacral plexus (L4–S4): supplies lower limb and perineum.
- Autonomic nerves:
- Sympathetic: from hypogastric plexus → vasoconstriction, ejaculation.
- Parasympathetic (S2–S4): pelvic splanchnic nerves → micturition, defaecation, erection.
🩻 Applied Anatomy
- Pelvic fractures: high-energy injuries with potential for massive haemorrhage (internal iliac branches).
- Childbirth injury: levator ani or pudendal nerve damage → pelvic organ prolapse, incontinence.
- Rectouterine pouch (Douglas): lowest peritoneal point – site of fluid collection; accessible via posterior fornix.
- Prostate cancer: spreads via venous plexus → lumbar spine metastases.
🧠 Clinical Pearls
- Visualise pelvis as a “bowl” of viscera supported by a muscular floor – helpful in understanding prolapse and continence.
- Always remember the S2–S4 roots: “keep the 3 Ps – pee, poo, and penis – working”.
- In pelvic surgery, careful respect for autonomic plexuses preserves bladder and sexual function.
📋 Summary Table
| Region | Main Structures | Clinical Significance |
|---|
| Pelvic inlet | Sacral promontory → pubic symphysis | Obstetric measurement (conjugate diameter) |
| True pelvis | Bladder, uterus/prostate, rectum | Pelvic organ pathology |
| Pelvic floor | Levator ani + coccygeus | Support; continence |
| Blood supply | Internal iliac arteries | Pelvic trauma haemorrhage |
| Innervation | Pudendal nerve, S2–S4 | Urinary/faecal continence |
🩺 Summary for Practice
A sound grasp of pelvic anatomy underpins safe catheterisation, childbirth management, prostate assessment, and surgical procedures.
Think spatially — the pelvis integrates skeletal support, vascular complexity, visceral organisation, and neurocontrol.
Clinically, dysfunction manifests as pain, incontinence, or organ prolapse — all rooted in this shared anatomy.