| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Diabetes Insipidus (AVP Deficiency)
🧪 Vasopressin (antidiuretic hormone, ADH; arginine vasopressin, AVP) is a nonapeptide synthesised in the hypothalamus and stored in the posterior pituitary. 💧 It is the key regulator of water reabsorption in the distal nephron. 📈 A rise in plasma osmolality of as little as 1% (threshold ~280–285 mOsm/kg H₂O) triggers AVP release → water retention + concentrated urine.
📖 About
- Produced in the supraoptic & paraventricular nuclei of the hypothalamus, stored in the posterior pituitary.
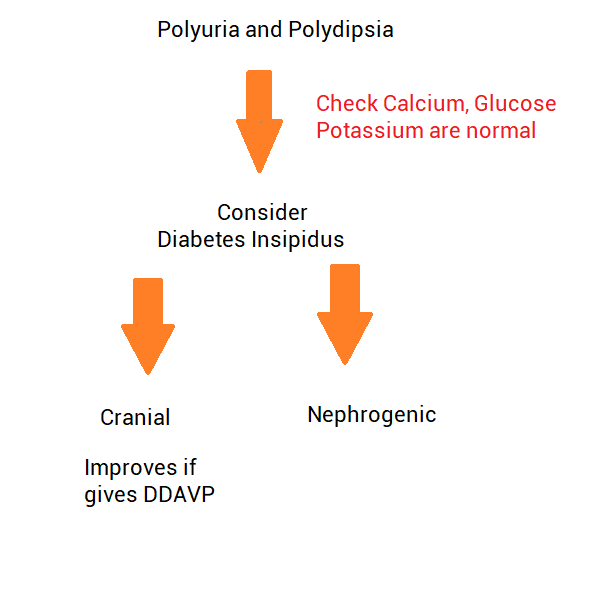
- Diabetes Insipidus (DI) = failure of AVP secretion or action → inability to concentrate urine → polyuria, polydipsia, hypernatraemia risk.
- 👉 Cranial DI: Impaired secretion.
👉 Nephrogenic DI: Kidneys unresponsive. - Severe DI: urine output can exceed 10–12 L/day.
⚙️ Physiology
- AVP release is controlled by plasma osmolality & blood volume/pressure.
- Acts via V2 receptors on collecting duct principal cells.
- Activates cAMP–PKA pathway → insertion of aquaporin-2 channels.
- Effect: ↑ water reabsorption, ↓ urine output, concentrated urine.
🧬 Aetiology
- Loss of AVP action → uncontrolled free water loss.
- If water intake inadequate → ⚠️ rapid dehydration & hypernatraemia.
- Note: >80–90% hypothalamic neuron loss needed before symptoms appear.
🧠 Cranial (Central) DI – Causes
- Idiopathic (most common in adults).
- Trauma, neurosurgery, craniopharyngioma.
- Sarcoidosis, TB, histiocytosis X.
- Meningitis, encephalitis, subarachnoid haemorrhage.
- Familial (rare, AD inheritance).
- Syndromic (e.g. DIDMOAD: DI, DM, optic atrophy, deafness).
🧩 Nephrogenic DI – Causes
- 💊 Drugs: Lithium, demeclocycline.
- ⚡ Electrolytes: Hypercalcaemia, hypokalaemia.
- CKD: Pyelonephritis, obstruction, amyloidosis, PKD.
- Inherited mutations: V2 receptor or aquaporin-2 defects.
- Systemic: Sickle cell disease, sarcoidosis.
📋 Clinical Features
- 💧 Polyuria: large volumes of dilute urine.
- 🚰 Polydipsia, intense thirst.
- ⚠️ Hypernatraemia if fluid intake inadequate → confusion, seizures, coma.
- ↑ VTE risk from haemoconcentration.
🔬 Investigations
- 🩺 Bloods: U&E (↑ Na⁺), ↑ plasma osmolality.
- 🧪 Urine: low osmolality despite high volume.
- 💡 Water deprivation test: confirms DI.
– Central DI: urine concentrates after desmopressin.
– Nephrogenic DI: no response to desmopressin. - Consider MRI brain (pituitary/hypothalamus).
🔎 Differential of Polyuria
- Diabetes mellitus (osmotic diuresis).
- Hypercalcaemia.
- Diuretics.
- Psychogenic polydipsia (excessive fluid intake).
- CKD.
- Post-obstructive diuresis.
💊 Management
- Cranial DI: Desmopressin (DDAVP) – intranasal, oral, or injection. ⚠️ Monitor for hyponatraemia.
- Nephrogenic DI: Low-salt diet, thiazides ± amiloride. NSAIDs (indomethacin) can ↓ urine output.
- Lithium-induced DI: Amiloride (blocks lithium uptake in collecting duct). Stop lithium if possible.
- General: Careful correction of hypernatraemia – avoid rapid shifts (risk of cerebral oedema).
📚 Teaching Pearls
💡 Exam buzzwords: Polyuria + hypernatraemia + low urine osmolality. 💡 Always distinguish from diabetes mellitus (check urine glucose). 💡 Water deprivation + desmopressin test = gold standard. 💡 In psychiatry patients with polydipsia, always consider psychogenic vs DI.
📚 References
Cases — Diabetes Insipidus (DI)
- Case 1 — Central DI after Pituitary Surgery 🧠: A 45-year-old woman develops sudden-onset polyuria (8 L/day) and polydipsia following transsphenoidal surgery for a pituitary macroadenoma. Urine: very dilute (osmolality 80 mOsm/kg). Plasma sodium: 152 mmol/L. Diagnosis: Central diabetes insipidus (loss of ADH secretion). Management: Desmopressin (DDAVP); fluid replacement; monitor electrolytes closely.
- Case 2 — Nephrogenic DI from Lithium 💊: A 60-year-old man with bipolar disorder on long-term lithium presents with excessive thirst and nocturia. Urine remains dilute despite rising serum osmolality. Water deprivation test: no response to desmopressin. Diagnosis: Nephrogenic diabetes insipidus secondary to lithium. Management: Stop lithium if possible; consider amiloride/thiazide + NSAIDs; low-salt, low-protein diet.
- Case 3 — Primary Polydipsia Mimicking DI 🚰: A 30-year-old woman reports constant thirst and drinking >6 L/day. Exam: normal. Labs: low-normal plasma sodium, urine osmolality increases significantly with water deprivation test. Diagnosis: Psychogenic (dipsogenic) polydipsia, not true DI. Management: Behavioural modification, psychiatric input; avoid unnecessary desmopressin (risk of hyponatraemia).
Teaching Commentary 🧠
Diabetes insipidus = impaired water reabsorption due to ADH deficiency (central) or renal resistance (nephrogenic). - Central DI: trauma, surgery, pituitary tumour, idiopathic. - Nephrogenic DI: lithium, hypercalcaemia, hypokalaemia, inherited. - Dipsogenic: excessive fluid intake mimics DI. Dx: Water deprivation test → central DI responds to desmopressin, nephrogenic does not, primary polydipsia concentrates with deprivation alone. Mx: Desmopressin for central; remove offending drugs + thiazides/amiloride for nephrogenic; behavioural therapy for dipsogenic.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
