| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Horner's syndrome
🦉 Horner’s Syndrome is caused by the loss of sympathetic nerve supply to the face and eye. It classically presents with ptosis, miosis, anhidrosis, and apparent enophthalmos. ⚠️ Important causes to exclude: lung apex malignancy (Pancoast tumour), carotid artery dissection, and lateral medullary infarct.
📍 Aetiology
- The sympathetic pathway originates in the hypothalamus, descends through the brainstem, exits at C8/T1, travels with the carotid artery, and finally enters the eye.
- Lesions along this 3-neuron pathway produce Horner’s syndrome.
🧠 Causes (By Neuron Level)
- First-order (Central): Brainstem and cervical cord lesions
- Stroke (especially lateral medullary syndrome).
- Tumours, demyelination (e.g., MS).
- Syringomyelia, trauma.
- Second-order (Preganglionic): Apex of lung / chest outlet
- Pancoast tumour (lung apex squamous carcinoma).
- Thoracic trauma or post-surgical damage.
- Schwannoma.
- Third-order (Postganglionic): Neck / carotid artery to the eye
- Carotid artery dissection or aneurysm.
- Base of skull tumours or infections.
- Cluster headaches / migraines.
- Birth trauma in children.
📊 Anatomy of Autonomic Supply
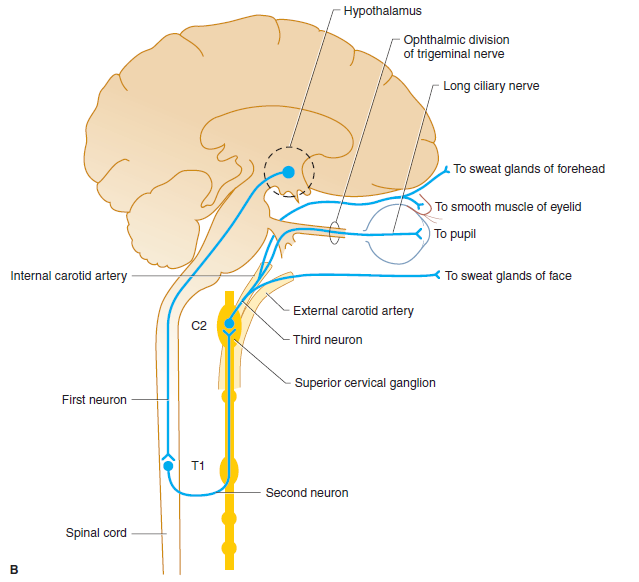
This 3-neuron oculosympathetic pathway runs: Hypothalamus → Spinal cord (C8–T1) → Superior cervical ganglion → Eye (pupil dilator, eyelid smooth muscle, facial sweat glands).
🩺 Clinical Features
- 👁️ Ptosis: Drooping of upper eyelid (loss of sympathetic innervation to Müller’s muscle).
- 🎯 Miosis: Constricted pupil that reacts normally to light.
- 💧 Anhidrosis: Reduced sweating on affected side (distribution depends on lesion level).
- ⚡ Apparent enophthalmos: Sunken eye appearance.
- Additional: Conjunctival injection; cough and cachexia if lung cancer-related.
📸 Case Studies
- Left Pancoast Tumour: Horner’s with ptosis from apical lung cancer.

- Idiopathic Horner’s: Left-sided, cause unknown.

- Classic Clinical Signs: Ptosis + miosis + anhidrosis.

🧪 Investigations
- Bloods: FBC, U&E; calcium or sodium derangements may suggest paraneoplastic lung cancer.
- Imaging:
- MRI brainstem for stroke.
- MRA neck for carotid dissection.
- CT chest for apical lung tumour (Pancoast).
- Pharmacological Testing:
- 1% cocaine drops: failure of pupil dilation confirms Horner’s.
- Apraclonidine drops may also be used (denervation supersensitivity → pupil dilates).
🩹 Management
- 🎯 Treat the underlying cause:
- Surgery / radiotherapy for lung cancer.
- Anticoagulation or stenting for carotid dissection.
- Stroke management if central cause.
- 👁️ Symptom management: Usually benign, but underlying pathology must never be missed.
💡 Clinical Pearls
- Think “Ptosis + Miosis + Anhidrosis = Horner’s until proven otherwise”.
- Always exclude 🚬 Pancoast tumour in a smoker with Horner’s + arm/shoulder pain.
- 🚑 Carotid dissection is a stroke emergency: look for ipsilateral head/neck pain + Horner’s.
Cases — Horner’s Syndrome
- Case 1 — Apical Lung Tumour (First-Order Neuron) 🫁: A 62-year-old man with a 40 pack-year smoking history presents with right-sided shoulder pain radiating to the arm. Exam: mild right ptosis, miosis, and anhidrosis. CXR shows a right apical mass. Diagnosis: Horner’s syndrome due to Pancoast tumour invading sympathetic chain. Management: Oncology referral; CT chest; biopsy for staging.
- Case 2 — Carotid Artery Dissection (Second-Order Neuron) ⚡: A 45-year-old man presents with sudden neck pain and headache after minor trauma. Exam: left ptosis and miosis without anhidrosis; no extraocular palsy. MRI angiography: left internal carotid artery dissection. Diagnosis: Painful Horner’s syndrome due to carotid dissection. Management: Urgent vascular input; anticoagulation/antiplatelets; stroke prevention.
- Case 3 — Cluster Headache (Third-Order Neuron) 💥: A 38-year-old man has recurrent severe left periorbital headaches lasting 1 hour, associated with ipsilateral lacrimation and nasal congestion. Exam during attack: mild ptosis and miosis on the left. Diagnosis: Horner’s syndrome associated with cluster headache. Management: High-flow oxygen, subcutaneous sumatriptan for acute attack; verapamil for prevention.
- Case 4 — Stroke-Related Horner’s 🧠: A 59-year-old man with vascular risk factors presents with acute vertigo, dysphagia, hoarseness, and loss of pain/temperature sensation on the right side of his face and left body. Exam: right-sided ptosis and miosis. MRI brain: infarct in right lateral medulla (posterior inferior cerebellar artery territory). Diagnosis: Horner’s syndrome secondary to lateral medullary (Wallenberg’s) syndrome. Management: Stroke care (antiplatelet therapy, risk factor modification, swallow assessment, rehab); supportive for Horner’s.
Teaching Commentary 🧠
Lateral medullary syndrome = classic brainstem stroke syndrome (PICA or vertebral artery occlusion). Key features: - Ipsilateral: facial pain/temperature loss (trigeminal nucleus), Horner’s syndrome (sympathetic tract), ataxia (cerebellar peduncle), palate weakness (nucleus ambiguus → dysphagia/hoarseness). - Contralateral: body pain/temperature loss (spinothalamic tract). Mnemonic: “Don’t PICA horse (hoarseness) that can’t eat (dysphagia)”. Management: same as ischaemic stroke (antiplatelets, risk factor control, swallow therapy). Prognosis depends on severity of bulbar dysfunction.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
