| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Drug Reaction Eosinophilia Systemic Symptoms (DRESS syndrome)
Related Subjects: |Acute Severe Asthma |Eosinophilic granulomatosis (Churg Strauss) |Loffler's syndrome (Pulmonary Eosinophilia) |Pulmonary Eosinophilia and CXR changes |Drug Reaction Eosinophilia Systemic Symptoms
🚨 DRESS Syndrome (Drug Reaction with Eosinophilia and Systemic Symptoms) is a life-threatening idiosyncratic drug reaction with mortality of ~10%. It causes a widespread skin eruption, fever, lymphadenopathy, and can involve multiple organs (liver, kidneys, lungs, heart).
📖 About
- Severe, delayed-onset hypersensitivity reaction (latency 2–8 weeks).
- Also called anticonvulsant hypersensitivity syndrome.
- Classified as one of the Severe Cutaneous Adverse Reactions (SCARs) alongside SJS/TEN.
🧪 Aetiology
- Most commonly triggered by aromatic anticonvulsants (carbamazepine, phenytoin, lamotrigine, phenobarbital).
- Other drugs: allopurinol, minocycline, abacavir, nevirapine, vancomycin, sulfonamides, NSAIDs.
- Genetic predisposition (e.g. HLA-B*58:01 and allopurinol in Han Chinese patients).
- Latency: typically 2–6 weeks, longer than most other drug reactions.
💊 High-Risk Drugs
- Anticonvulsants: Carbamazepine, Phenytoin, Lamotrigine, Valproate.
- Anti-infectives: Sulfonamides, Minocycline, Dapsone, Vancomycin, Doxycycline.
- Others: Allopurinol, Abacavir, Nevirapine, Clozapine, Rituximab, NSAIDs.
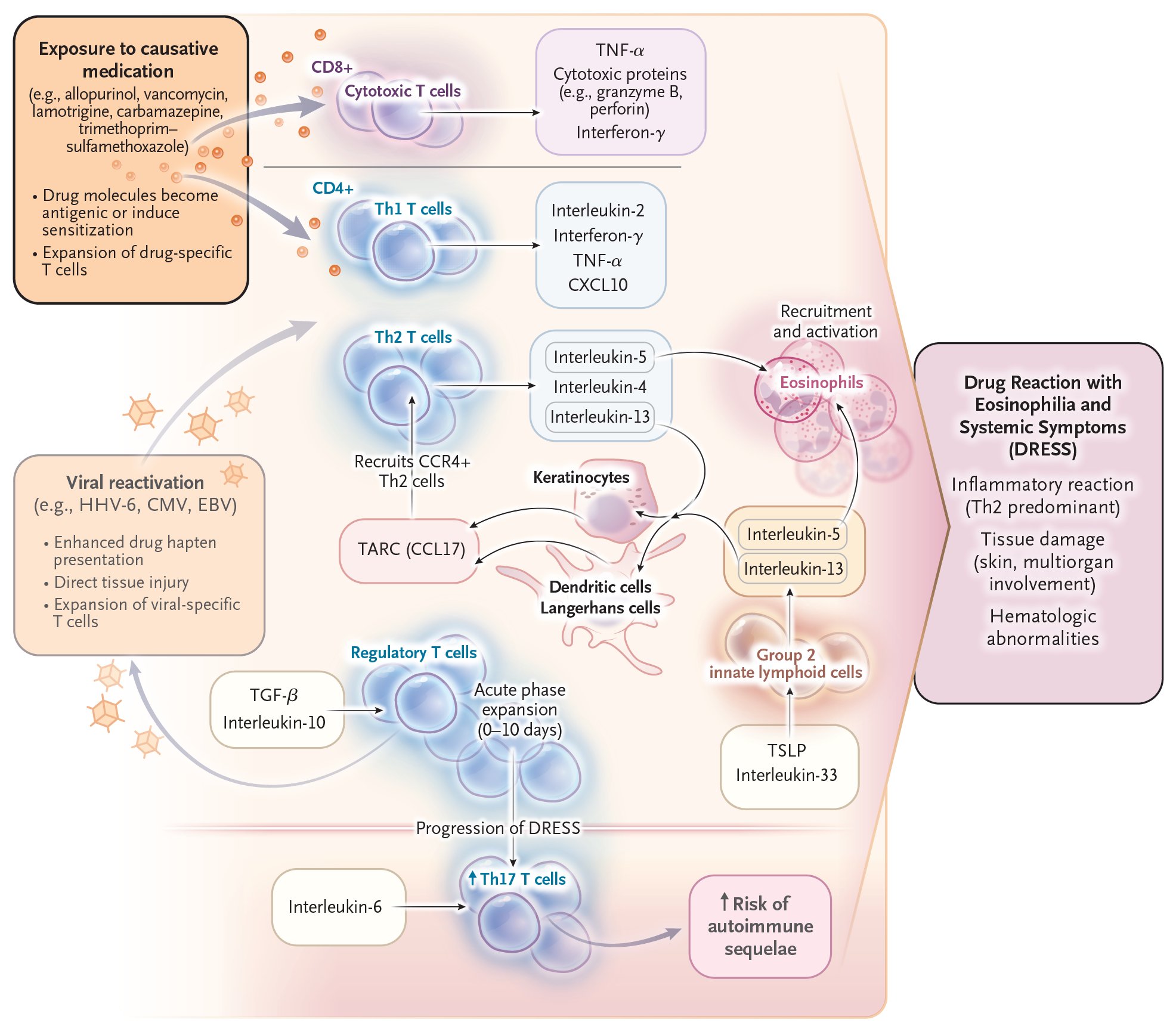
🩺 Clinical Features
- Onset 2–8 weeks after drug initiation.
- Systemic symptoms: Fever, lymphadenopathy, malaise.
- Skin: Morbilliform/maculopapular eruption, urticaria, vesicles, bullae, target lesions, erythroderma, facial oedema.
- Internal organs: Hepatitis (commonest), nephritis, pneumonitis, myocarditis, colitis.
- May overlap with SJS/TEN or erythema multiforme.
🔬 Investigations
- Bloods: Eosinophilia, atypical lymphocytosis, leukocytosis, abnormal LFTs, renal impairment.
- Rule out other causes (viral hepatitis, EBV/CMV, autoimmune disease).
- RegiSCAR criteria used for standardised diagnosis.
⚕️ Management
- 🚫 Immediate withdrawal of the offending drug (key determinant of prognosis).
- Supportive care: fluids, electrolyte balance, nutritional support.
- Corticosteroids (e.g. Prednisolone) often used if systemic involvement, though evidence is limited.
- Ciclosporin and other immunosuppressants may be used in severe/refractory cases.
- Close ITU/HDU monitoring if multi-organ failure risk.
🛡️ Prevention
- Genetic screening (e.g. HLA-B*58:01 before allopurinol, HLA-B*15:02 before carbamazepine in high-risk populations).
- Educate patients about early warning signs (rash, fever).
- Avoid re-exposure to the offending drug or structurally similar compounds.
📈 Prognosis
- Mortality ~10%, mainly due to fulminant hepatitis or myocarditis.
- Early recognition and drug withdrawal greatly improve outcomes.
- Possible long-term sequelae: chronic kidney disease, autoimmune thyroiditis, type 1 diabetes.
✅ Conclusion
- DRESS is a severe, delayed drug hypersensitivity syndrome with multi-organ involvement.
- Rapid recognition, drug cessation, and supportive care are vital for survival.
- Preventive strategies (genetic testing, education, monitoring) reduce incidence and severity.
📚 References
3 Clinical Cases — DRESS Syndrome 💊🔥🩸
- Case 1 — Anticonvulsant-related DRESS 🧠: A 27-year-old man started on carbamazepine for epilepsy 5 weeks ago develops fever, widespread morbilliform rash, facial oedema, and lymphadenopathy. Bloods: eosinophilia and raised ALT/AST. Teaching: Classic culprit drugs are aromatic anticonvulsants (carbamazepine, phenytoin, lamotrigine). DRESS typically appears 2–8 weeks after exposure. Management: stop the drug immediately, supportive care, and systemic corticosteroids if organ involvement.
- Case 2 — Antibiotic-induced DRESS 💉: A 45-year-old woman treated with vancomycin for MRSA endocarditis presents with high-grade fever, diffuse erythematous rash, and swelling of the face. Bloods: eosinophilia, atypical lymphocytes, and renal impairment. Teaching: Antibiotics such as vancomycin, minocycline, and sulfonamides can trigger DRESS. Key danger = multi-organ involvement (especially kidney, liver). Withdrawal of the drug + systemic steroids is essential.
- Case 3 — Allopurinol-associated DRESS 🦶: A 68-year-old man recently started on allopurinol for gout prophylaxis develops fever, malaise, extensive exfoliative rash, and marked facial oedema. Bloods: eosinophilia, deranged LFTs, and creatinine rise. Teaching: Allopurinol is a leading cause of DRESS, particularly in older patients with renal impairment. Risk factors include HLA-B*58:01 allele (high prevalence in Asian populations). Stopping the drug promptly is life-saving, with steroids often required.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
