| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Fractured Neck of Femur/Femoral Neck
Related Subjects: |Fractured Neck of Femur |Fractured Shaft Femur |Supracondylar Femur Fractures |Femoral fractures and Injuries
⚠️ Key Point: Intracapsular fractures have a higher incidence of AVN (Avascular Necrosis) and non-union due to the femoral head blood supply. 👉 If displacement is minimal → internal fixation gives best outcome. 👉 If displaced → high risk of AVN, so prosthesis insertion is usually required.
ℹ️ About
- 🦴 Intracapsular fractures carry high AVN risk.
- ☠️ 30% of patients die within 1 year.
- 👵 Most common in the elderly due to frailty and falls.
- 🧓 Patients often have multiple co-morbidities.
- 🦴 Osteoporosis is the major underlying factor.
📊 Epidemiology
- ~80,000 hip fractures per year in the UK.
- Numbers are rising as the population ages.
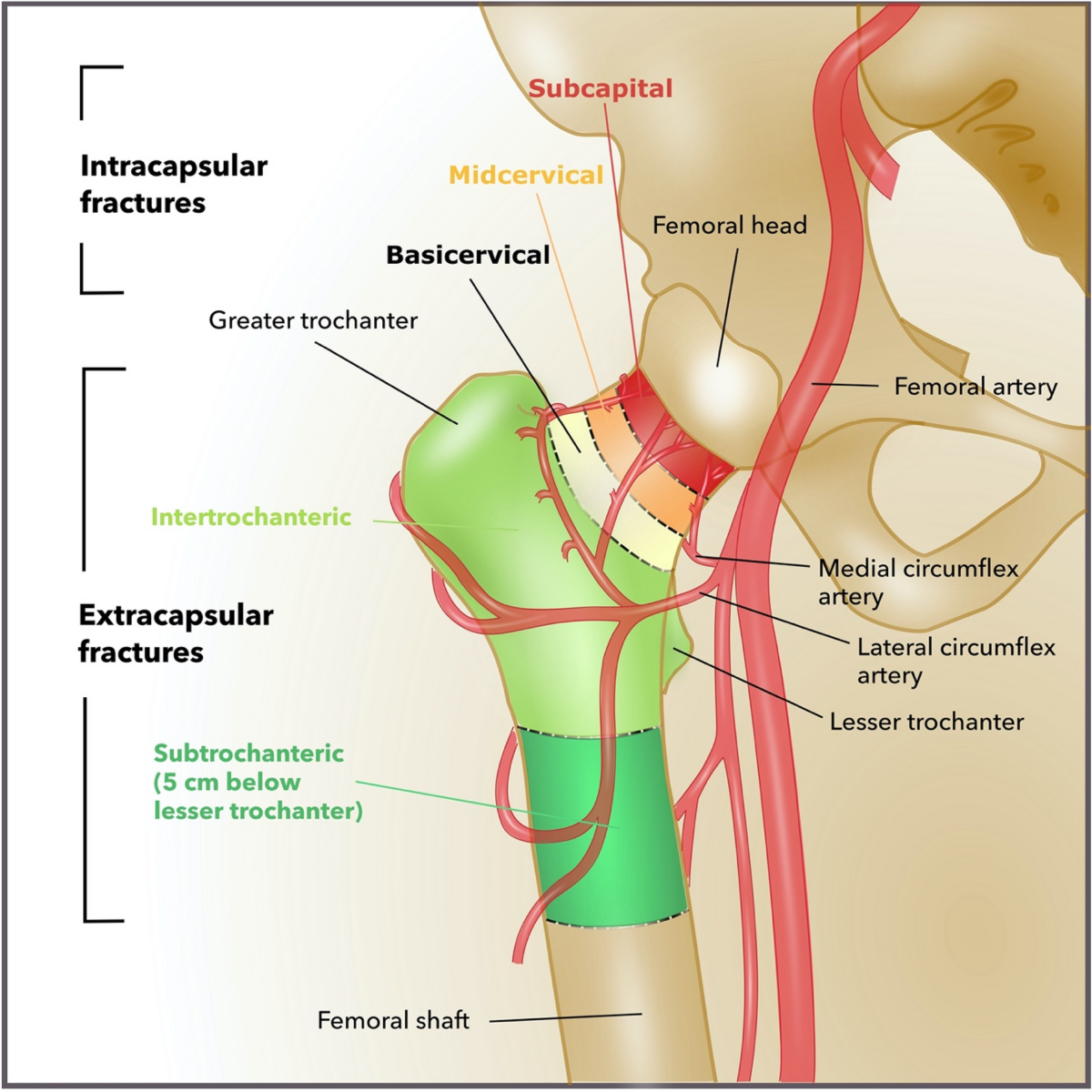
🧠 Anatomy
🧬 Aetiology
- Falls + Osteoporosis are the commonest causes.
- The medial femoral circumflex artery supplies the femoral head ➝ vulnerable in NOF fractures.
- Vascular compromise ➝ ischaemia ➝ AVN.
📉 Risk Factors for Bone Fragility
- Osteoporosis: age, inactivity, smoking, alcohol, low BMI, family history.
- Previous fragility fracture ➝ doubles future fracture risk.
- Other causes: metastases, Paget’s disease, osteomalacia, hyperparathyroidism, myeloma.
🤕 Risk Factors for Falls
- Muscle weakness, gait or balance problems.
- Neurological diseases: Parkinson’s, stroke.
- Poor vision.
- Medications: sedatives, hypnotics, diuretics, antihypertensives, alcohol.
🩺 Clinical Features
- Pain + external rotation, adduction, and shortening of the affected leg.
- History: establish whether mechanical fall or medical cause (syncope, arrhythmia, hypotension).
- Check co-morbidities that influence management.
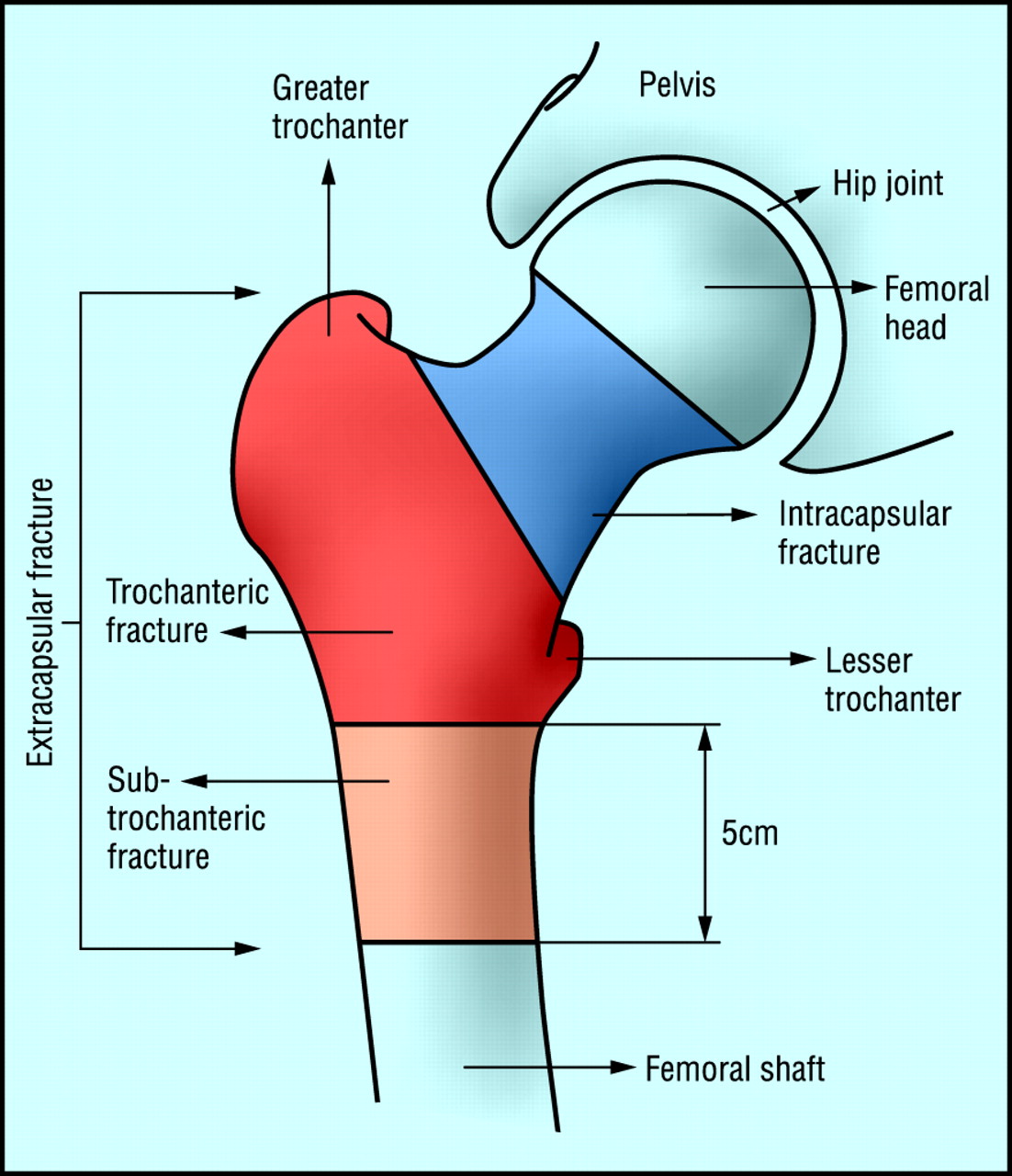
📌 Types of Fracture
- Intracapsular: High risk of AVN + non-union. Tx = hemiarthroplasty/THR.
- Subcapital & Transcervical: Common intracapsular fracture patterns.
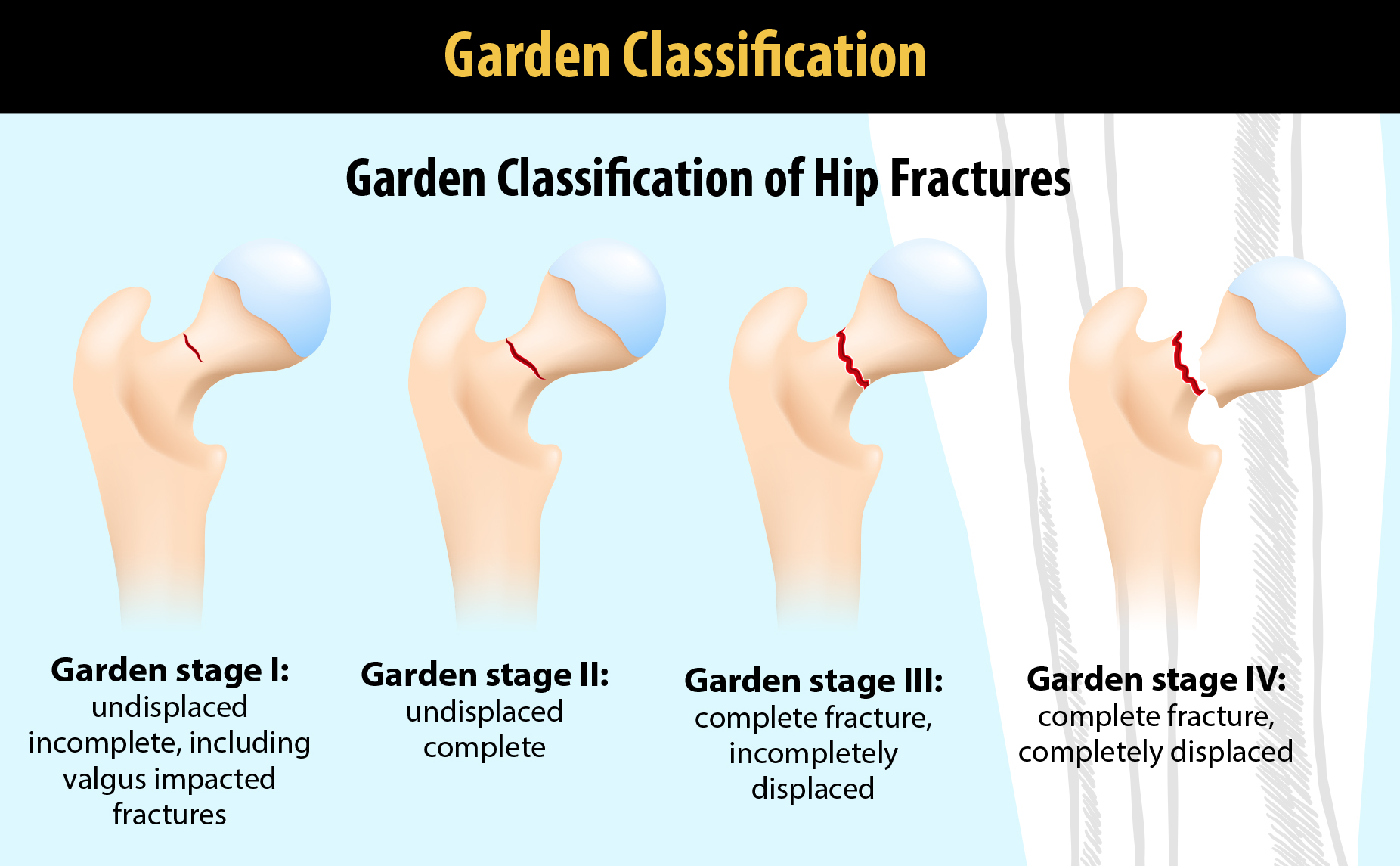
🗂️ Garden Classification
- Type I: Incomplete fracture
- Type II: Complete, undisplaced
- Type III: Complete, partially displaced
- Type IV: Complete, fully displaced
📌 Extracapsular Fractures
- Trochanteric
- Transtrochanteric
- Subtrochanteric
Other Fractures
- Pubic ramus fractures (usually conservative).
- Acetabular fractures (conservative unless complex).
🔍 Investigations
- Baseline bloods: FBC, U&E, clotting, group & save.
- CXR + ECG (pre-op assessment).
- Pelvic AP X-ray (compare both hips, check pubic rami).
- Lateral hip X-ray (often diagnostic when AP is normal).
- MRI/CT if X-rays inconclusive (10% occult fractures).
🛡️ Prevention
- Falls risk assessment + home/environment modifications.
- Muscle strengthening + balance retraining (e.g. Tai Chi).
- Bisphosphonates increase bone density, reduce fracture risk.
- Calcium, Vitamin D, ± HRT can reduce risk.
📊 Mortality: 10% at 30 days, 30% at 12 months (reflecting frailty + co-morbidities).
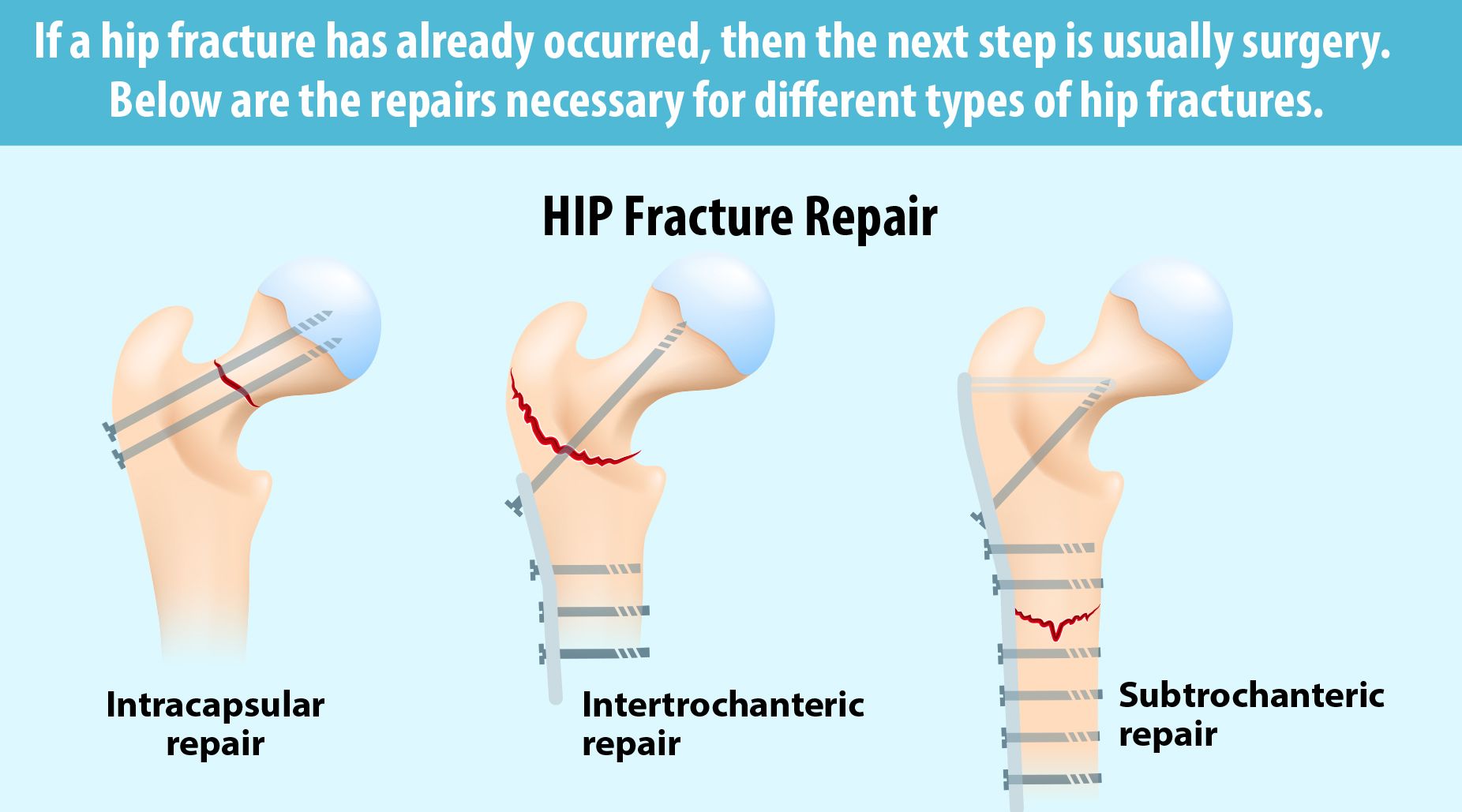
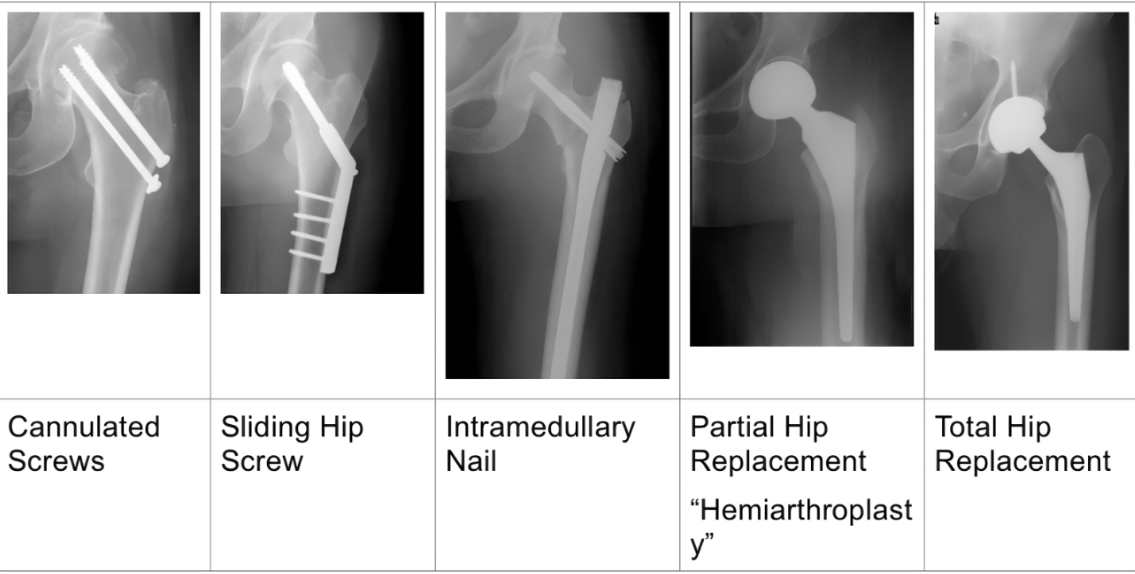
🛠️ Treatment Options
- Conservative: For patients unfit for surgery ➝ bed rest, analgesia, physio. Poor outcomes.
- Surgical: Standard of care.
- Internal fixation: For undisplaced intracapsular (cannulated screws/DHS). Also for young with displaced fractures.
- Hemiarthroplasty: For older patients with displaced fractures ➝ faster recovery.
- Total Hip Replacement (THR): For active elderly/younger displaced fractures ➝ better function long term, higher surgical risk.
- Intramedullary nailing: For extracapsular/subtrochanteric fractures ➝ early mobilisation.
- DHS: For intertrochanteric fractures ➝ controlled collapse and healing.
In frail elderly after a hip fracture, annual IV zoledronate not only prevents further fractures but also reduces mortality. This is unique among osteoporosis treatments and why geriatricians are so keen to give it post-fracture. 5 mg IV once yearly, infused over at least 15 minutes. Ensure adequate vitamin D and calcium before infusion (correct hypocalcaemia).
🩺 Management
- ABC resuscitation.
- Analgesia (including fascia iliaca block).
- IV fluids & electrolyte correction.
- Orthogeriatric review early.
- Admit + imaging if unable to walk or occult fracture suspected.
- Assess mental state, pressure sore risk, nutrition.
- Surgery:
- Intracapsular undisplaced ➝ cannulated screws.
- Intracapsular displaced ➝ hemiarthroplasty or THR if fit.
- Extracapsular ➝ screws/nailing depending on pattern.
- VTE prophylaxis ➝ stockings + LMWH/DOAC until mobilising.
🏃♀️ Post-Surgical Care & Rehabilitation
- Early mobilisation with physio ➝ prevents DVT, improves outcomes.
- Pain management + infection prophylaxis.
- Monitor for complications: infection, non-union, prosthetic dislocation.
- Rehab programmes: strength, balance, gait training ➝ reduce future falls.
⚠️ Complications
- AVN (esp. intracapsular fractures).
- Non-union (esp. displaced fractures).
- Osteoarthritis.
- DVT/PE.
- Surgical site infection, prosthetic dislocation.
📈 Prognosis
- Outcome depends on age, co-morbidities, and rapidity of surgery.
- Mortality: ~30% at 1 year, largely due to frailty not fracture itself.
- Good surgical + rehab care ➝ mobility and independence can be maintained.
✅ Conclusion
Fractured neck of femur is a major orthopaedic emergency, common in elderly patients with osteoporosis and falls. Intracapsular fractures are particularly high risk due to compromised blood supply ➝ AVN + non-union. Prompt surgical management (fixation or replacement), multidisciplinary orthogeriatric input, and effective rehab are key to improving survival and function.
📚 References
- Royal College of Physicians – Fractured Neck of Femur
- NICE – Hip Fracture Management Guidelines
- Mayo Clinic – Hip Fracture
- UpToDate – Hip Fracture Overview
- British Orthopaedic Association – Hip Fracture Guidance
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
