| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Frailty an Overview
Frailty is a multisystem clinical syndrome of decreased physiological reserve and resilience, making older adults vulnerable to stressors. 📌 It is not inevitable with ageing, but more common with increasing age and multimorbidity.
⚙️ Pathophysiology
- Frailty reflects dysregulation across multiple systems:
- 💪 Musculoskeletal: sarcopenia → reduced strength and mobility.
- 🧠 Neurological: impaired cognition, balance, reaction times.
- 🫁 Cardiopulmonary: reduced reserve, poor tolerance to stress.
- 🩸 Immune / Endocrine: inflammageing, insulin resistance, reduced vitamin D.
- Result = homeostatic instability → small insults (infection, fall, new drug) → disproportionate decline.
📊 Models of Frailty
- 🔬 Phenotype (Fried): frailty = ≥3 of 5 (weight loss, exhaustion, weakness, slow gait, low activity).
- 📈 Deficit accumulation (Rockwood): frailty index = ratio of deficits present.
- 📏 Clinical Frailty Scale (CFS): 1–9, quick bedside tool → widely used in UK (NHS, NICE, BGS).
🧾 Frailty Syndromes (the “Geriatric Giants”)
- 🚶 Falls: impaired balance, weakness, home hazards.
- 🧠 Delirium: acute confusion, often with infection, pain, drugs.
- 🚽 Incontinence: bladder or bowel, loss of independence.
- 💊 Polypharmacy: multiple medications → adverse events, interactions.
- 📉 Immobility: pressure sores, deconditioning, pneumonia.
🔍 Clinical Features
- General: fatigue, unintentional weight loss, frequent infections.
- Physical: slow walking speed, weak grip, recurrent falls.
- Cognitive: poor concentration, memory issues.
- Functional: dependence in ADLs/IADLs, poor recovery after illness.
📉 Consequences of Frailty
- ⚡ Increased risk of falls, fractures, delirium, disability.
- 🏥 More hospitalisations, longer stays, higher readmission rates.
- 🧩 Greater dependency on care homes and social care.
- ☠️ Increased mortality risk.
🧪 Assessment Tools
- 📏 Clinical Frailty Scale (CFS) – quick bedside stratification.
- 🏃 Gait speed – <0.8 m/s = frailty marker.
- 💪 Grip strength – reduced = sarcopenia indicator.
- 📊 Frailty Index – research/academic use.
- 📋 Edmonton Frail Scale – broader screening (cognition, mood, meds, nutrition, continence).
⚕️ Management Principles
- 🩺 Comprehensive Geriatric Assessment (CGA) → holistic, MDT approach.
- 💊 Medication optimisation → deprescribe where possible.
- 🏃 Exercise & rehab → resistance training, physio to improve strength/balance.
- 🥗 Nutrition → protein, vitamin D, calcium supplementation.
- 🧠 Cognitive support → screen for delirium & dementia, optimise hearing/vision.
- 👪 Social support → carers, social worker, community resources.
- 📜 Advance care planning → discuss goals of care, avoid burdensome treatments.
🌍 UK Context
- 📌 NICE: frailty is a long-term condition requiring proactive identification and management.
- 📌 NHS England: CFS recommended for ≥65s in hospital/ICU to guide decisions.
- 📌 BGS: promote frailty identification in community (GP, care homes).
- 📌 QOF (primary care): practices incentivised to code frailty and undertake medication reviews & falls risk assessment.
💡 Teaching pearl: Frailty is dynamic and potentially reversible → interventions like nutrition, exercise, and deprescribing can slow progression. Think of frailty as a "red flag vital sign" in older adults.
References
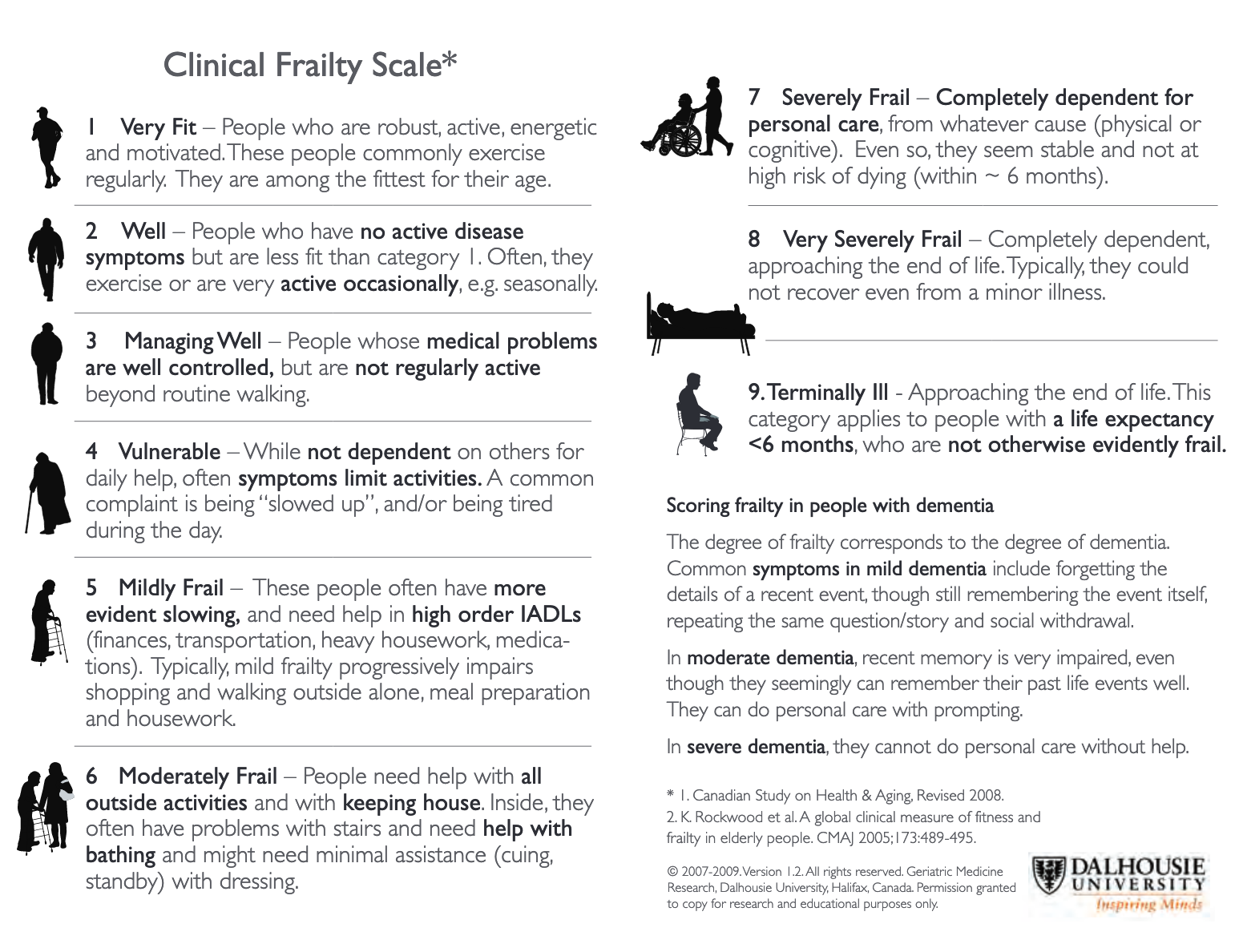
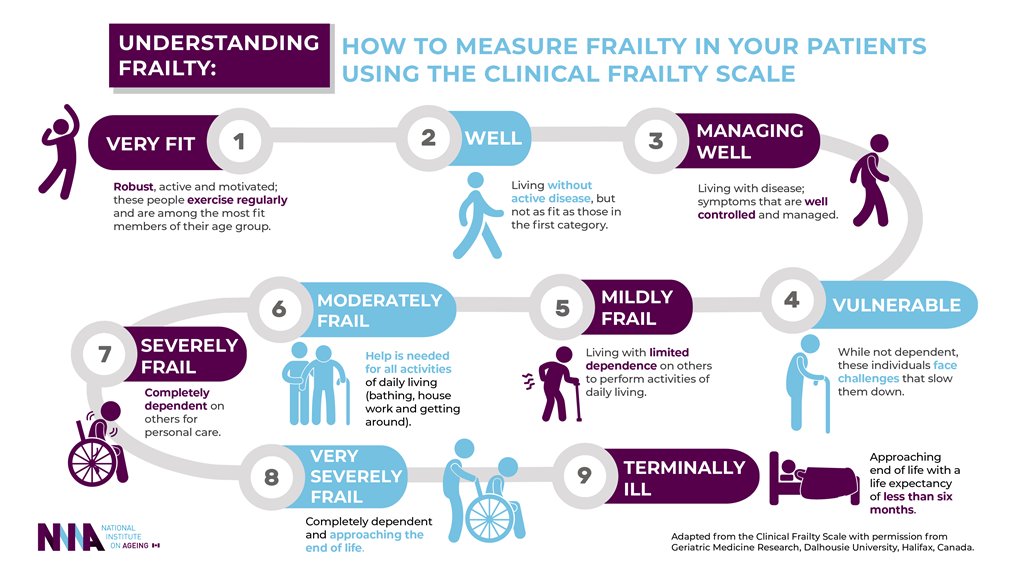 The Rockwood Clinical Frailty Scale is often used to categorize levels of frailty in older adults.
The Rockwood Clinical Frailty Scale is often used to categorize levels of frailty in older adults.
Revisions
- Ensure updates and revisions based on emerging research and clinical guidelines for the management of frailty.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
