| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Human Herpesvirus 6A (HHV-6A)
🧠 HHV-6 Encephalitis is a serious complication after stem cell transplants, often presenting with:
⚡ Hyponatraemia
| 🧩 Cognitive decline
| ⚠️ Seizures
| 📉 Memory loss
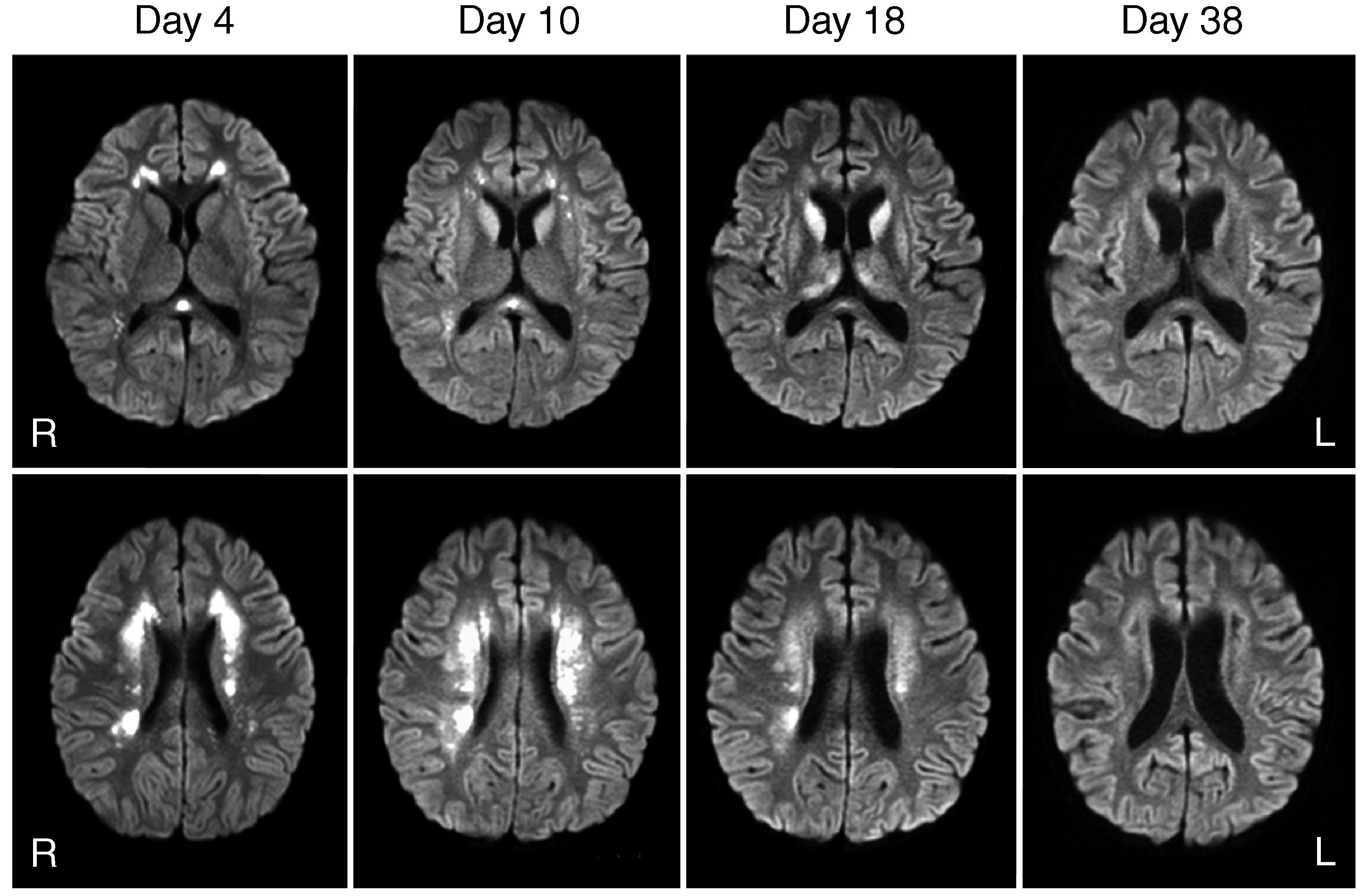
🧪 CSF & PCR are diagnostic gold standards. MRI (T2, FLAIR, DWI) typically shows hyperintensities in the medial temporal lobes, amygdala, and hippocampus.
💊 Treat with antivirals (foscarnet or ganciclovir). Prompt diagnosis is essential to prevent permanent neurological damage.
🔎 Overview
- HHV-6 = collective term for HHV-6A and HHV-6B.
- HHV-6A belongs to the Herpesviridae family (like HSV & CMV).
- HHV-6B commonly causes 🌸 roseola infantum in children.
- HHV-6A is less understood, often reactivates in immunocompromised patients.
- It is a double-stranded DNA virus, with T-lymphocytes as the main target.
📤 Transmission
- Worldwide, ubiquitous virus.
- HHV-6A: spread via close contact & saliva (exact routes unclear).
- Usually asymptomatic in healthy individuals.
- Reactivation occurs in immunosuppression ➝ drives complications.
🧬 Pathogenesis
- HHV-6A: infects CD4+ T cells, glial cells, macrophages, and epithelial cells. 🛑 Latency in monocytes/macrophages ➝ reactivation when immune defences fail. 🌀 Can disrupt immune balance → chronic inflammation, autoimmunity, or neurological disease.
- HHV-6B: causes roseola infantum (exanthema subitum) with fever + rash. ⚠️ Accounts for ~10–17% of febrile ED attendances in <36-month-olds.
🩺 Clinical Manifestations
- HHV-6A reactivation linked to:
- Neurological disease: encephalitis, MS associations, cognitive decline, seizures, SIADH.
- Chronic fatigue syndrome (possible role, under study).
- Immunosuppression in transplant patients.
- Worsening HIV progression by depleting CD4+ T cells.
- In healthy people ➝ often asymptomatic or mild flu-like illness.
🧪 Diagnosis
- PCR: most sensitive for viral DNA in blood/CSF.
- Serology: limited in distinguishing HHV-6A vs HHV-6B.
- Viral culture: rarely practical (needs high viral load).
- Tissue biopsy: brain biopsy in severe encephalitis cases.
- MRI: hyperintensity in medial temporal lobes (hippocampus + amygdala).
- EEG: temporal lobe epileptiform discharges may be seen.
🧒 Primary Infection
HHV-6B = roseola infantum → high fever + rash in infants. Complication: febrile seizures (most common). Rarely, acute encephalopathy.
💊 Treatment
- Most primary HHV-6 infections = self-limiting, resolve in 5–7 days.
- Complications: febrile seizures, encephalopathy due to neurotropic effect.
- For severe HHV-6A disease: use antivirals
- 🧪 Ganciclovir
- 🧪 Foscarnet
- 🧪 Cidofovir
- Supportive therapy: seizure control, management of raised ICP, fluid balance in SIADH.
⚠️ Complications
- Encephalitis: transplant recipients most at risk.
- Multiple sclerosis: association proposed, not proven.
- Chronic fatigue syndrome: under research as possible trigger.
- Long-term cognitive decline after encephalitis.
🛡️ Prevention
- No vaccine currently available.
- Strategies: close monitoring in immunocompromised patients (esp. transplant, HIV).
- Pre-emptive screening with PCR in post-transplant settings.
- Rapid initiation of antivirals when reactivation suspected.
📌 Conclusion
- HHV-6A is less understood than HHV-6B but is emerging as a key cause of CNS disease post-transplant.
- Diagnosis requires high suspicion + early PCR/MRI.
- Early antiviral therapy can prevent severe, irreversible neurological injury.
💡 Teaching Pearl: In transplant medicine, always consider HHV-6 encephalitis when you see: 📉 Memory loss + 🌙 confusion + ⚡ seizures + 🔬 hyponatraemia (SIADH). These are red flags for early MRI & PCR testing.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
