| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Diabetes: Eye Disease
Related Subjects: Type 1 DM |Type 2 DM |Diabetes in Pregnancy |HbA1c |Diabetic Ketoacidosis (DKA) Adults |Hyperglycaemic Hyperosmolar State (HHS) |Diabetic Nephropathy |Diabetic Retinopathy |Diabetic Neuropathy |Diabetic Amyotrophy |Maturity Onset Diabetes of the Young (MODY)
👁️ Diabetic retinopathy is largely preventable: tight glycaemic control, BP and lipids slow microvascular damage; timely laser/anti-VEGF preserves sight. In the UK, routine annual screening from age 12 (NHS DES) catches asymptomatic disease early.
📖 About
- ~50% of T1D affected within 10–15 years; ~50% of T2D within 15 years. Most changes are mild if detected early.
- Risk rises with diabetes duration, hyperglycaemia (HbA1c), hypertension, dyslipidaemia, nephropathy, pregnancy, and smoking.
🧠 Pathophysiology (why VEGF rises)
- Chronic hyperglycaemia → pericyte loss, basement-membrane thickening, capillary dropout → retinal ischaemia.
- Ischaemia ↑VEGF → ↑permeability (macular oedema) and fragile neovascularisation (proliferative disease).
🩺 Screening (UK focus)
- Annual mydriatic digital photography (NHS DES). Symptomless until late stages—screening is crucial.
- Pregnancy (pre-existing diabetes): retinal assessment at booking (1st trimester) and again at 28 weeks; if retinopathy at booking, add a review at 16–20 weeks.
🔎 Classification → what it means
- Background (R1): microaneurysms, dot/blot haemorrhages, hard exudates. Usually asymptomatic.
- Pre-proliferative (R2): venous beading, multiple blot haemorrhages, IRMA/cotton-wool spots = significant ischaemia.
- Proliferative (R3): new vessels at disc/elsewhere ± pre-retinal/vitreous haemorrhage → high risk of tractional detachment.
- Maculopathy (M1): macular oedema/exudates within 1 disc diameter of fovea or reduced acuity from oedema.
🚦Referral urgency (practical)
- 🔴 R3 or M1 with reduced vision: urgent same-week ophthalmology (often same-day if vitreous haemorrhage/sudden floaters or vision drop).
- 🟠 R2: prompt routine referral (weeks).
- 🟢 R1: continue annual screening; optimise risk factors.
🧰 Management
- Risk factor optimisation: individualised HbA1c target, strict BP control, statin/ACEi as indicated, smoking cessation.
- Macular oedema (centre-involving): intravitreal anti-VEGF (e.g., aflibercept/ranibizumab); steroids in selected cases.
- Proliferative retinopathy: pan-retinal photocoagulation (PRP); anti-VEGF as adjunct/bridge.
- Advanced disease: vitrectomy for non-clearing vitreous haemorrhage or tractional retinal detachment.
⚠️ Red flags (act now)
- Sudden floaters, curtain over vision, or acute vision drop → possible vitreous haemorrhage/retinal detachment → same-day eye assessment.
- Pregnancy with progressive retinopathy → expedite ophthalmology review.
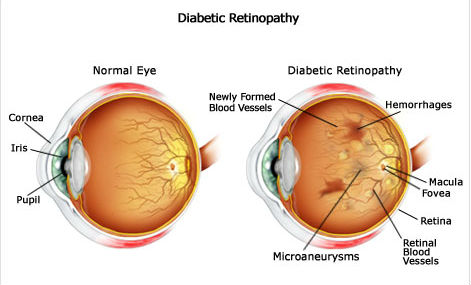
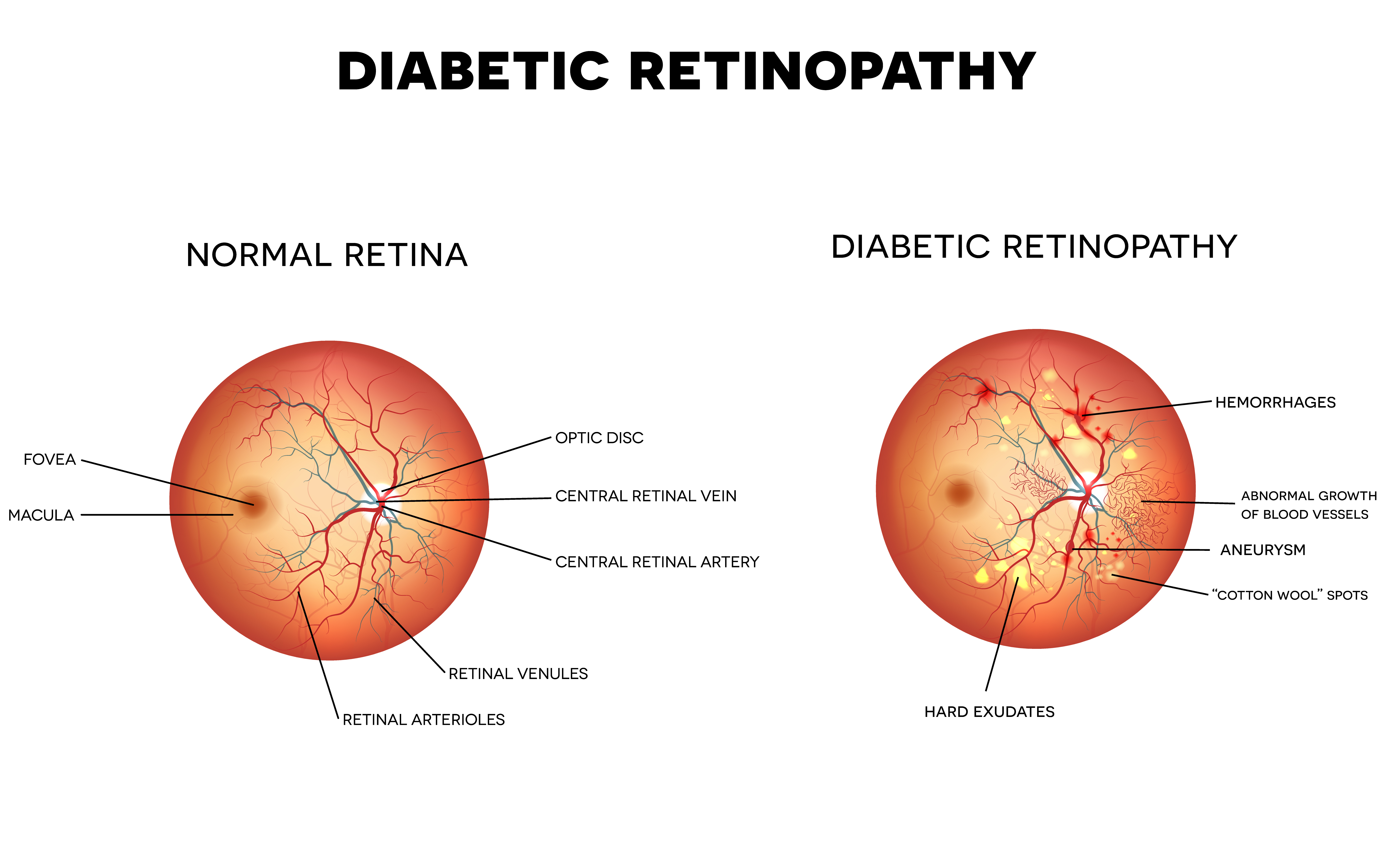
📚 Teaching diagram placeholders
🧑⚕️ Case vignette
A 58-year-old with T2D (12 yrs), HbA1c 74 mmol/mol, BP 154/92, reports mild central blur. Screening photo shows hard exudates within 1DD of the fovea and thickening on OCT. ✅ M1 maculopathy → refer urgently for anti-VEGF; tighten BP and glucose; start/optimise statin and ACEi.
💡 Mentor tip
If you remember just three things for viva: duration drives risk, VEGF links ischaemia to oedema/neovascularisation, and R3/M1 need urgent eyes-on. Everything else is risk-factor medicine.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Disease
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
