| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Long COVID
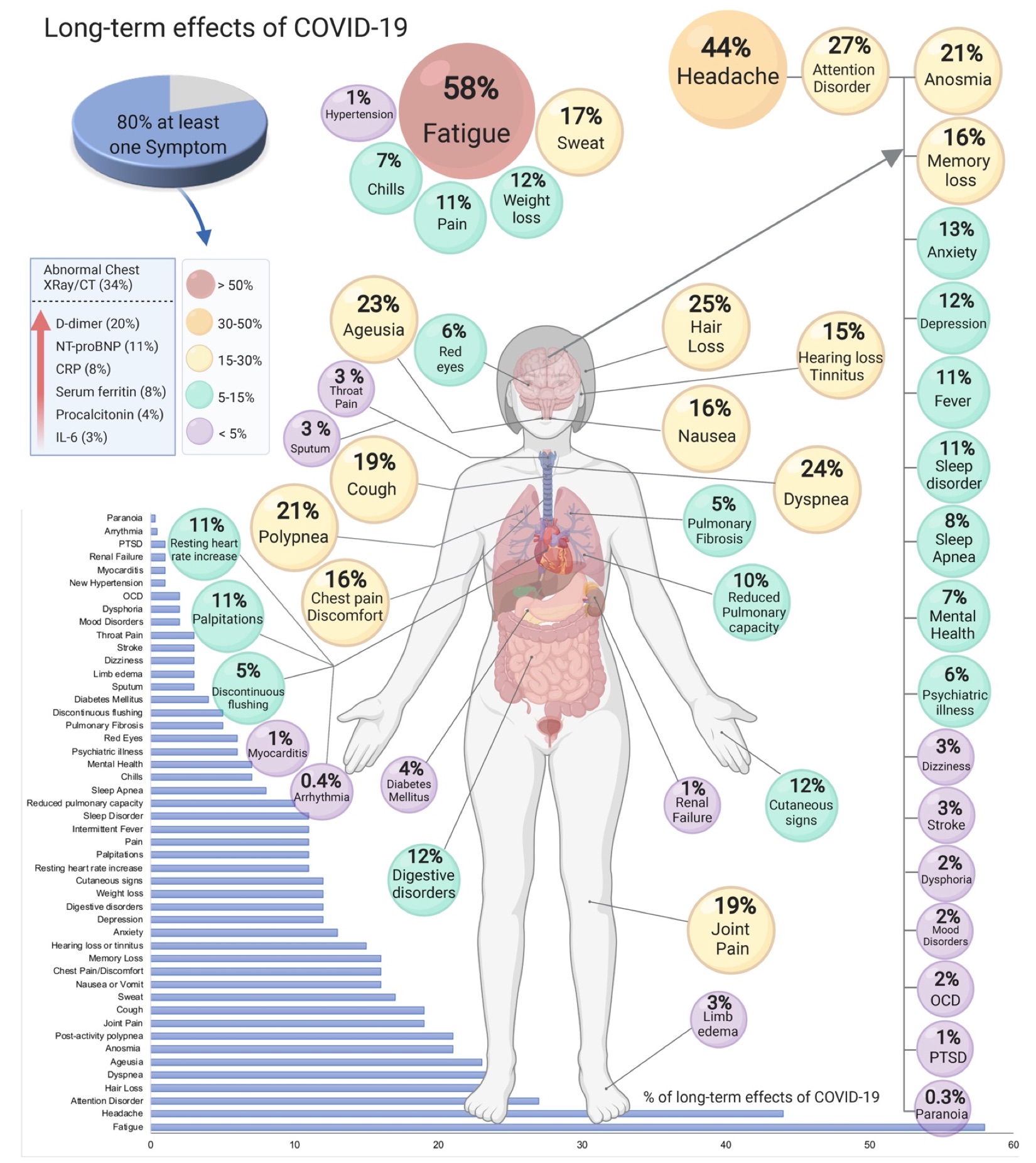
🧠 Long COVID (Post-COVID-19 condition) — persistent or new symptoms ≥12 weeks after acute infection, not explained by an alternative diagnosis. Multisystem; fluctuating course; pacing and symptom-guided rehab are central.
🗂️ One-Page Clinical Summary (no extra CSS)
| Domain | Common features | Initial approach (primary care) |
|---|---|---|
| Energy / Fatigue | Profound fatigue; post-exertional symptom exacerbation (PESE/PEM); unrefreshing sleep | 🧭 Teach pacing & energy envelope; avoid fixed graded exercise. Sleep hygiene; screen for anaemia, thyroid, B12, ferritin, HbA1c; occupational/education adjustments. |
| Breathlessness / Chest | Dyspnoea, chest tightness, cough; palpitations | Vitals incl. SpO₂; CXR (≥12 wks if persistent), ECG; consider BNP if HF symptoms; inhaler trial if variable wheeze/cough. Safety-net for red flags. |
| Neurocognitive | “Brain fog”, poor concentration, headaches, dizziness | Rule out depression, anxiety, sleep apnoea, migraine. Cognitive pacing, task chunking, screen/limit multitasking; consider work/study accommodations. |
| Autonomic / Orthostatic | Orthostatic intolerance, tachycardia (possible PoTS), temperature dysregulation | Active stand test; fluids 2–3 L/day, ↑salt if appropriate, compression stockings, slow position changes. Consider propranolol/ivabradine under specialist advice if PoTS suspected. |
| MSK / Pain | Myalgia, arthralgia, deconditioning | Gentle flexibility and symptom-contingent strengthening within energy envelope; heat/ice; simple analgesia; avoid NSAIDs if gastritis risk. |
| Mental health | Anxiety, low mood, PTSD-like symptoms | Validate; brief CBT-informed strategies; peer support; consider SSRIs/SNRIs if indicated; manage insomnia. |
| GI | Nausea, diarrhoea, abdominal pain | Hydration; low-FODMAP trial if IBS-like (short term, dietitian if possible); rule out red flags; treat reflux/IBS per guidelines. |
| ENT / Olfactory | Hyposmia/anosmia, dysgeusia | Olfactory training (twice daily, 12+ weeks); treat rhinitis/reflux if present. |
🧪 Baseline Assessment (rule out differentials)
| Tests | Why | Notes |
|---|---|---|
| FBC, U&E, LFTs, CRP, ferritin, TSH, HbA1c, B12/folate | Screen for anaemia, thyroid disease, inflammation, diabetes, deficiencies | Target correctables that mimic fatigue/brain fog |
| ECG; consider CXR (persistent respiratory symptoms ≥12 wks) | Exclude occult cardiopulmonary disease | Troponin/BNP guided by symptoms/exam |
| Urinalysis; pulse oximetry (rest/exertional) | Renal screen; exertional desaturation | 6-minute walk if safe; stop if symptomatic |
| Directed tests | Only if red flags (PE, myocarditis, new neuro deficits) | D-dimer/CTPA, echo, neuro imaging per presentation |
🛡️ Red Flags (urgent same-day assessment)
- New/worsening chest pain, syncope, resting SpO₂ <94% (or <92% in COPD) or exertional desaturation
- Focal neurology, severe new headache, confusion
- Haemoptysis, calf swelling/pleuritic pain (consider PE)
- Cardiac red flags after COVID (myocarditis/pericarditis features)
🎯 Management & Follow-up
- Education & pacing: plan-do-review diary; avoid “boom-bust”.
- Rehab: breathing control, gentle mobility, then symptom-contingent strengthening; refer to local Long COVID / pulmonary rehab services when available.
- Sleep: regular schedule, light exposure, limit naps/caffeine; consider melatonin short-term.
- Autonomic care: fluids/salt, compression, recumbent exercise start; meds via specialist if PoTS.
- Return to work/school: phased, with adjustments; provide fit note specifying limitations.
- Vaccination: associated with lower risk of developing Long COVID; keep up to date.
🧑🏫 Patient-friendly message
“Long COVID can wax and wane. Working within your energy limits, prioritising sleep, and tackling one problem at a time usually helps. We’ll rule out other causes, support your rehab, and review regularly. Seek urgent help if you develop chest pain, fainting, or new breathlessness.”
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
