| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Introduction to ECGs
Before interpreting an ECG, always confirm the basics: ✅ Correct patient name and hospital/NHS number ✅ Correct date and time ✅ Speed (usually 25 mm/s) and gain (10 mm/mV) are clearly marked ✅ Ensure the ECG is technically adequate (no major artefact, all leads visible) ✅ Always review in clinical context — symptoms, medications, electrolytes, and comparison with previous ECGs.
Normal ECG showing sinus rhythm with standard calibration.
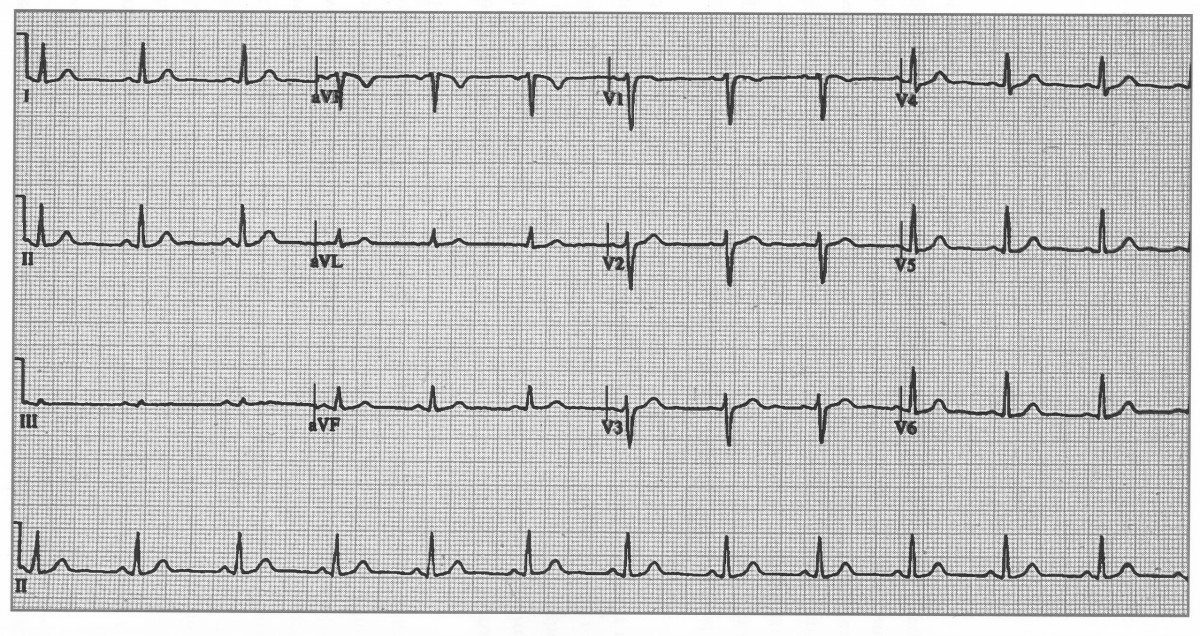
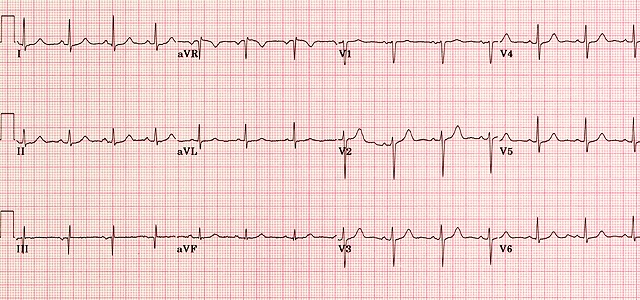
Another normal trace, demonstrating upright P waves and progressive R-wave amplitude across the precordial leads.
✅ Features of a Normal ECG
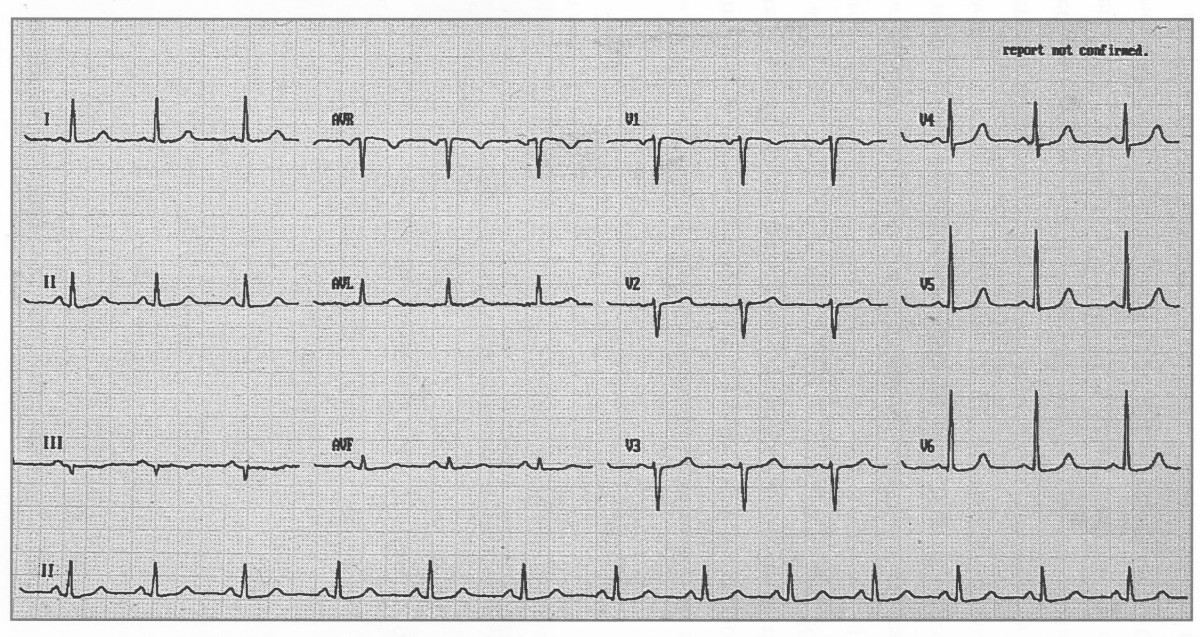
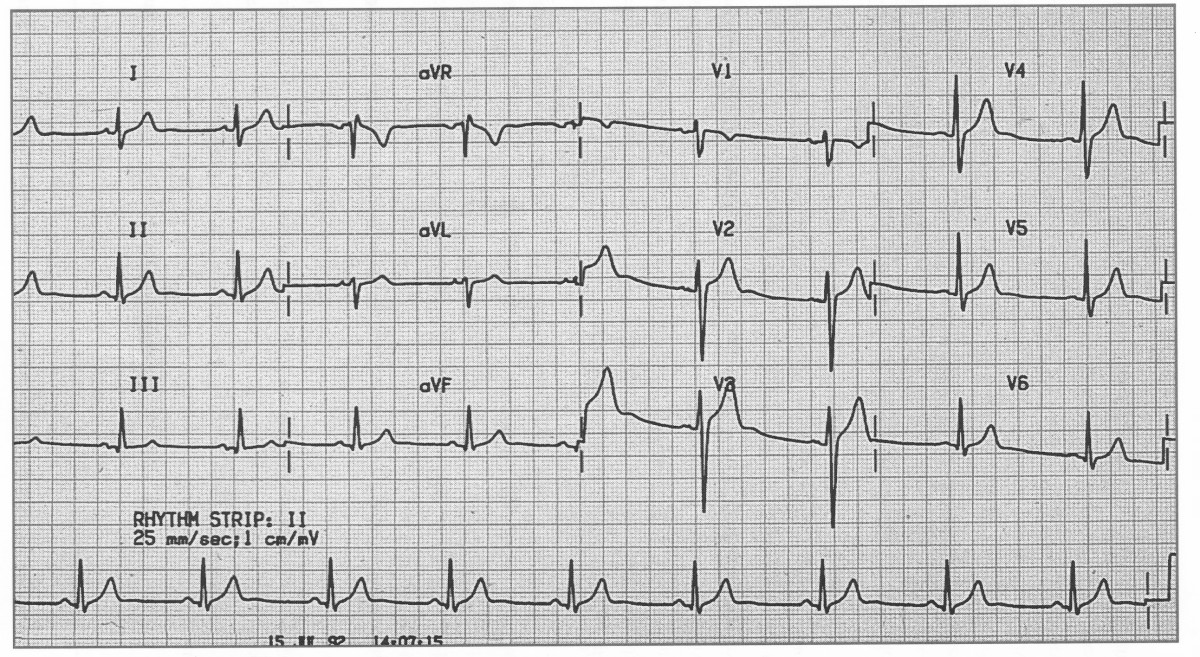
 A normal ECG (above) demonstrates regular sinus rhythm, rate around 82 bpm, and normal intervals throughout.
All deflections and segments are within physiological limits.
A normal ECG (above) demonstrates regular sinus rhythm, rate around 82 bpm, and normal intervals throughout.
All deflections and segments are within physiological limits.
🧭 Stepwise ECG Interpretation (UK Clinical Method)
Adopt a structured, reproducible approach each time you interpret an ECG:
- 👤 Check the patient details — name, date of birth, hospital/NHS number, and time recorded. Mislabelled ECGs can lead to catastrophic error.
- ⚙️ Check calibration — 25 mm/s speed and 10 mm/mV gain (1 mV = 10 mm vertically).
- 💓 Rate — Regular rhythm: 300/150/100/75/60/50 big-box method. Irregular rhythm: count QRS in 10 s ×6.
- 🔄 Rhythm — Is there a P wave before every QRS? Constant PR interval? Sinus rhythm = P upright in I, II, aVF and inverted in aVR.
- 🧭 Cardiac axis — Positive I and aVF → normal axis (−30° to +90°). I positive, aVF negative → left axis. I negative, aVF positive → right axis.
- 📏 Intervals — PR 120–200 ms; QRS ≤120 ms; QTc <440 ms (men) or <460 ms (women). Correct QT for rate (Bazett or Fridericia).
- 📊 Waves and segments — Evaluate each: P, QRS, ST, T, and U. Check morphology, amplitude, and concordance.
- 🩸 Compare — Always compare with old ECGs and correlate with symptoms and troponin results.
📏 Normal ECG Parameters
| Parameter | Normal range | Key teaching point |
|---|---|---|
| P wave | ≤110 ms, ≤2.5 mm height | Upright in I, II, aVF; biphasic in V1; negative in aVR. |
| PR interval | 120–200 ms | Prolonged = 1° AV block; short = pre-excitation. |
| QRS complex | ≤120 ms | Widened QRS = bundle branch block or ventricular rhythm. |
| QRS amplitude | >0.5 mV in limb, >1.0 mV in chest leads | High voltage → LVH; low → pericardial effusion/obesity. |
| ST segment | Isoelectric ±1 mm | Elevation/depression implies ischaemia or pericarditis. |
| T wave | Upright in I, II, V3–V6 | Inverted T may be normal in III, aVR, V1. |
| QT interval | ≤440 ms (M), ≤460 ms (F) | Prolonged QT → risk of torsades; correct for rate. |
| Axis | −30° to +90° | Left shift = LVH or inferior MI; right shift = RVH or PE. |
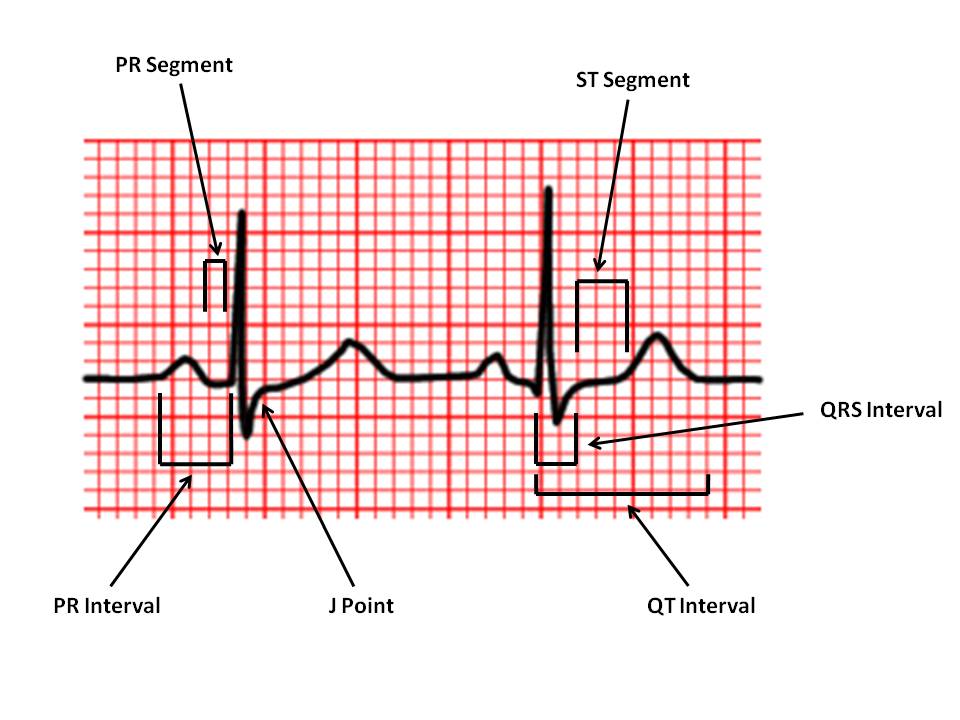
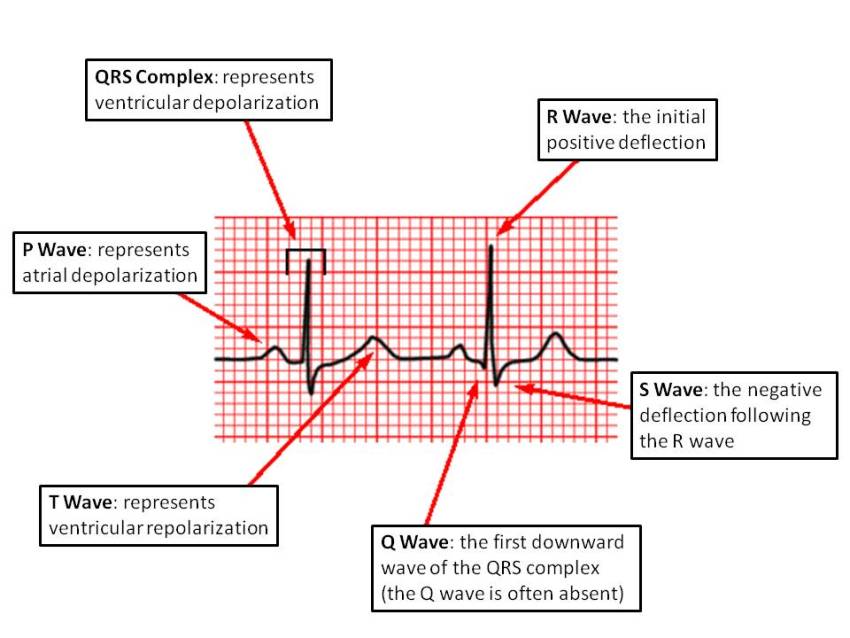
🔍 Key Waveform Components
1️⃣ P wave: Represents atrial depolarisation. Normal ≤0.11 s; smooth, rounded, upright in I, II, aVF. Bifid P = left atrial enlargement (P mitrale); peaked P = right atrial enlargement (P pulmonale).
2️⃣ PR interval: Measured from start of P to start of QRS. Normal 0.12–0.20 s. Prolonged = delayed AV conduction; short = accessory pathway (e.g. WPW).
3️⃣ QRS complex: Represents ventricular depolarisation. Normal ≤0.12 s. Look for bundle branch block patterns and R-wave progression V1→V6.
4️⃣ ST segment: Represents early ventricular repolarisation. Normally flat (isoelectric). ST ↑ > 1 mm in two contiguous leads → consider STEMI. ST ↓ > 0.5 mm → ischaemia or reciprocal change.
5️⃣ T wave: Represents ventricular repolarisation. Asymmetric, upright in most leads (except aVR, V1). Inverted T = ischaemia, strain, PE, or normal variant.
6️⃣ QT interval: Represents total ventricular depolarisation + repolarisation. Normal ≤0.44 s (M) or ≤0.46 s (F). Prolonged QT → risk of torsades (think hypokalaemia, macrolides, antipsychotics). Short QT → hypercalcaemia, digoxin effect.
⚡ Recognising Abnormal Patterns
- Ischaemia / STEMI ❤️🔥 — Localised ST elevation, reciprocal depression, new Q waves, evolving T inversion.
- Pericarditis ♨️ — Widespread concave ST elevation + PR depression; no reciprocal change.
- Hyperkalaemia 🔺 — Tall peaked T, PR prolongation, QRS widening → sine-wave.
- Hypokalaemia 🔻 — Flat T, U waves, prolonged QT.
- LVH / RVH 💪 — High voltage, strain pattern (ST depression, T inversion opposite QRS direction).
- Bundle Branch Blocks — RBBB (rsR′ V1), LBBB (broad notched R V6). LBBB + chest pain → treat as STEMI (until proven otherwise).
- PE (S1Q3T3) 🫁 — S in I, Q and T inversion in III; sinus tachycardia; right axis deviation.
🧠 Common UK Exam & OSCE Tips
- Start with: “This ECG is recorded at 25 mm/s and 10 mm/mV. It shows sinus rhythm at 78 bpm with a normal axis.”
- Describe the abnormality last, and conclude with likely cause: “…features of left ventricular hypertrophy with secondary repolarisation change, likely due to longstanding hypertension.”
- Always state the rate, rhythm, axis, intervals, and key wave/segment findings in OSCEs.
- Look for artefact, baseline wander, or poor lead placement before over-interpreting.
- Document serial ECGs — trend changes over time are diagnostically powerful. 📈
🧩 Rapid ECG Reference (Summary Card)
Checklist: ID → Calibration → Rate → Rhythm → Axis → Intervals → Morphology → ST/T → Comparison.
PR 120–200 ms • QRS ≤120 ms • QTc <440/460 ms • Axis −30°→+90° • ST isoelectric • Sinus rhythm = P upright I, II, aVF; negative aVR.
Always treat the patient, not the ECG.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
