| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Acute Inflammation
Related Subjects: | Acute Inflammation
🔥 Acute inflammation is a rapid, early defensive response of the body to harmful stimuli such as pathogens, damaged cells, or irritants. It is characterised by the classical signs of ➡️ heat, redness, swelling, pain, and loss of function. Its main purposes are to eliminate the cause of injury, remove necrotic debris, and initiate tissue repair.
🔄 Stages of Acute Inflammation
- 1. Initiation 🛎️ :
- Recognition of harmful stimuli via pattern recognition receptors (PRRs) on immune cells.
- Release of inflammatory mediators such as histamine, prostaglandins, cytokines.
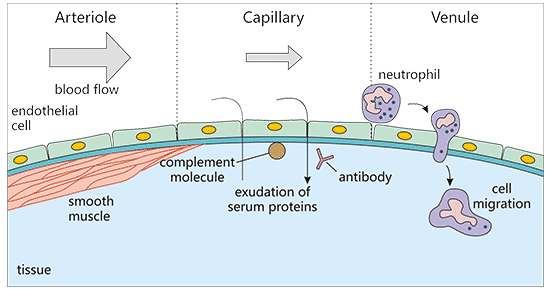
- 2. Vascular Changes 💉 :
- Vasodilation: Increased blood flow → redness & heat.
- Increased vascular permeability: Plasma proteins & fluid leak into tissues → oedema (swelling).
- 3. Cellular Events 🧑⚕️🦠 :
- Leukocyte recruitment: Margination → rolling → adhesion → transmigration (diapedesis).
- Phagocytosis: Neutrophils & macrophages engulf debris → fuse phagosome with lysosome → destruction by ROS & enzymes.
🧪 Chemical Mediators of Inflammation
- Vasoactive Amines ⚡ :
- Histamine: Mast cells, basophils, platelets → vasodilation & permeability.
- Serotonin: Platelets & enterochromaffin cells → similar vascular effects.
- Plasma Protein Systems 🩸 :
- Complement (C3a, C5a): Anaphylatoxins → permeability & chemotaxis. C3b acts as an opsonin.
- Coagulation: Fibrin meshwork forms a clot scaffold.
- Kinin system: Bradykinin → vasodilation, pain, permeability.
- Arachidonic Acid Metabolites 🌀 :
- Prostaglandins (COX): Pain, vasodilation, fever.
- Leukotrienes (LOX): Chemotaxis, permeability, bronchospasm.
- Cytokines & Chemokines 📢 :
- TNF, IL-1: Fever, adhesion molecules, systemic acute phase response.
- Chemokines: Recruit leukocytes to the site.
- ROS & Nitric Oxide ⚔️ :
- Microbicidal and signalling roles.
- Excess = tissue injury (ARDS, reperfusion injury).
🧭 Outcomes of Acute Inflammation
- ✅ Resolution: Full clearance & return to normal tissue.
- 💥 Abscess: Localised pus collection when clearance fails.
- ♻️ Chronic inflammation: If stimulus persists → fibrosis & immune activation.
- 🧱 Fibrosis/scarring: When tissue repair is incomplete.
🩺 Clinical Signs & Symptoms ("Cardinal Signs")
- 🔴 Redness (Rubor): Vasodilation, hyperaemia.
- 🔥 Heat (Calor): Increased blood flow & metabolic activity.
- 💧 Swelling (Tumour): Oedema from plasma leakage.
- 😣 Pain (Dolor): Mediated by bradykinin, prostaglandins, pressure effects.
- ⚠️ Loss of Function (Functio Laesa): Pain & swelling limiting use.
📚 Clinical Relevance
- Fever in systemic inflammation is driven by IL-1 & TNF acting on the hypothalamus.
- Raised CRP & ESR are acute phase reactants produced by the liver.
- Uncontrolled acute inflammation can → sepsis, SIRS, or chronic inflammation (e.g. Crohn’s, RA).
📝 Summary
Acute inflammation is an essential protective response, aimed at eliminating harmful agents and initiating repair. It integrates vascular changes, leukocyte activity, and chemical mediators. ⚖️ While vital, if unchecked it can cause collateral tissue injury or evolve into chronic disease.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
